Monday Poster Session
Category: IBD
P3398 - Scallops, Strictures, and Surprises: Unmasking Celiac Disease in a Suspected IBD Case
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Gopala Koneru, MBBS
University of Iowa Hospitals & Clinics
Iowa City, IA
Presenting Author(s)
Gopala Koneru, MBBS, Tanner Simonson, MD, Jeffrey Goldman, MD
University of Iowa Hospitals & Clinics, Iowa City, IA
Introduction: Crohn’s disease has a wide clinicopathological spectrum, which can include segmental small bowel inflammation and strictures. Its symptoms can resemble those of other digestive problems including celiac disease. Rarely, celiac disease can closely mimic Crohn’s disease on imaging, complicating diagnosis. Keeping a wide differential diagnosis including unusual manifestations of common diseases is critical to avoid misdiagnosis and unnecessary immunosuppressive therapy.
Case Description/
Methods: A 56-year-old man with no remarkable past medical or family history came with intermittent abdominal distension and diarrhea which existed from the beginning of 2000. CT enterography requested by his primary physician demonstrated multifocal small bowel wall thickening, mucosal hyperenhancement, and segmental strictures with intervening dilation, raising concern for Crohn’s disease (Figure 1a,b,c,d). Symptoms improved transiently after empiric prednisone therapy, leading to referral for Gastroenterology evaluation.
Labs were unrevealing at time of initial evaluation including negative CRP and AST only minimally elevated (42 U/L). Empiric budesonide was started and the possibility of long-term immunosuppression was entertained. Double balloon enteroscopy (DBE) performed to evaluate strictures reached ~200 cm beyond the pylorus, demonstrating diffuse scalloping of jejunal folds but no ulcers or strictures. The biopsies demonstrated patchy architectural distortion but no active inflammation, granulomas or dysplasia (figure2a).
Tissue transglutaminase IgA serology was promptly requested due to the endoscopic findings, which came back significantly raised ( >250 IU/mL). Subsequent pathology revaluation identified villous blunting and increased intraepithelial lymphocytes (up to 40 per 100 enterocytes) (Figure 2b), consistent with celiac disease. Gluten free diet was recommended, budesonide was discontinued, and long-term immunosuppression was deferred. Repeat imaging and upper endoscopy was scheduled to monitor response.
Discussion: This case demonstrates the difficulty in obtaining an accurate diagnosis between Crohn’s disease and celiac disease when there is ambiguity in imaging characteristics and clinical signs. A comprehensive evaluation integrating imaging modalities, serologic testing, endoscopic assessment, and histological analysis, is critical to an accurate diagnosis which can help with effective management and avoiding unnecessary immunosuppressive therapies.
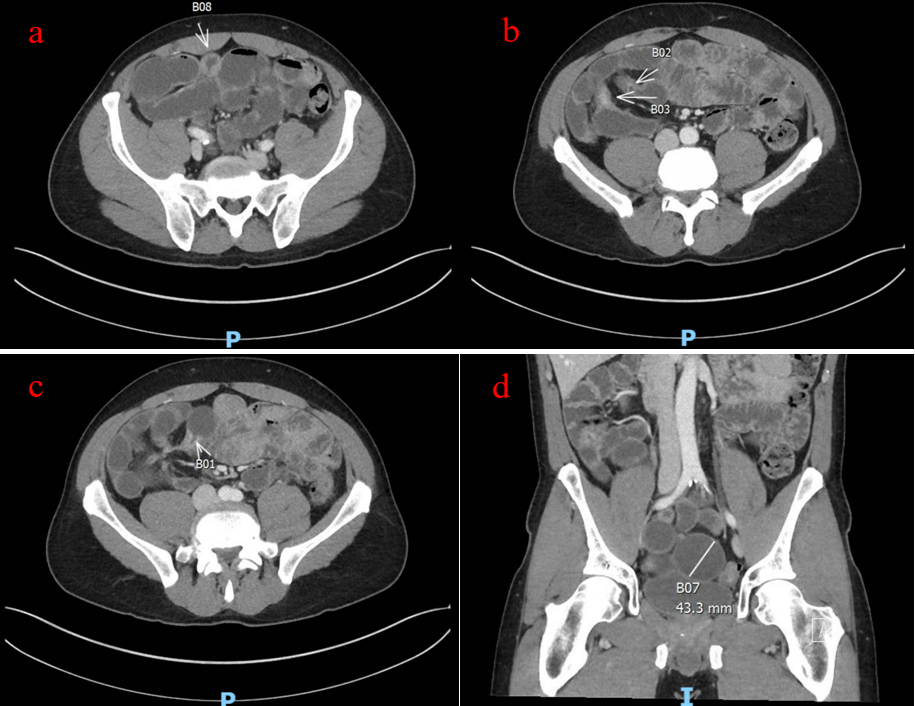
Figure: Figure 1: (a) Small bowel segmental wall thickening. (b, c) Mucosal hyperenhancement of the small bowel with strictures. (d) Multiple areas of segmental dilation measuring up to 4.3 cm.
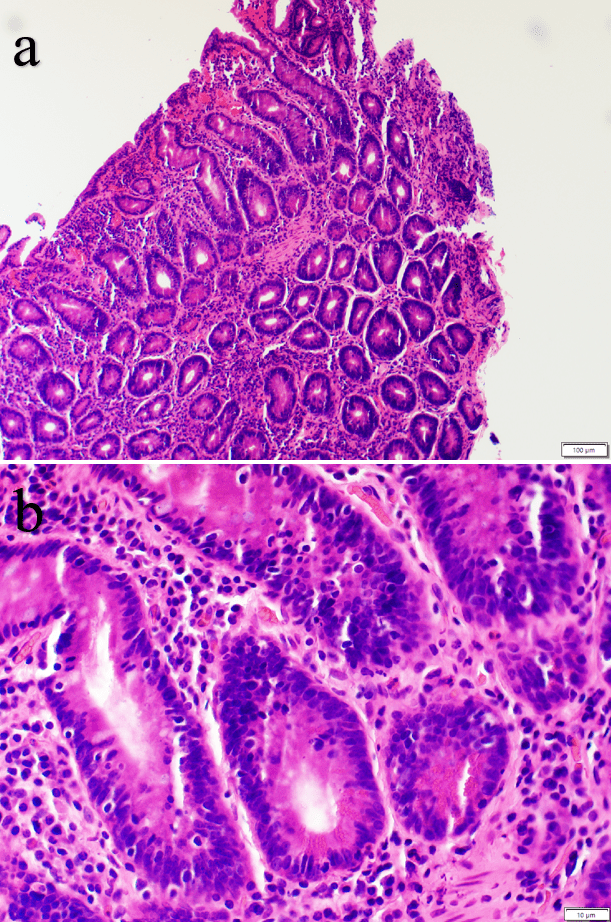
Figure: Figure 2: (a) Histologic sections showed patchy architectural distortion including shortening of the villi. (b) High power view demonstrates focally increased intraepithelial lymphocytes (up to 40 per 100 enterocytes) without active inflammation, granulomas or dysplasia.
Disclosures:
Gopala Koneru indicated no relevant financial relationships.
Tanner Simonson indicated no relevant financial relationships.
Jeffrey Goldman indicated no relevant financial relationships.
Gopala Koneru, MBBS, Tanner Simonson, MD, Jeffrey Goldman, MD. P3398 - Scallops, Strictures, and Surprises: Unmasking Celiac Disease in a Suspected IBD Case, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Iowa Hospitals & Clinics, Iowa City, IA
Introduction: Crohn’s disease has a wide clinicopathological spectrum, which can include segmental small bowel inflammation and strictures. Its symptoms can resemble those of other digestive problems including celiac disease. Rarely, celiac disease can closely mimic Crohn’s disease on imaging, complicating diagnosis. Keeping a wide differential diagnosis including unusual manifestations of common diseases is critical to avoid misdiagnosis and unnecessary immunosuppressive therapy.
Case Description/
Methods: A 56-year-old man with no remarkable past medical or family history came with intermittent abdominal distension and diarrhea which existed from the beginning of 2000. CT enterography requested by his primary physician demonstrated multifocal small bowel wall thickening, mucosal hyperenhancement, and segmental strictures with intervening dilation, raising concern for Crohn’s disease (Figure 1a,b,c,d). Symptoms improved transiently after empiric prednisone therapy, leading to referral for Gastroenterology evaluation.
Labs were unrevealing at time of initial evaluation including negative CRP and AST only minimally elevated (42 U/L). Empiric budesonide was started and the possibility of long-term immunosuppression was entertained. Double balloon enteroscopy (DBE) performed to evaluate strictures reached ~200 cm beyond the pylorus, demonstrating diffuse scalloping of jejunal folds but no ulcers or strictures. The biopsies demonstrated patchy architectural distortion but no active inflammation, granulomas or dysplasia (figure2a).
Tissue transglutaminase IgA serology was promptly requested due to the endoscopic findings, which came back significantly raised ( >250 IU/mL). Subsequent pathology revaluation identified villous blunting and increased intraepithelial lymphocytes (up to 40 per 100 enterocytes) (Figure 2b), consistent with celiac disease. Gluten free diet was recommended, budesonide was discontinued, and long-term immunosuppression was deferred. Repeat imaging and upper endoscopy was scheduled to monitor response.
Discussion: This case demonstrates the difficulty in obtaining an accurate diagnosis between Crohn’s disease and celiac disease when there is ambiguity in imaging characteristics and clinical signs. A comprehensive evaluation integrating imaging modalities, serologic testing, endoscopic assessment, and histological analysis, is critical to an accurate diagnosis which can help with effective management and avoiding unnecessary immunosuppressive therapies.
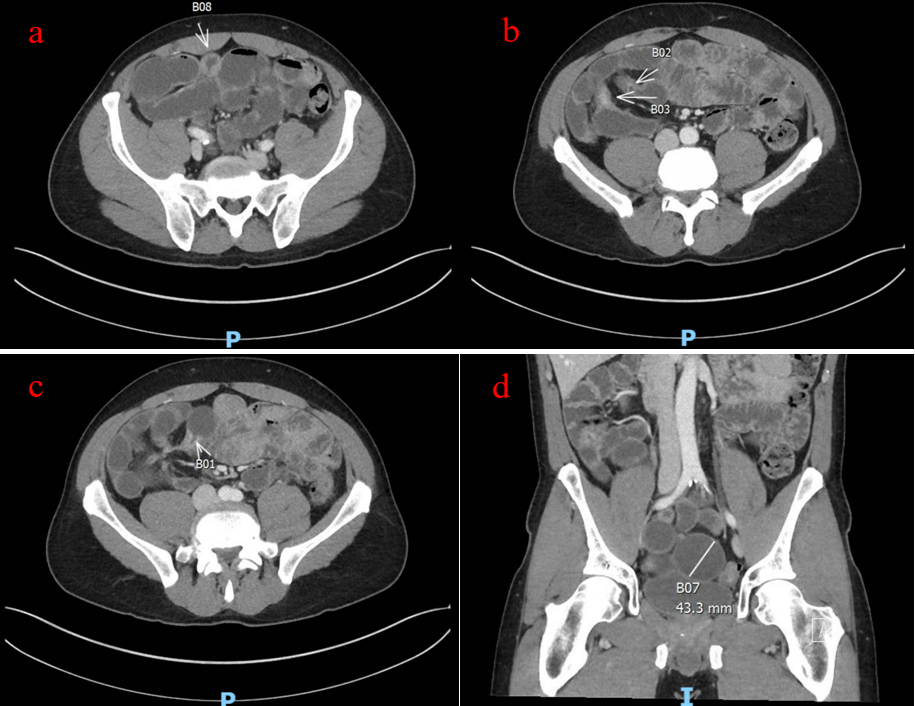
Figure: Figure 1: (a) Small bowel segmental wall thickening. (b, c) Mucosal hyperenhancement of the small bowel with strictures. (d) Multiple areas of segmental dilation measuring up to 4.3 cm.
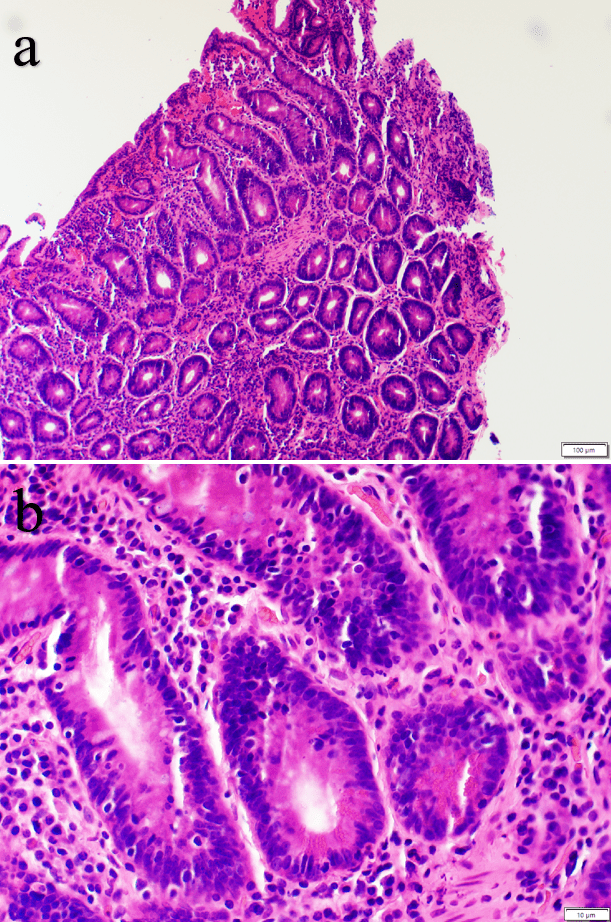
Figure: Figure 2: (a) Histologic sections showed patchy architectural distortion including shortening of the villi. (b) High power view demonstrates focally increased intraepithelial lymphocytes (up to 40 per 100 enterocytes) without active inflammation, granulomas or dysplasia.
Disclosures:
Gopala Koneru indicated no relevant financial relationships.
Tanner Simonson indicated no relevant financial relationships.
Jeffrey Goldman indicated no relevant financial relationships.
Gopala Koneru, MBBS, Tanner Simonson, MD, Jeffrey Goldman, MD. P3398 - Scallops, Strictures, and Surprises: Unmasking Celiac Disease in a Suspected IBD Case, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
