Monday Poster Session
Category: Infections and Microbiome
P3433 - Epidemiology of Diarrheal Infections in Patients With HIV Infection Before and After Gastrointestinal Panel Testing
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Michelle E. Lee, MD
NewYork-Presbyterian / Weill Cornell Medical Center
New York, NY
Presenting Author(s)
Michelle E. Lee, MD1, Catherine Ng, MS1, Ying Li, MS2, Carl V. Crawford, MD1, Harjot K.. Singh, MD1
1NewYork-Presbyterian / Weill Cornell Medical Center, New York, NY; 2NewYork-Presbyterian / Weill Cornell Medicine, New York, NY
Introduction: Diarrhea in patients with HIV is associated with increased mortality. Our understanding of diarrheal pathogens has relied on older stool culture and ova and parasite studies, and limited data exist on the epidemiology since the implementation of the gastrointestinal polymerase chain reaction (GI PCR) test. In June 2016, the Weill Cornell Medicine laboratory implemented a GI PCR Panel that tests for the 22 most common pathogens in the United States. This study evaluates the epidemiology of diarrhea among patients with HIV before and after the GI PCR implementation.
Methods: This retrospective study from 6/1/2011-6/1/2021 included patients 18 years with HIV infection who had at least one diarrheal stool test: GI PCR, C. difficile, stool culture, ova and parasite, Giardia or Cryptosporidium direct fluorescent antibody (DFA), rotavirus antigen, norovirus PCR, and/or stains for Microsporidia. Demographics, HIV parameters, and hospitalization data were collected and summarized with descriptive statistics. Patients were compared by CD4 count using Wilcoxon rank sum, Pearson’s chi-square or Fisher’s exact test.
Results: Among 1830 patients with HIV infection who had stool testing, the average age was 50 years at the time of diarrheal episode and about 80% were male (Table 1). 32% of patients reported their sexual orientation as lesbian or gay. Stool testing was more common inpatient prior to June 2016, and more outpatient after 2016. Before implementation of GI PCR, patients had an average of 1.9 stool tests versus 28.8 tests after. Of 40,682 tests, 1509 pathogens were detected: 1042 bacteria, 281 viruses, and 186 parasites (Table 2). C. difficile, Enteropathogenic and Enteroaggregative E. coli, norovirus, and Shigella were the most common pathogens. After June 2016, patients with CD4< 200 mL were more likely to have norovirus and sapovirus and those with CD4³200 were more likely to have Giardia.
Discussion: The implementation of GI PCR resulted in an increase in diarrheal pathogen detection. Enteropathogenic E. coli was the most common pathogen after 2016 and C. difficile which was the most common pathogen before 2016. Giardia was more commonly identified than Cryptosporidium, which was previously reported as the most common parasitic cause of diarrhea in patients with HIV. Understanding the wide distribution of pathogens is important and can inform empiric treatment in this population.
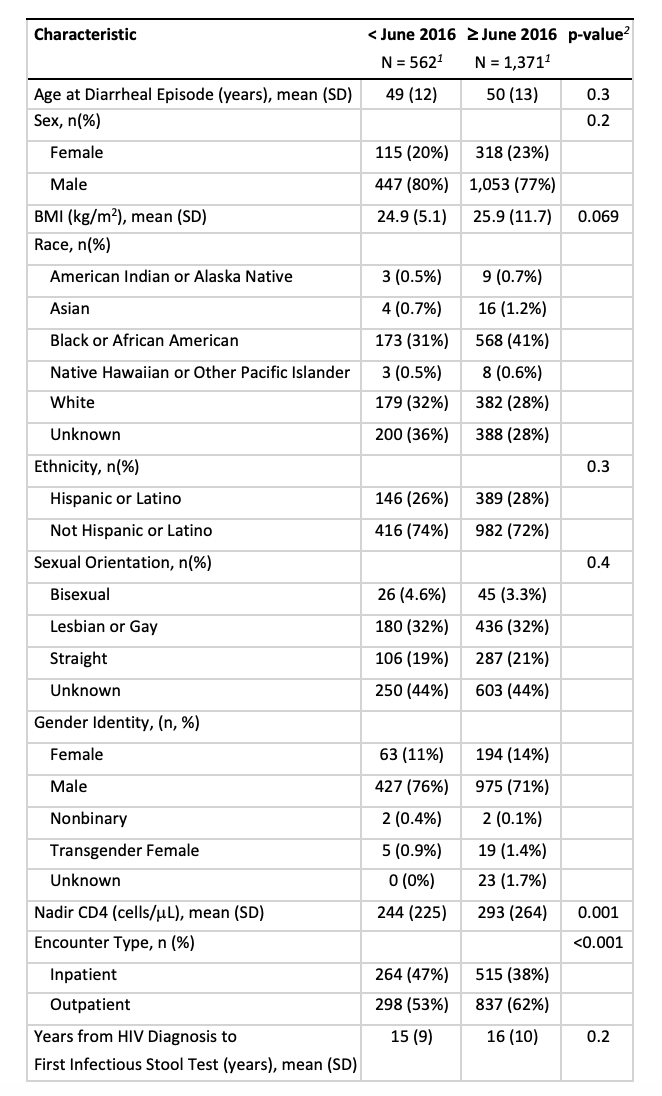
Figure: Table 1. Characteristics of Patients with HIV Tested for Diarrheal Pathogens Before and After GI Panel Implementation
1. 163 patients with infectious diarrhea testing both before and after June 2016
2. Wilcoxon rank sum test; Pearson's Chi-squared test
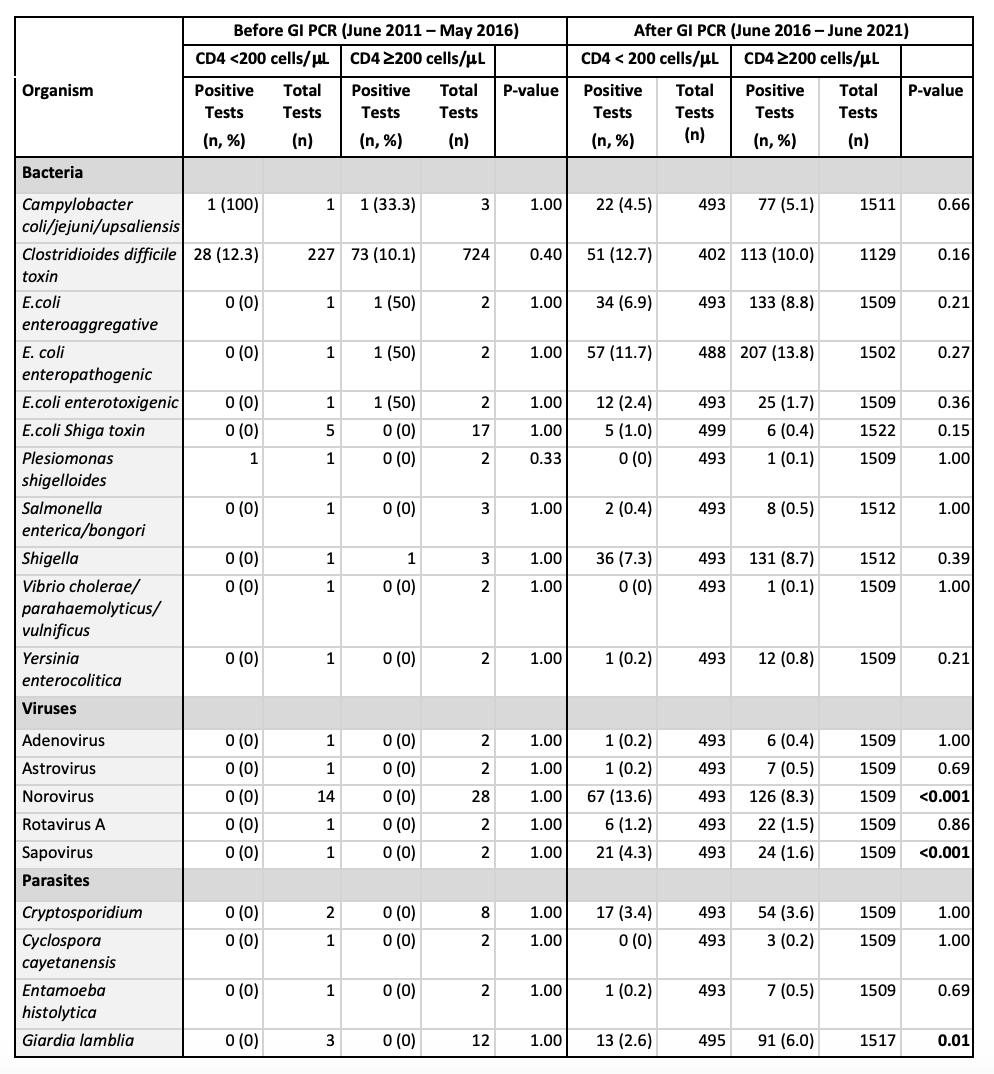
Figure: Table 2. Pathogens Detected Before and After GI Panel Implementation
Disclosures:
Michelle Lee indicated no relevant financial relationships.
Catherine Ng indicated no relevant financial relationships.
Ying Li indicated no relevant financial relationships.
Carl Crawford: Ferring – Advisor or Review Panel Member, Consultant, Grant/Research Support, Speakers Bureau. lumen – Grant/Research Support. nestle – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Phathom – Speakers Bureau. vedanta – Grant/Research Support.
Harjot Singh indicated no relevant financial relationships.
Michelle E. Lee, MD1, Catherine Ng, MS1, Ying Li, MS2, Carl V. Crawford, MD1, Harjot K.. Singh, MD1. P3433 - Epidemiology of Diarrheal Infections in Patients With HIV Infection Before and After Gastrointestinal Panel Testing, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1NewYork-Presbyterian / Weill Cornell Medical Center, New York, NY; 2NewYork-Presbyterian / Weill Cornell Medicine, New York, NY
Introduction: Diarrhea in patients with HIV is associated with increased mortality. Our understanding of diarrheal pathogens has relied on older stool culture and ova and parasite studies, and limited data exist on the epidemiology since the implementation of the gastrointestinal polymerase chain reaction (GI PCR) test. In June 2016, the Weill Cornell Medicine laboratory implemented a GI PCR Panel that tests for the 22 most common pathogens in the United States. This study evaluates the epidemiology of diarrhea among patients with HIV before and after the GI PCR implementation.
Methods: This retrospective study from 6/1/2011-6/1/2021 included patients 18 years with HIV infection who had at least one diarrheal stool test: GI PCR, C. difficile, stool culture, ova and parasite, Giardia or Cryptosporidium direct fluorescent antibody (DFA), rotavirus antigen, norovirus PCR, and/or stains for Microsporidia. Demographics, HIV parameters, and hospitalization data were collected and summarized with descriptive statistics. Patients were compared by CD4 count using Wilcoxon rank sum, Pearson’s chi-square or Fisher’s exact test.
Results: Among 1830 patients with HIV infection who had stool testing, the average age was 50 years at the time of diarrheal episode and about 80% were male (Table 1). 32% of patients reported their sexual orientation as lesbian or gay. Stool testing was more common inpatient prior to June 2016, and more outpatient after 2016. Before implementation of GI PCR, patients had an average of 1.9 stool tests versus 28.8 tests after. Of 40,682 tests, 1509 pathogens were detected: 1042 bacteria, 281 viruses, and 186 parasites (Table 2). C. difficile, Enteropathogenic and Enteroaggregative E. coli, norovirus, and Shigella were the most common pathogens. After June 2016, patients with CD4< 200 mL were more likely to have norovirus and sapovirus and those with CD4³200 were more likely to have Giardia.
Discussion: The implementation of GI PCR resulted in an increase in diarrheal pathogen detection. Enteropathogenic E. coli was the most common pathogen after 2016 and C. difficile which was the most common pathogen before 2016. Giardia was more commonly identified than Cryptosporidium, which was previously reported as the most common parasitic cause of diarrhea in patients with HIV. Understanding the wide distribution of pathogens is important and can inform empiric treatment in this population.
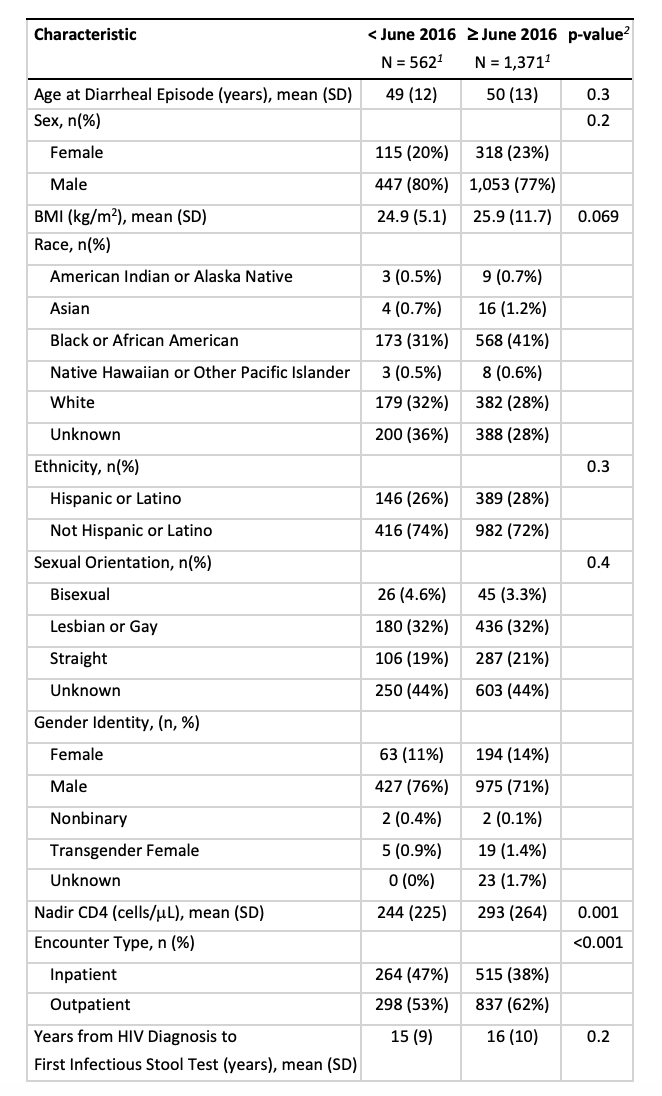
Figure: Table 1. Characteristics of Patients with HIV Tested for Diarrheal Pathogens Before and After GI Panel Implementation
1. 163 patients with infectious diarrhea testing both before and after June 2016
2. Wilcoxon rank sum test; Pearson's Chi-squared test
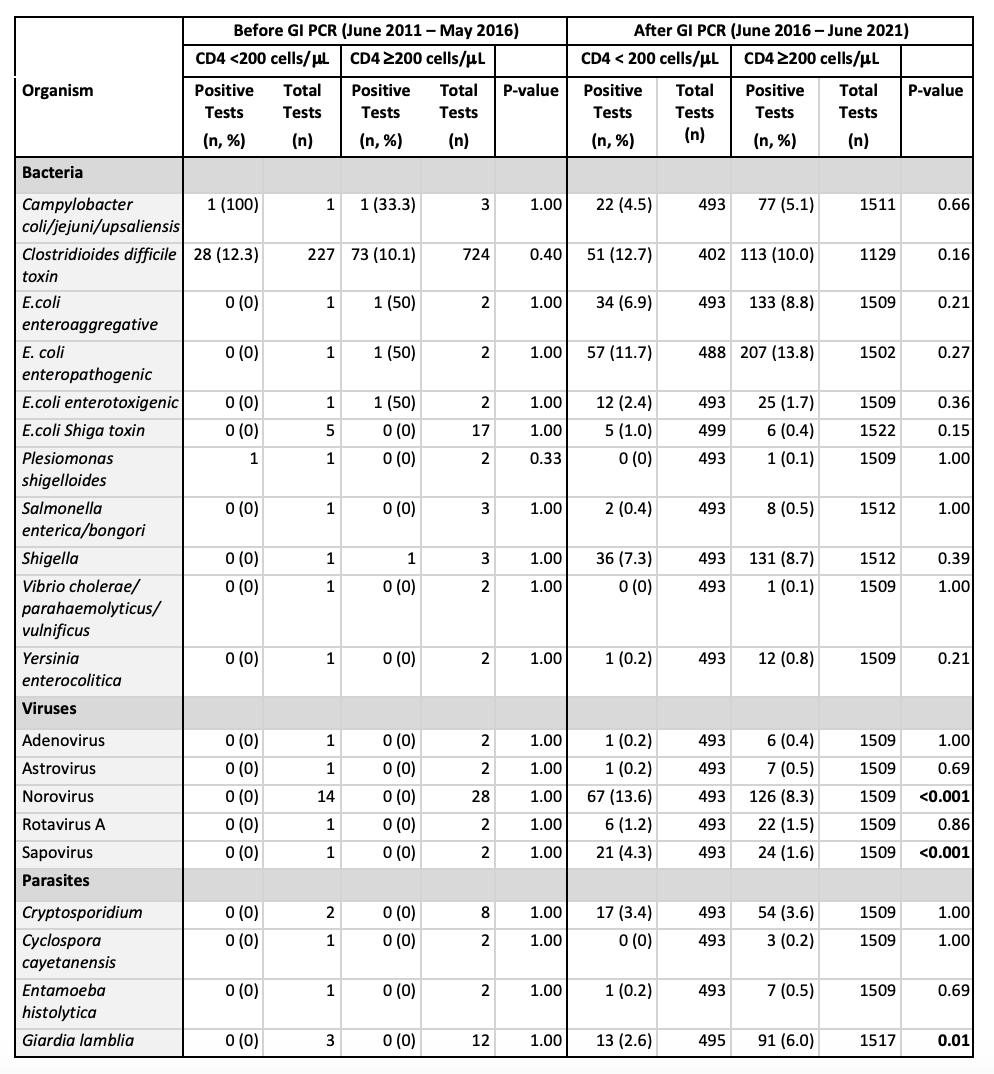
Figure: Table 2. Pathogens Detected Before and After GI Panel Implementation
Disclosures:
Michelle Lee indicated no relevant financial relationships.
Catherine Ng indicated no relevant financial relationships.
Ying Li indicated no relevant financial relationships.
Carl Crawford: Ferring – Advisor or Review Panel Member, Consultant, Grant/Research Support, Speakers Bureau. lumen – Grant/Research Support. nestle – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Phathom – Speakers Bureau. vedanta – Grant/Research Support.
Harjot Singh indicated no relevant financial relationships.
Michelle E. Lee, MD1, Catherine Ng, MS1, Ying Li, MS2, Carl V. Crawford, MD1, Harjot K.. Singh, MD1. P3433 - Epidemiology of Diarrheal Infections in Patients With HIV Infection Before and After Gastrointestinal Panel Testing, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
