Monday Poster Session
Category: IBD
P3334 - Inflammation and Proliferation: Burden of Myeloproliferative Disorders in Patients With IBD - A Real-World Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mohammad Kloub, MD (he/him/his)
New York Medical College - Saint Michael's Medical Center
Bloomfield, NJ
Presenting Author(s)
Mohammad Kloub, MD1, Abdellatif Ismail, MD2, Mohammed Al-Aquily, MD3, Mohamed Eldesouki, MD4, Abdulrahman Abusalim, MD5, Yamini Katamreddy, MD6, Mohammad Nabil Rayad, MD6, Muhammad Hussain, MD7, Shehab Mohamed, MD8, Yatinder Bains, MD7
1New York Medical College - Saint Michael's Medical Center, Bloomfield, NJ; 2University of Maryland Medical Center, Baltimore, MD; 3Norwalk Hospital/Yale University, Norwalk, CT; 4Saint Michael's Medical Center, New York Medical College, Newark, NJ; 5University of Wisconsin School of Medicine and Public Health, Madison, WI; 6New York Medical College - Saint Micheal’s Medical Center, Newark, NJ; 7New York Medical College - Saint Michael's Medical Center, Newark, NJ; 8Hamad Medical Corporation, Doha, Ad Dawhah, Qatar
Introduction: Inflammatory bowel disease (IBD) has been linked to myeloproliferative neoplasm (MPN) such as essential thrombocythemia (ET), polycythemia vera (PV), and myelofibrosis (MF). Data suggests that IBD and MPN share similar pathophysiological mechanisms, including chronic systemic inflammation and genetic profiles. However, real-world data evaluating clinical outcomes in patients with both IBD and MPN are limited. This study aims to compare IBD-related outcomes in patients with coexisting IBD and MPN versus those with IBD alone.
Methods: A retrospective cohort study on the TriNetX platform. Adult with newly diagnosed IBD were included in the study and followed up for 5 years. The patients were divided into two cohorts: Cohort 1: patients with IBD and MPN diagnosis and Cohort 2: patients with IBD alone diagnosis. Propensity score matching (PSM) was performed based on demographics, comorbidities, laboratory values, and medications as shown in Table 1. The primary outcome was the risk of CRC, colectomy, intestinal fistula, and obstruction while secondary outcome included the risk of iron deficiency anemia (IDA), malnutrition, depression, and overall mortality. Outcomes were analyzed using risk estimates over the 5-year follow-up and expressed as Hazard Ratios (HR) with two-sided P-values.
Results: After PSM, a total of 11,475 patients were included in each cohort. As shown in Table 2, The risk of colorectal cancer was significantly higher in MPN+IBD group compared to the control group (HR 1.63, 95% confidence intervals [CI]: 1.22–2.19, p < 0.001). Other complications were significantly higher in MPN+IBD group, including colectomy (HR 2.65; 95% CI: 2.16–3.25, p < 0.001), intestinal fistula (HR 2.41; 95% CI: 2.01–2.89, p < 0.001), bowel obstruction (HR 1.95 ; 95% CI: 1.76–2.16, p < 0.001), and intestinal perforation (HR 2.28; 95% CI: 1.83–2.85, p < 0.001). Additionally, the MPN+IBD cohort experienced higher rates of IDA (HR 2.29; 95% CI: 2.14–2.46, p < 0.001), malnutrition (HR 2.35; 95% CI: 2.15–2.57, p < 0.001), and depression (HR 1.23; 95% CI: 1.12–1.36, p < 0.001). All-cause mortality was not significantly higher between the two study groups.
Discussion: During a 5-year follow up, patients with co-existing IBD and MPN had a higher risk of CRC, colectomy, intestinal fistula, intestinal obstruction, IDA, malnutrition, and depression compared to IBD alone. Further prospective studies are needed to implement risk stratification strategies to improve clinical care for these vulnerable patients.
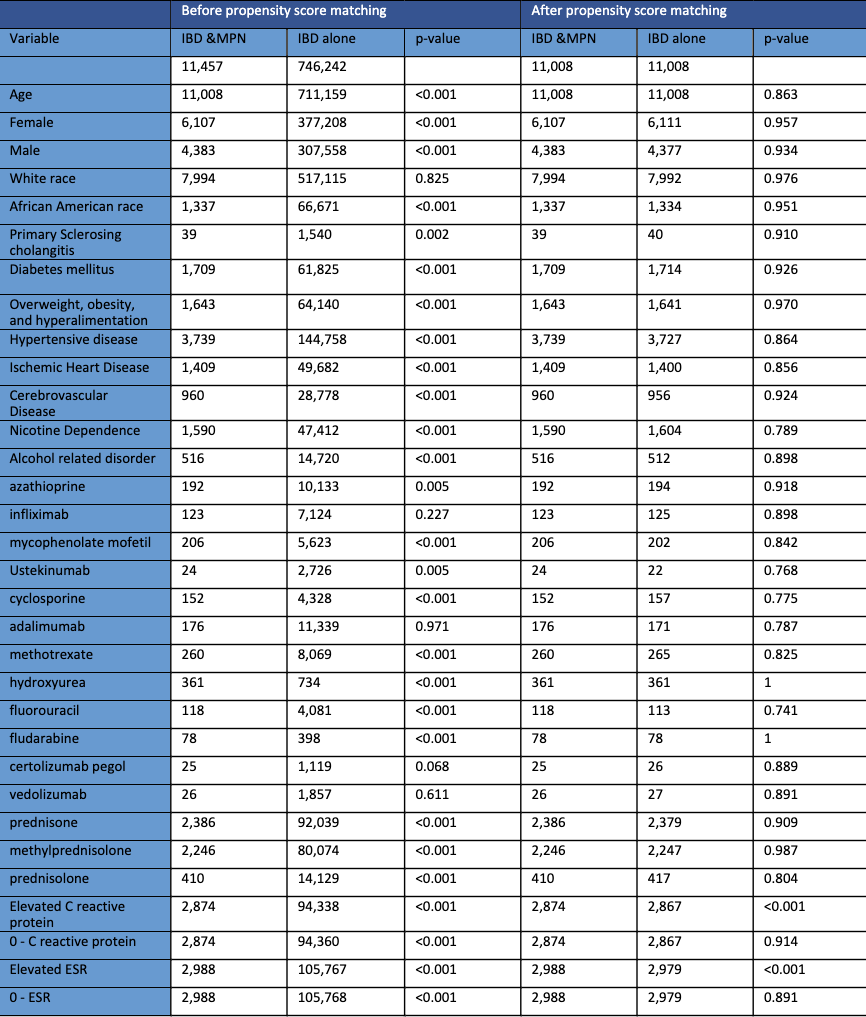
Figure: Table 1: The baseline characteristics of the 2 cohorts before and after propensity score matching.
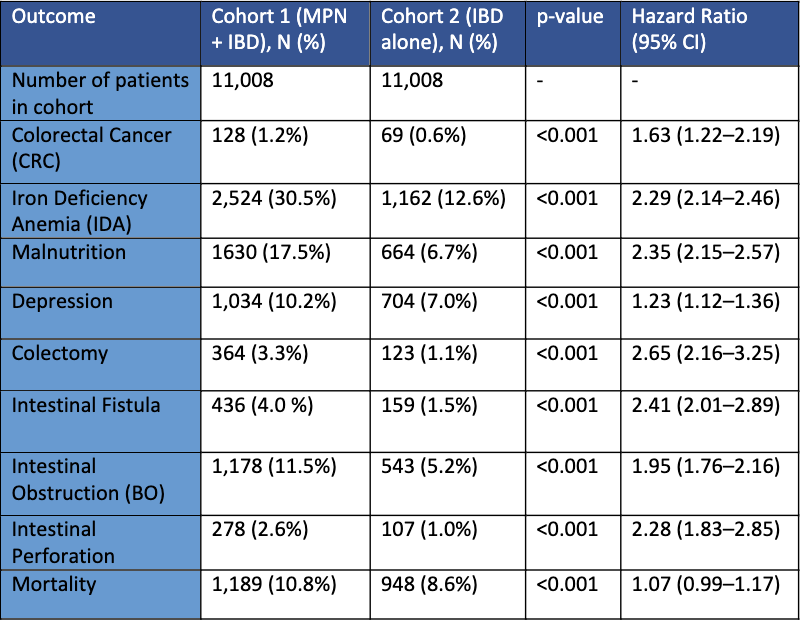
Figure: Table 2: Comparison of risk of primary outcome and secondary outcomes between patients in Cohort 1 (IBD & MPN diagnoses) and patients in Cohort 2 (IBD alone).
Disclosures:
Mohammad Kloub indicated no relevant financial relationships.
Abdellatif Ismail indicated no relevant financial relationships.
Mohammed Al-Aquily indicated no relevant financial relationships.
Mohamed Eldesouki indicated no relevant financial relationships.
Abdulrahman Abusalim indicated no relevant financial relationships.
Yamini Katamreddy indicated no relevant financial relationships.
Mohammad Nabil Rayad indicated no relevant financial relationships.
Muhammad Hussain indicated no relevant financial relationships.
Shehab Mohamed indicated no relevant financial relationships.
Yatinder Bains indicated no relevant financial relationships.
Mohammad Kloub, MD1, Abdellatif Ismail, MD2, Mohammed Al-Aquily, MD3, Mohamed Eldesouki, MD4, Abdulrahman Abusalim, MD5, Yamini Katamreddy, MD6, Mohammad Nabil Rayad, MD6, Muhammad Hussain, MD7, Shehab Mohamed, MD8, Yatinder Bains, MD7. P3334 - Inflammation and Proliferation: Burden of Myeloproliferative Disorders in Patients With IBD - A Real-World Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1New York Medical College - Saint Michael's Medical Center, Bloomfield, NJ; 2University of Maryland Medical Center, Baltimore, MD; 3Norwalk Hospital/Yale University, Norwalk, CT; 4Saint Michael's Medical Center, New York Medical College, Newark, NJ; 5University of Wisconsin School of Medicine and Public Health, Madison, WI; 6New York Medical College - Saint Micheal’s Medical Center, Newark, NJ; 7New York Medical College - Saint Michael's Medical Center, Newark, NJ; 8Hamad Medical Corporation, Doha, Ad Dawhah, Qatar
Introduction: Inflammatory bowel disease (IBD) has been linked to myeloproliferative neoplasm (MPN) such as essential thrombocythemia (ET), polycythemia vera (PV), and myelofibrosis (MF). Data suggests that IBD and MPN share similar pathophysiological mechanisms, including chronic systemic inflammation and genetic profiles. However, real-world data evaluating clinical outcomes in patients with both IBD and MPN are limited. This study aims to compare IBD-related outcomes in patients with coexisting IBD and MPN versus those with IBD alone.
Methods: A retrospective cohort study on the TriNetX platform. Adult with newly diagnosed IBD were included in the study and followed up for 5 years. The patients were divided into two cohorts: Cohort 1: patients with IBD and MPN diagnosis and Cohort 2: patients with IBD alone diagnosis. Propensity score matching (PSM) was performed based on demographics, comorbidities, laboratory values, and medications as shown in Table 1. The primary outcome was the risk of CRC, colectomy, intestinal fistula, and obstruction while secondary outcome included the risk of iron deficiency anemia (IDA), malnutrition, depression, and overall mortality. Outcomes were analyzed using risk estimates over the 5-year follow-up and expressed as Hazard Ratios (HR) with two-sided P-values.
Results: After PSM, a total of 11,475 patients were included in each cohort. As shown in Table 2, The risk of colorectal cancer was significantly higher in MPN+IBD group compared to the control group (HR 1.63, 95% confidence intervals [CI]: 1.22–2.19, p < 0.001). Other complications were significantly higher in MPN+IBD group, including colectomy (HR 2.65; 95% CI: 2.16–3.25, p < 0.001), intestinal fistula (HR 2.41; 95% CI: 2.01–2.89, p < 0.001), bowel obstruction (HR 1.95 ; 95% CI: 1.76–2.16, p < 0.001), and intestinal perforation (HR 2.28; 95% CI: 1.83–2.85, p < 0.001). Additionally, the MPN+IBD cohort experienced higher rates of IDA (HR 2.29; 95% CI: 2.14–2.46, p < 0.001), malnutrition (HR 2.35; 95% CI: 2.15–2.57, p < 0.001), and depression (HR 1.23; 95% CI: 1.12–1.36, p < 0.001). All-cause mortality was not significantly higher between the two study groups.
Discussion: During a 5-year follow up, patients with co-existing IBD and MPN had a higher risk of CRC, colectomy, intestinal fistula, intestinal obstruction, IDA, malnutrition, and depression compared to IBD alone. Further prospective studies are needed to implement risk stratification strategies to improve clinical care for these vulnerable patients.
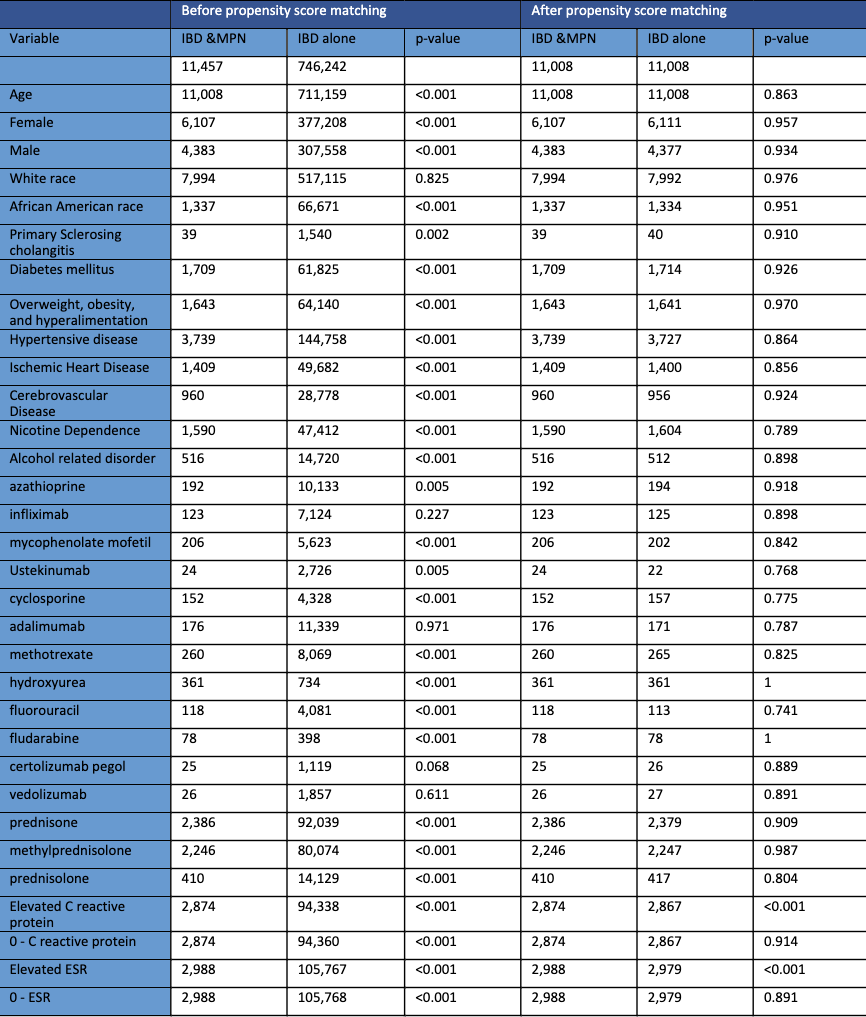
Figure: Table 1: The baseline characteristics of the 2 cohorts before and after propensity score matching.
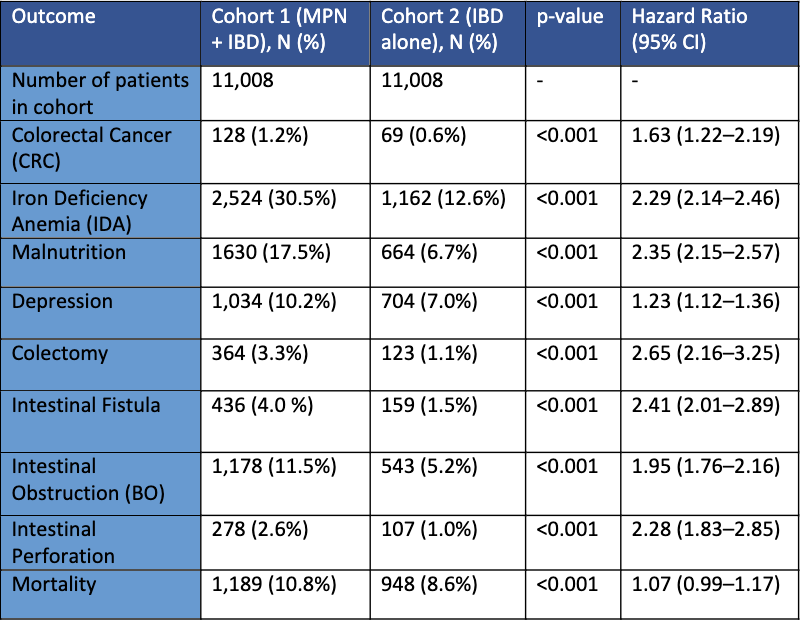
Figure: Table 2: Comparison of risk of primary outcome and secondary outcomes between patients in Cohort 1 (IBD & MPN diagnoses) and patients in Cohort 2 (IBD alone).
Disclosures:
Mohammad Kloub indicated no relevant financial relationships.
Abdellatif Ismail indicated no relevant financial relationships.
Mohammed Al-Aquily indicated no relevant financial relationships.
Mohamed Eldesouki indicated no relevant financial relationships.
Abdulrahman Abusalim indicated no relevant financial relationships.
Yamini Katamreddy indicated no relevant financial relationships.
Mohammad Nabil Rayad indicated no relevant financial relationships.
Muhammad Hussain indicated no relevant financial relationships.
Shehab Mohamed indicated no relevant financial relationships.
Yatinder Bains indicated no relevant financial relationships.
Mohammad Kloub, MD1, Abdellatif Ismail, MD2, Mohammed Al-Aquily, MD3, Mohamed Eldesouki, MD4, Abdulrahman Abusalim, MD5, Yamini Katamreddy, MD6, Mohammad Nabil Rayad, MD6, Muhammad Hussain, MD7, Shehab Mohamed, MD8, Yatinder Bains, MD7. P3334 - Inflammation and Proliferation: Burden of Myeloproliferative Disorders in Patients With IBD - A Real-World Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
