Monday Poster Session
Category: IBD
P3394 - Between Two Strictures: A Rare Case of Enterolith Formation in Longstanding Crohn's Disease
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Nourhan Saleh, MD
University of Missouri Health Care
Columbia, MO
Presenting Author(s)
Nourhan Saleh, MD1, Ibukunoluwa Oshobu, MD, MPH1, Eunice Aregbesola, MD2, Mahmoud Mansour, MD1, Khulood Ahmed, MD1
1University of Missouri Health Care, Columbia, MO; 2University of Missouri, Columbia, Columbia, MO
Introduction: Crohn's disease is a chronic inflammatory condition that can lead to stricturing and penetrating complications. Enterolith formation, while more commonly reported in small bowel diverticula and gallstone disease, represents an exceptionally rare complication in Crohn's disease. The unusual nature of this complication and its management challenges warrant documentation to enhance clinical awareness.
Case Description/
Methods: A 73-year-old male with Crohn's ileitis diagnosed in 1978 and ileal resection in the 1980s presented with recent changes in bowel habits. He had been without medical therapy for approximately 30 years. He reported diarrhea with 4-5 loose bowel movements daily but denied abdominal pain, weight loss, or hematochezia.
Imaging revealed a 2.5 cm calcified structure within the mid-distal ileum with associated wall thickening. Colonoscopy was normal with biopsies showing no active inflammation. MR enterography confirmed the intraluminal calcified structure with inflammatory changes proximal and distal to it.
Surgical intervention was recommended based on risk for future obstruction, fibrotic strictures unlikely to resolve with medical therapy, concern for potential malignancy, and technical challenges of endoscopic removal.
The patient underwent laparoscopic small bowel resection. Two strictures were identified within 4 cm of each other in the mid ileum with a palpable foreign body between them. An approximately 15 cm segment of ileum was resected. Pathology confirmed Crohn's disease with two stenoses and a 2.5 cm dark green calculus. The patient had an uneventful recovery.
Discussion: The pathophysiology of enterolith formation involves salt precipitation in areas of intestinal stasis, particularly in the alkaline small bowel environment. This case featured an enterolith trapped between two closely positioned strictures in a patient who had minimal symptoms for decades before developing diarrhea.
Diagnostic imaging initially raised consideration of gallstone ileus. However, the absence of pneumobilia on imaging, along with the patient's remote cholecystectomy history and the characteristic position between two inflammatory strictures, all supported a primary enterolith rather than a migrated gallstone.
Surgical intervention proved highly effective when faced with anatomical complexity that limited endoscopic options. This case highlights a rarely reported complication of Crohn's disease and the importance of considering the pathophysiology and anatomical features in management.
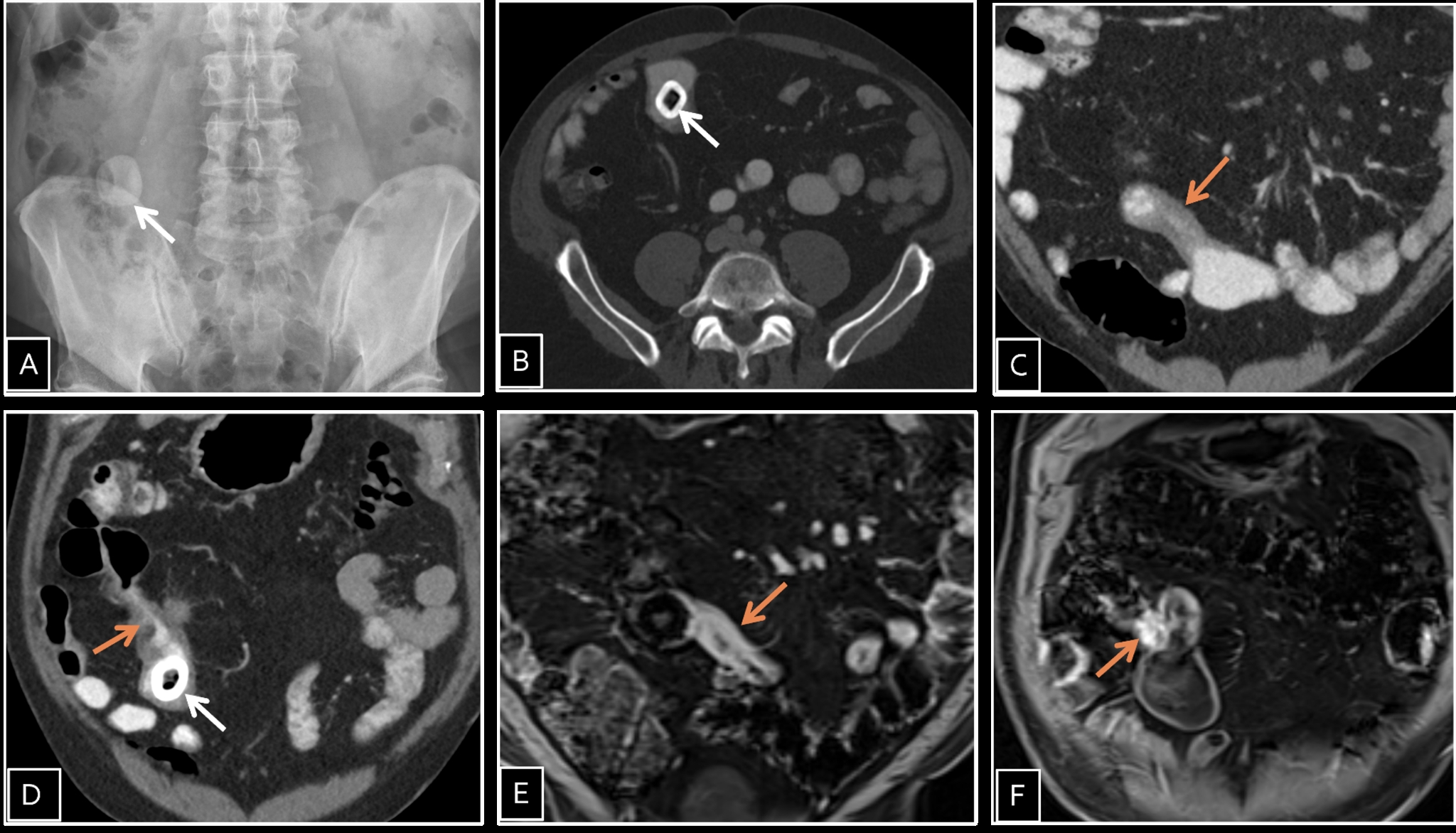
Figure: (A) Plain abdominal radiograph shows rounded hyperdense structure in the right iliac fossa (white arrow) (B), (C) and (D) Axial and coronal CT images show distal ileum calculus (white arrows) with associated proximal and distal bowel wall thickening.
(E) and (D) coronal MR images show the calculus with associated mural thickening and mucosal hyper-enhancing (orange arrows) noted at the distal ileum at the small bowel anastomotic site. Overall features are suggestive of entero-lithiasis with ileal inflammatory changes which could be related to the patient’s history of Crohn's disease versus reactive changes to entero-lithiasis.
Disclosures:
Nourhan Saleh indicated no relevant financial relationships.
Ibukunoluwa Oshobu indicated no relevant financial relationships.
Eunice Aregbesola indicated no relevant financial relationships.
Mahmoud Mansour indicated no relevant financial relationships.
Khulood Ahmed indicated no relevant financial relationships.
Nourhan Saleh, MD1, Ibukunoluwa Oshobu, MD, MPH1, Eunice Aregbesola, MD2, Mahmoud Mansour, MD1, Khulood Ahmed, MD1. P3394 - Between Two Strictures: A Rare Case of Enterolith Formation in Longstanding Crohn's Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Missouri Health Care, Columbia, MO; 2University of Missouri, Columbia, Columbia, MO
Introduction: Crohn's disease is a chronic inflammatory condition that can lead to stricturing and penetrating complications. Enterolith formation, while more commonly reported in small bowel diverticula and gallstone disease, represents an exceptionally rare complication in Crohn's disease. The unusual nature of this complication and its management challenges warrant documentation to enhance clinical awareness.
Case Description/
Methods: A 73-year-old male with Crohn's ileitis diagnosed in 1978 and ileal resection in the 1980s presented with recent changes in bowel habits. He had been without medical therapy for approximately 30 years. He reported diarrhea with 4-5 loose bowel movements daily but denied abdominal pain, weight loss, or hematochezia.
Imaging revealed a 2.5 cm calcified structure within the mid-distal ileum with associated wall thickening. Colonoscopy was normal with biopsies showing no active inflammation. MR enterography confirmed the intraluminal calcified structure with inflammatory changes proximal and distal to it.
Surgical intervention was recommended based on risk for future obstruction, fibrotic strictures unlikely to resolve with medical therapy, concern for potential malignancy, and technical challenges of endoscopic removal.
The patient underwent laparoscopic small bowel resection. Two strictures were identified within 4 cm of each other in the mid ileum with a palpable foreign body between them. An approximately 15 cm segment of ileum was resected. Pathology confirmed Crohn's disease with two stenoses and a 2.5 cm dark green calculus. The patient had an uneventful recovery.
Discussion: The pathophysiology of enterolith formation involves salt precipitation in areas of intestinal stasis, particularly in the alkaline small bowel environment. This case featured an enterolith trapped between two closely positioned strictures in a patient who had minimal symptoms for decades before developing diarrhea.
Diagnostic imaging initially raised consideration of gallstone ileus. However, the absence of pneumobilia on imaging, along with the patient's remote cholecystectomy history and the characteristic position between two inflammatory strictures, all supported a primary enterolith rather than a migrated gallstone.
Surgical intervention proved highly effective when faced with anatomical complexity that limited endoscopic options. This case highlights a rarely reported complication of Crohn's disease and the importance of considering the pathophysiology and anatomical features in management.
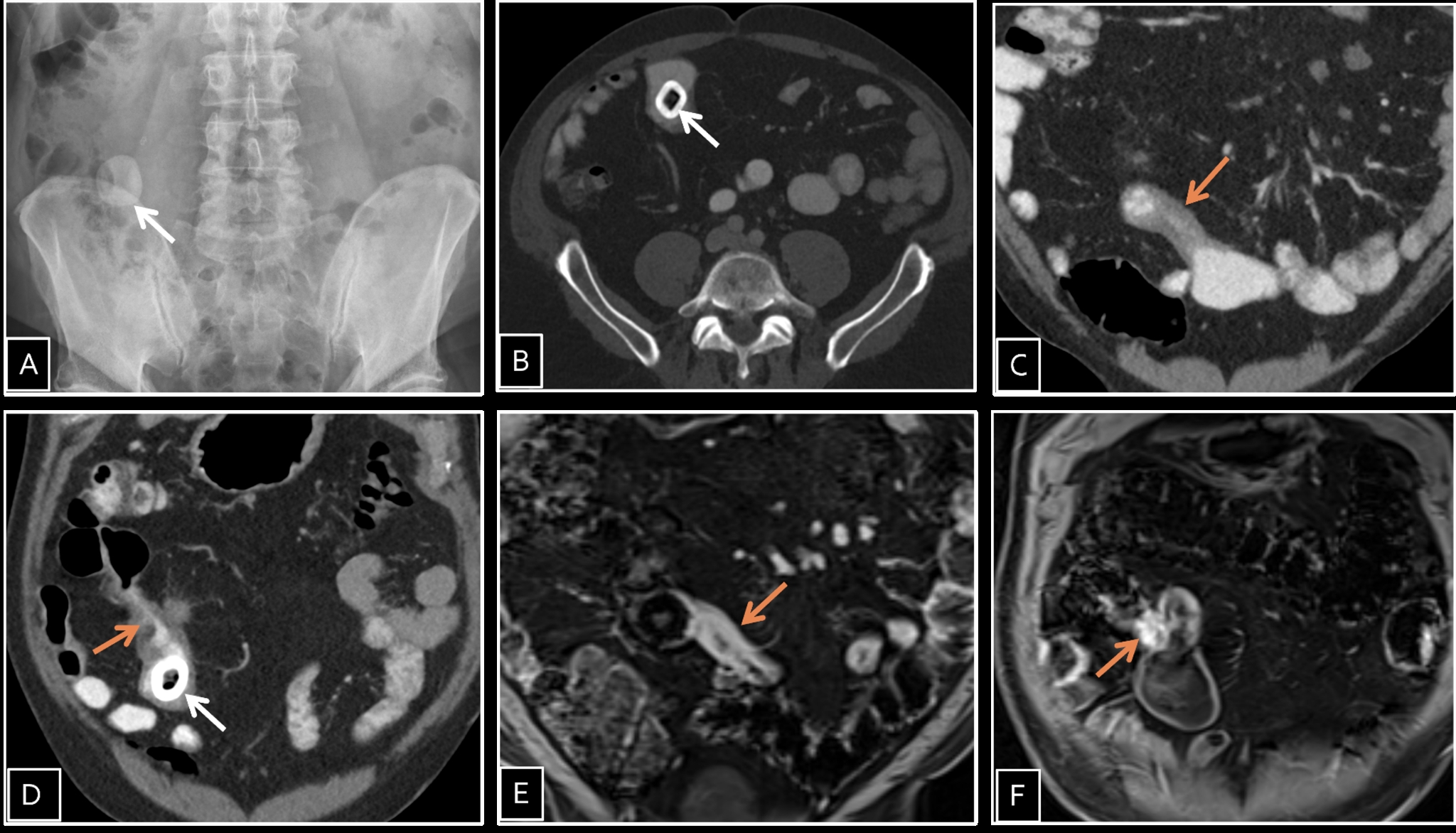
Figure: (A) Plain abdominal radiograph shows rounded hyperdense structure in the right iliac fossa (white arrow) (B), (C) and (D) Axial and coronal CT images show distal ileum calculus (white arrows) with associated proximal and distal bowel wall thickening.
(E) and (D) coronal MR images show the calculus with associated mural thickening and mucosal hyper-enhancing (orange arrows) noted at the distal ileum at the small bowel anastomotic site. Overall features are suggestive of entero-lithiasis with ileal inflammatory changes which could be related to the patient’s history of Crohn's disease versus reactive changes to entero-lithiasis.
Disclosures:
Nourhan Saleh indicated no relevant financial relationships.
Ibukunoluwa Oshobu indicated no relevant financial relationships.
Eunice Aregbesola indicated no relevant financial relationships.
Mahmoud Mansour indicated no relevant financial relationships.
Khulood Ahmed indicated no relevant financial relationships.
Nourhan Saleh, MD1, Ibukunoluwa Oshobu, MD, MPH1, Eunice Aregbesola, MD2, Mahmoud Mansour, MD1, Khulood Ahmed, MD1. P3394 - Between Two Strictures: A Rare Case of Enterolith Formation in Longstanding Crohn's Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

