Monday Poster Session
Category: Infections and Microbiome
P3463 - Fowl Play in the Gut: A Case of Spirochetosis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Marie Balfour, MD (she/her/hers)
University of California Irvine Health
Orange, CA
Presenting Author(s)
Marie Balfour, MD1, Nicholas Garcia, MD1, Amirali Tavangar, MD2, Kamran Urgun, MD3, Suvarna A. Deshmukh-Rane, MD3, Vidya Atluri, MD3, Mark Salem, MD3, Peter H. Nguyen, MD1
1University of California Irvine Health, Orange, CA; 2University of California Irvine Digestive Health Institute, Orange, CA; 3Tibor Rubin Veterans Affairs Medical Center, Long Beach, CA
Introduction: Intestinal spirochetosis (IS) is a rare infection that is characterized by attachment of Brachyspira spirochetes to the epithelial brush border. This results in impairment of water and electrolyte absorption and manifests as abdominal pain, altered bowel habits, and chronic diarrhea. While the incidence is low, it is more common in children, immunocompromised patients, and patients exposed to human or animal feces or contaminated water.
Case Description/
Methods: We describe a case of a patient found to have IS despite minimal risk factors, highlighting the importance of considering spirochetosis in a differential for chronic diarrhea. A 31-year-old male with past medical history of anxiety presented with intermittent watery diarrhea for the past year and left lower quadrant abdominal pain. Previous stool cultures from 4 months prior were positive for Enteropathogenic Escherichia coli (EPEC) and norovirus. Given the persistence of symptoms, the patient underwent a colonoscopy, which was overall grossly normal. Random biopsies were taken of the colon and were significant for intestinal spirochetosis in all biopsies with spirochete immunostaining highlighting numerous immunostain-positive organisms attached to the surface of epithelial cells without invasion. The patient’s sexual history was unremarkable and HIV testing was negative. However, the patient did report exposure to chickens as his sister has a chicken coop that he visited several times the previous year, and he also owns a dog. The patient’s symptoms initially improved after completing a 10-day course of metronidazole. He returned to clinic with recurrent diarrhea 4 months after his initial colonoscopy and is scheduled to undergo a repeat colonoscopy.
Discussion: This case highlights the diagnostic challenge of intestinal spirochetosis as its presentation overlaps with functional, autoimmune, and infectious gastrointestinal pathologies. The patient’s prior exposure to chickens and pet dog poses his only risk factors for IS, underscoring the need for a thorough clinical and social history. The gold standard for diagnosis remains colonic biopsy. While there are no standard guidelines for treating IS and its presence may not always be pathologic, metronidazole is the recommended antibiotic. If symptoms persist, it is recommended to repeat a colonoscopy to evaluate if spirochetes are still present in the epithelium. Recurrence is rare but can be treated with repeat courses of metronidazole.
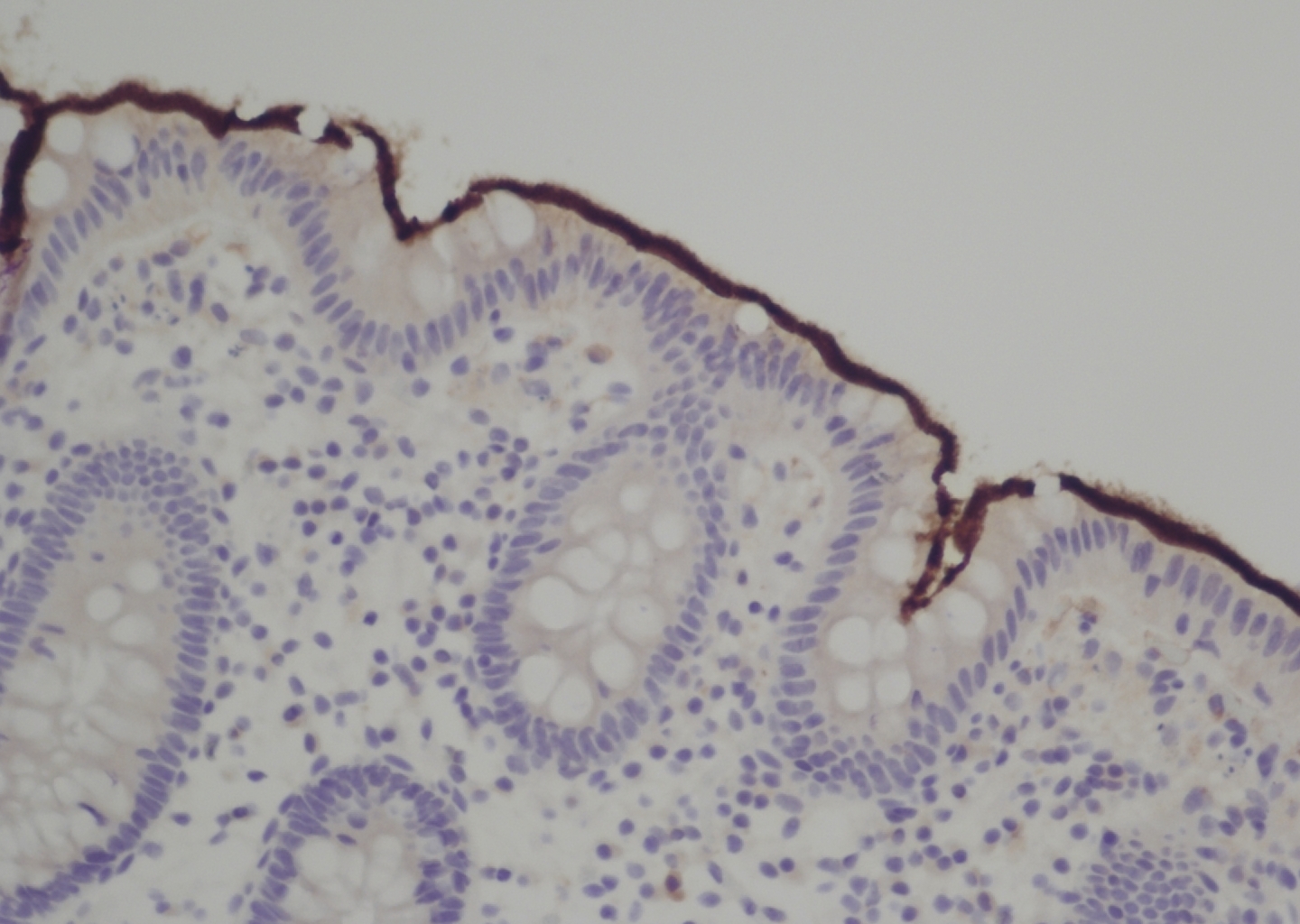
Figure: Figure 1: Colon biopsy demonstrating positive Spirochete immunostaining (dark brown stain) along the apical surface of the epithelium
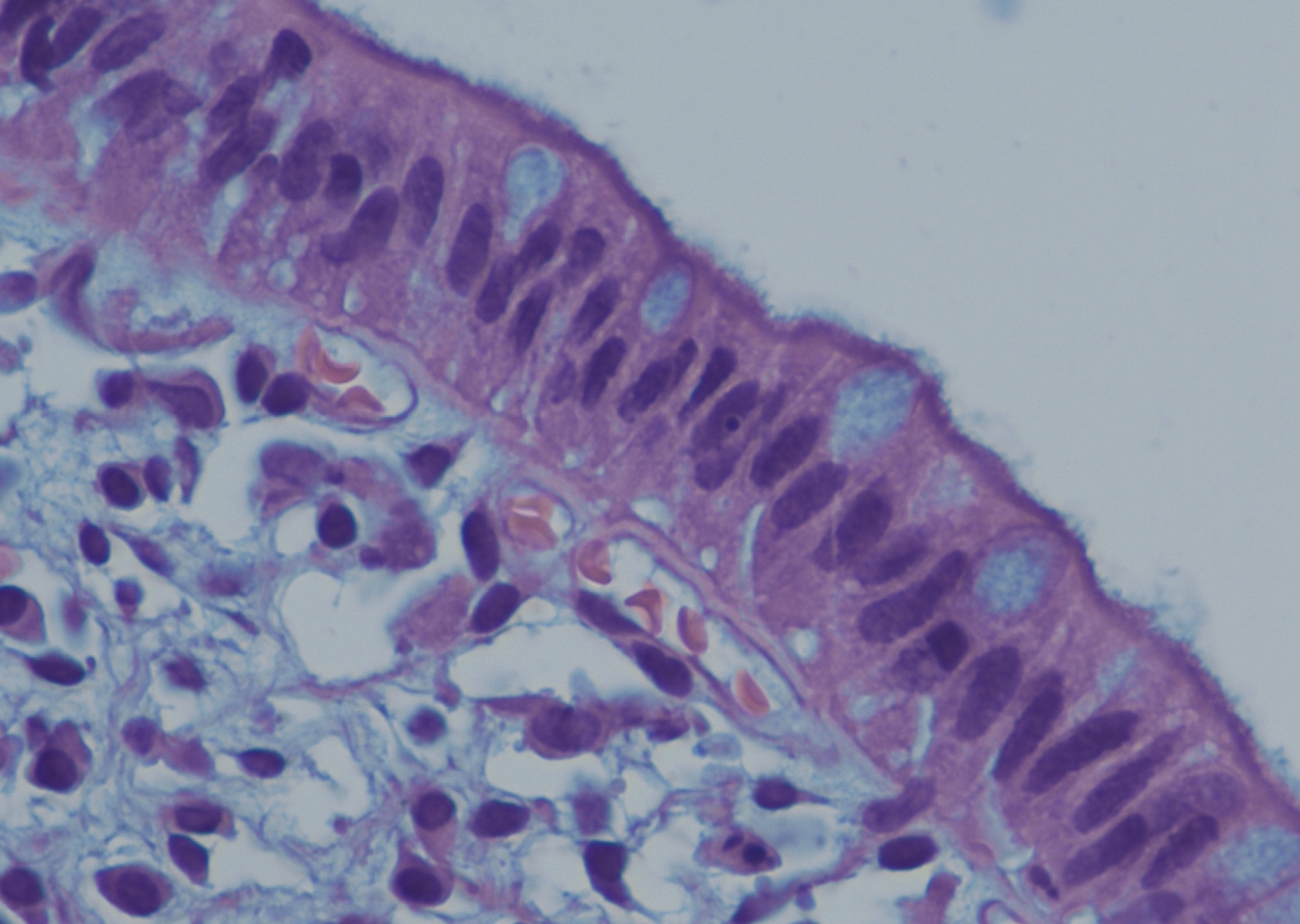
Figure: Figure 2: H&E slide demonstrating Brachyspira colonization denoted by the basophilic (blue) fringe along the epithelium which can be referred to as a “false brush border”
Disclosures:
Marie Balfour indicated no relevant financial relationships.
Nicholas Garcia indicated no relevant financial relationships.
Amirali Tavangar indicated no relevant financial relationships.
Kamran Urgun indicated no relevant financial relationships.
Suvarna Deshmukh-Rane indicated no relevant financial relationships.
Vidya Atluri indicated no relevant financial relationships.
Mark Salem indicated no relevant financial relationships.
Peter Nguyen indicated no relevant financial relationships.
Marie Balfour, MD1, Nicholas Garcia, MD1, Amirali Tavangar, MD2, Kamran Urgun, MD3, Suvarna A. Deshmukh-Rane, MD3, Vidya Atluri, MD3, Mark Salem, MD3, Peter H. Nguyen, MD1. P3463 - Fowl Play in the Gut: A Case of Spirochetosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of California Irvine Health, Orange, CA; 2University of California Irvine Digestive Health Institute, Orange, CA; 3Tibor Rubin Veterans Affairs Medical Center, Long Beach, CA
Introduction: Intestinal spirochetosis (IS) is a rare infection that is characterized by attachment of Brachyspira spirochetes to the epithelial brush border. This results in impairment of water and electrolyte absorption and manifests as abdominal pain, altered bowel habits, and chronic diarrhea. While the incidence is low, it is more common in children, immunocompromised patients, and patients exposed to human or animal feces or contaminated water.
Case Description/
Methods: We describe a case of a patient found to have IS despite minimal risk factors, highlighting the importance of considering spirochetosis in a differential for chronic diarrhea. A 31-year-old male with past medical history of anxiety presented with intermittent watery diarrhea for the past year and left lower quadrant abdominal pain. Previous stool cultures from 4 months prior were positive for Enteropathogenic Escherichia coli (EPEC) and norovirus. Given the persistence of symptoms, the patient underwent a colonoscopy, which was overall grossly normal. Random biopsies were taken of the colon and were significant for intestinal spirochetosis in all biopsies with spirochete immunostaining highlighting numerous immunostain-positive organisms attached to the surface of epithelial cells without invasion. The patient’s sexual history was unremarkable and HIV testing was negative. However, the patient did report exposure to chickens as his sister has a chicken coop that he visited several times the previous year, and he also owns a dog. The patient’s symptoms initially improved after completing a 10-day course of metronidazole. He returned to clinic with recurrent diarrhea 4 months after his initial colonoscopy and is scheduled to undergo a repeat colonoscopy.
Discussion: This case highlights the diagnostic challenge of intestinal spirochetosis as its presentation overlaps with functional, autoimmune, and infectious gastrointestinal pathologies. The patient’s prior exposure to chickens and pet dog poses his only risk factors for IS, underscoring the need for a thorough clinical and social history. The gold standard for diagnosis remains colonic biopsy. While there are no standard guidelines for treating IS and its presence may not always be pathologic, metronidazole is the recommended antibiotic. If symptoms persist, it is recommended to repeat a colonoscopy to evaluate if spirochetes are still present in the epithelium. Recurrence is rare but can be treated with repeat courses of metronidazole.
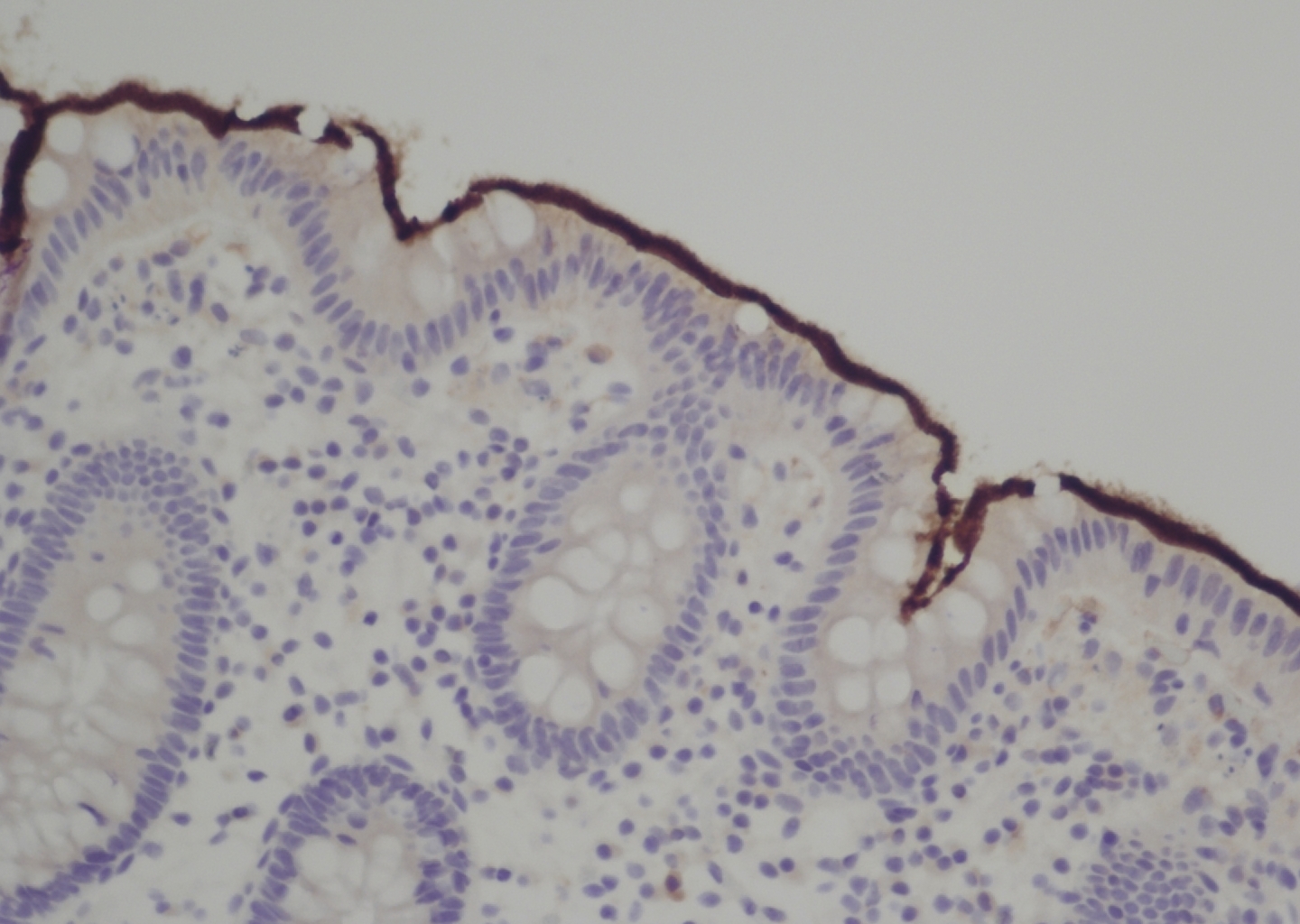
Figure: Figure 1: Colon biopsy demonstrating positive Spirochete immunostaining (dark brown stain) along the apical surface of the epithelium
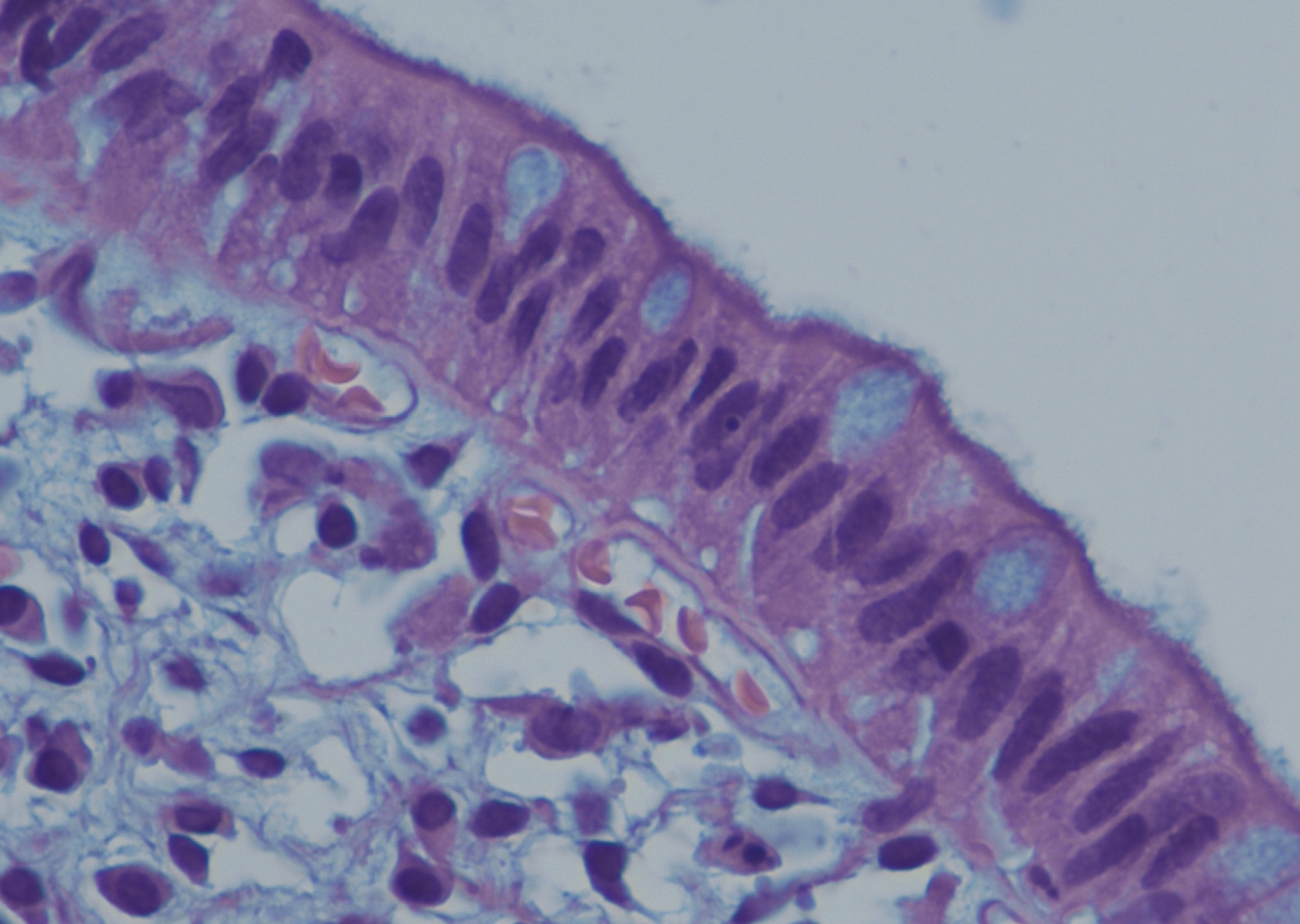
Figure: Figure 2: H&E slide demonstrating Brachyspira colonization denoted by the basophilic (blue) fringe along the epithelium which can be referred to as a “false brush border”
Disclosures:
Marie Balfour indicated no relevant financial relationships.
Nicholas Garcia indicated no relevant financial relationships.
Amirali Tavangar indicated no relevant financial relationships.
Kamran Urgun indicated no relevant financial relationships.
Suvarna Deshmukh-Rane indicated no relevant financial relationships.
Vidya Atluri indicated no relevant financial relationships.
Mark Salem indicated no relevant financial relationships.
Peter Nguyen indicated no relevant financial relationships.
Marie Balfour, MD1, Nicholas Garcia, MD1, Amirali Tavangar, MD2, Kamran Urgun, MD3, Suvarna A. Deshmukh-Rane, MD3, Vidya Atluri, MD3, Mark Salem, MD3, Peter H. Nguyen, MD1. P3463 - Fowl Play in the Gut: A Case of Spirochetosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
