Monday Poster Session
Category: IBD
P3401 - Conservative Management at What Cost?: Trans-Prostate Ileourethral Fistula in Crohn’s Disease Post-Ileal Pouch-Anal Anastomosis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Robert Graham Ferguson, IV, MD, MPH (he/him/his)
AU/UGA Medical Partnership
Athens, GA
Presenting Author(s)
Award: ACG Presidential Poster Award
Robert Graham. Ferguson, MD, MPH1, Vinod Jeyaretnam, DO1, Carla Erb, DO1, Gregory Smith, MD2
1AU/UGA Medical Partnership, Athens, GA; 2Athens Gastroenterology Center, Athens, GA
Introduction: Entero-urinary (GI-GU) fistulae are a rare complication of Crohn’s disease, occurring in 1.6% of patients. However, ileourethral fistulae are exceedingly rare, with urethral fistulae only previously documented to originate from the rectum. Herein, we present the first reported case of a prostate-traversing ileourethral fistula in a young male with Crohn’s disease, where conservative management was prolonged for nearly 2 years before surgical diversion was pursued.
Case Description/
Methods: A 33-year-old male with Crohn’s disease presented with fecaluria and pneumaturia. He had previously undergone a proctocolectomy with ileal pouch-anal anastomosis (IPAA) at age 24 and started risankizumab-rzaa. A previous CT revealed a fistula between the ileal J-pouch and central prostate; colonoscopy had been unremarkable. Repeat imaging, including MRI, revealed a 2.5 cm long, 5 mm diameter fistulous tract communicating from the left aspect of the membranous urethra to the ileal pouch containing fecal material. Cystoscopy showed fecal contents emerging through the fistulous opening in the membranous tract. Pouchoscopy revealed healthy ileal pouch mucosa with a fistula at the verge of the rectal cuff with friable mucosa (cryptitis on pathology). Conservative management, including several antibiotic regimens and Foley, was trialed for nearly 2 years, but symptoms persisted. Finally, a diverting loop ileostomy was performed, resulting in overall improvement of symptoms.
Discussion: To our knowledge, this is the first reported case of a trans-prostatic ileourethral fistula. GI-GU fistulae typically originate in the ileum (64%) and terminate in the bladder (88%), while urethral exit is seen in only 6% of GI-GU fistulae. However, urethral fistulae have only been documented to communicate with the rectum. This patient with an IPAA and an ileourethral fistula suggests that anatomical location is a major factor in formation of fistulae to the urethra. Furthermore, this case underscores the limited utility of conservative therapy as nearly 2 years of antibiotics and catheterization failed to treat the fistula. Surgical diversion ultimately led to symptom improvement, aligning with existing recommendations for surgical correction. Previous studies show biologic therapy, primarily anti-TNF agents, results in sustained closure of fistula in < 20% of cases, antibiotics alone achieve closure in 1.3% of cases, and spontaneous closure of fistula from urethral catheterization occurs in isolated cases.
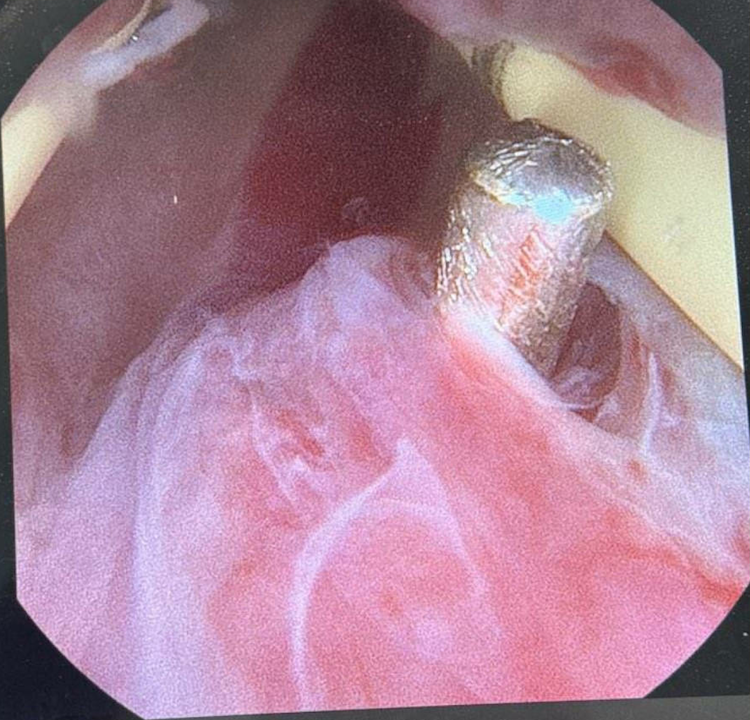
Figure: Figure 1. Ileal opening of ileourethral fistula
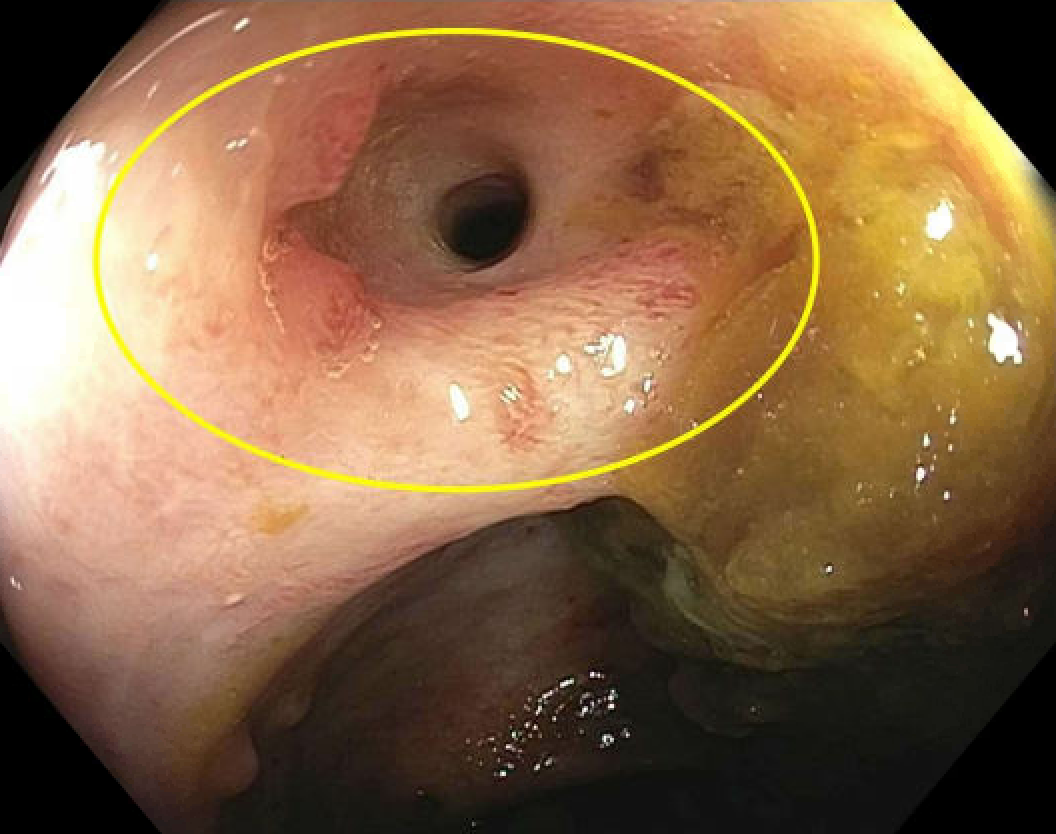
Figure: Figure 2. Urethral opening of ileourethral fistula
Disclosures:
Robert Ferguson indicated no relevant financial relationships.
Vinod Jeyaretnam: Bristol Meyers Squibb – Stock-publicly held company(excluding mutual/index funds).
Carla Erb indicated no relevant financial relationships.
Gregory Smith indicated no relevant financial relationships.
Robert Graham. Ferguson, MD, MPH1, Vinod Jeyaretnam, DO1, Carla Erb, DO1, Gregory Smith, MD2. P3401 - Conservative Management at What Cost?: Trans-Prostate Ileourethral Fistula in Crohn’s Disease Post-Ileal Pouch-Anal Anastomosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Robert Graham. Ferguson, MD, MPH1, Vinod Jeyaretnam, DO1, Carla Erb, DO1, Gregory Smith, MD2
1AU/UGA Medical Partnership, Athens, GA; 2Athens Gastroenterology Center, Athens, GA
Introduction: Entero-urinary (GI-GU) fistulae are a rare complication of Crohn’s disease, occurring in 1.6% of patients. However, ileourethral fistulae are exceedingly rare, with urethral fistulae only previously documented to originate from the rectum. Herein, we present the first reported case of a prostate-traversing ileourethral fistula in a young male with Crohn’s disease, where conservative management was prolonged for nearly 2 years before surgical diversion was pursued.
Case Description/
Methods: A 33-year-old male with Crohn’s disease presented with fecaluria and pneumaturia. He had previously undergone a proctocolectomy with ileal pouch-anal anastomosis (IPAA) at age 24 and started risankizumab-rzaa. A previous CT revealed a fistula between the ileal J-pouch and central prostate; colonoscopy had been unremarkable. Repeat imaging, including MRI, revealed a 2.5 cm long, 5 mm diameter fistulous tract communicating from the left aspect of the membranous urethra to the ileal pouch containing fecal material. Cystoscopy showed fecal contents emerging through the fistulous opening in the membranous tract. Pouchoscopy revealed healthy ileal pouch mucosa with a fistula at the verge of the rectal cuff with friable mucosa (cryptitis on pathology). Conservative management, including several antibiotic regimens and Foley, was trialed for nearly 2 years, but symptoms persisted. Finally, a diverting loop ileostomy was performed, resulting in overall improvement of symptoms.
Discussion: To our knowledge, this is the first reported case of a trans-prostatic ileourethral fistula. GI-GU fistulae typically originate in the ileum (64%) and terminate in the bladder (88%), while urethral exit is seen in only 6% of GI-GU fistulae. However, urethral fistulae have only been documented to communicate with the rectum. This patient with an IPAA and an ileourethral fistula suggests that anatomical location is a major factor in formation of fistulae to the urethra. Furthermore, this case underscores the limited utility of conservative therapy as nearly 2 years of antibiotics and catheterization failed to treat the fistula. Surgical diversion ultimately led to symptom improvement, aligning with existing recommendations for surgical correction. Previous studies show biologic therapy, primarily anti-TNF agents, results in sustained closure of fistula in < 20% of cases, antibiotics alone achieve closure in 1.3% of cases, and spontaneous closure of fistula from urethral catheterization occurs in isolated cases.
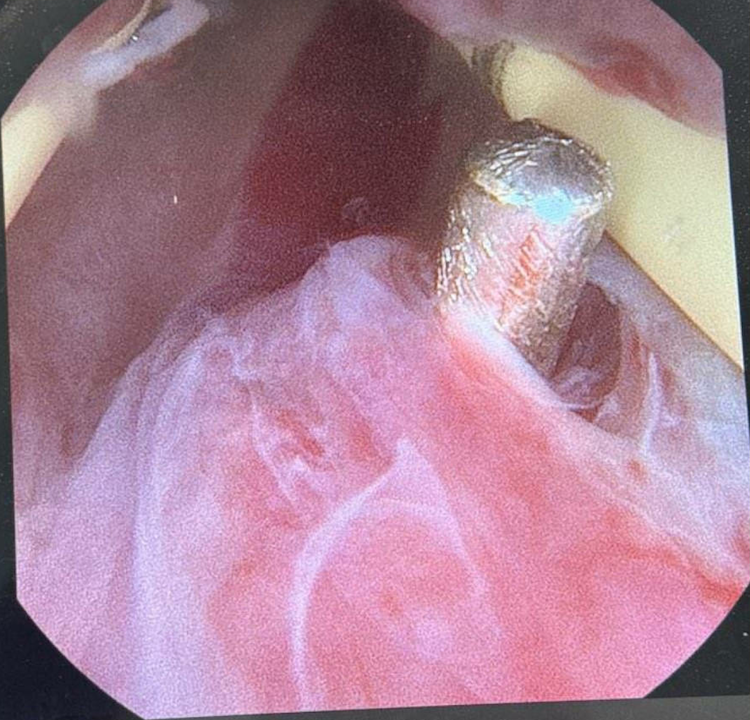
Figure: Figure 1. Ileal opening of ileourethral fistula
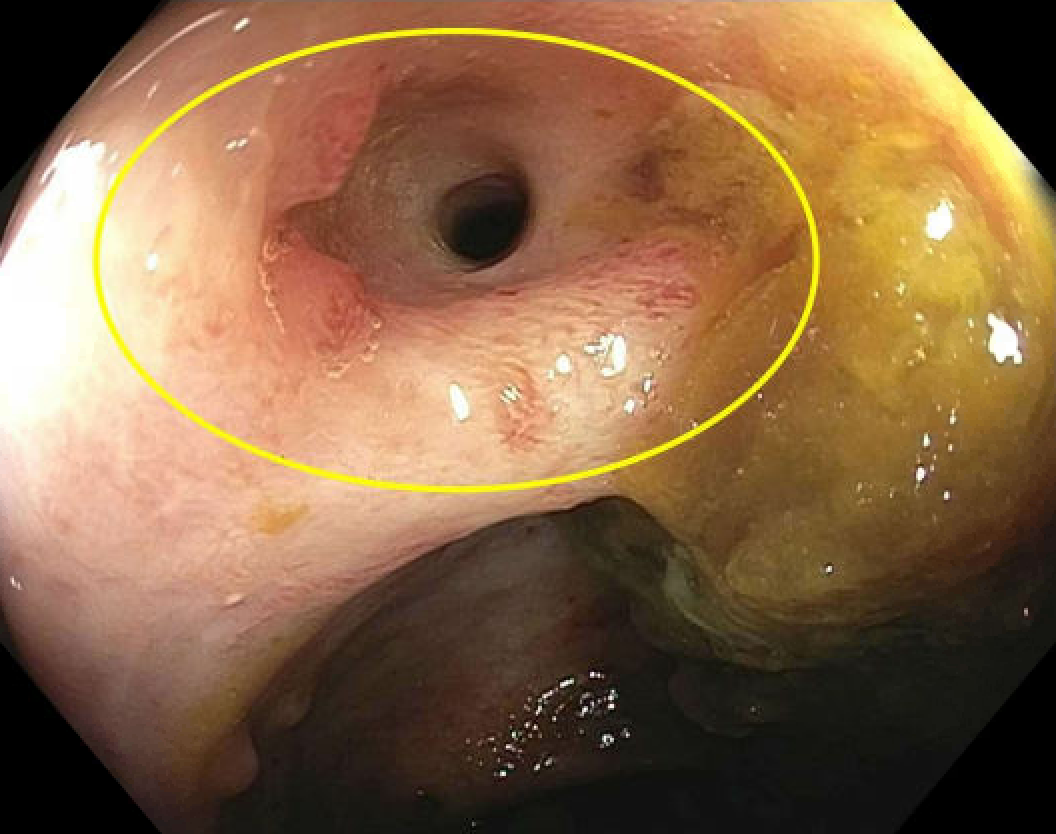
Figure: Figure 2. Urethral opening of ileourethral fistula
Disclosures:
Robert Ferguson indicated no relevant financial relationships.
Vinod Jeyaretnam: Bristol Meyers Squibb – Stock-publicly held company(excluding mutual/index funds).
Carla Erb indicated no relevant financial relationships.
Gregory Smith indicated no relevant financial relationships.
Robert Graham. Ferguson, MD, MPH1, Vinod Jeyaretnam, DO1, Carla Erb, DO1, Gregory Smith, MD2. P3401 - Conservative Management at What Cost?: Trans-Prostate Ileourethral Fistula in Crohn’s Disease Post-Ileal Pouch-Anal Anastomosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

