Monday Poster Session
Category: IBD
P3327 - The Hidden Burden of Mental Health in Inflammatory Bowel Disease: A 6-Year National Readmissions Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Silpa Choday, MD (she/her/hers)
Creighton University School of Medicine
Phoenix, AZ
Presenting Author(s)
Silpa Choday, MD1, Keng-Yu Chuang, MD2, Savio Reddymasu, MD1, Neil Vyas, MD1
1Creighton University School of Medicine, Phoenix, AZ; 2GI Alliance, Phoenix, AZ
Introduction: Inflammatory Bowel Disease (IBD), encompassing Crohn’s Disease (CD) and Ulcerative Colitis (UC), is associated with a range of psychiatric disorder (d/o) and substance use comorbidities. This study aims to assess the trends in these comorbidities over time in IBD patients.
Methods: We used data from Nationwide Readmissions Database (2016-2021) on the prevalence of mental health d/o and substance use for CD and UC. Inflation-adjusted costs were adjusted to 2021 U.S. dollars
Results: We identified 2,580,740 records, out of which 201, 052 has 30-day and 333, 585 has 90-day readmissions (P< 0.001). The mean age is 53.34 years, with females comprising of 56% admissions. For CD, significant increases were observed in the prevalence of depression and anxiety (18% and 20%, P< 0.01) compared to UC (16% and 17.2%, P< 0.001), with similar trends observed for bipolar d/o, post-traumatic stress d/o (PTSD) and attention-deficit/hyperactivity d/o (ADHD) (P< 0.001). Schizophrenia rates were consistent across groups at approximately 1% (P< 0.001).
Substance use d/o were notably higher in CD patients (24.1%) compared to UC patients (16%), with higher cannabis and cocaine use in CD patients (P< 0.001). However, alcohol use was slightly higher in UC (4% vs. 3.5% in CD). Clinically, UC patients had longer hospital stays (5.8 vs. 5.2 days), higher hospital charges ($71,645 vs. $60,673), and greater mortality (2.2% vs. 1.3%) compared to CD, indicating severe inpatient outcomes in UC
Yearly trends from 2016 to 2021 showed a significant increase in the prevalence of psychiatric d/o and substance use in both CD and UC patients. In CD, depression increased from 17% to 18.1% (P = 0.01), anxiety rose from 18.2% to 22% (P < 0.001), and substance use d/o increased from 23.6% to 25% (P= 0.04). Cannabis use nearly doubled from 2.7% to 4% (P < 0.001). In UC, depression rose from 15% to 17% (P < 0.001), anxiety from 15.8% to 20% (P < 0.001), and substance use increased from 14.1% to 16% (P < 0.001). Alcohol (3.7% to 5%, P < 0.001) and cannabis use (1.6% to 2.5%, P < 0.001) also increased significantly in UC.
Discussion: CD patients exhibited higher rates of mental health d/o and substance use, particularly cannabis and cocaine, while UC patients experienced more severe clinical outcomes, including longer hospital stays, higher healthcare costs, and increased mortality. Both CD and UC had upward trends in depression, anxiety, PTSD, ADHD, and substance use.
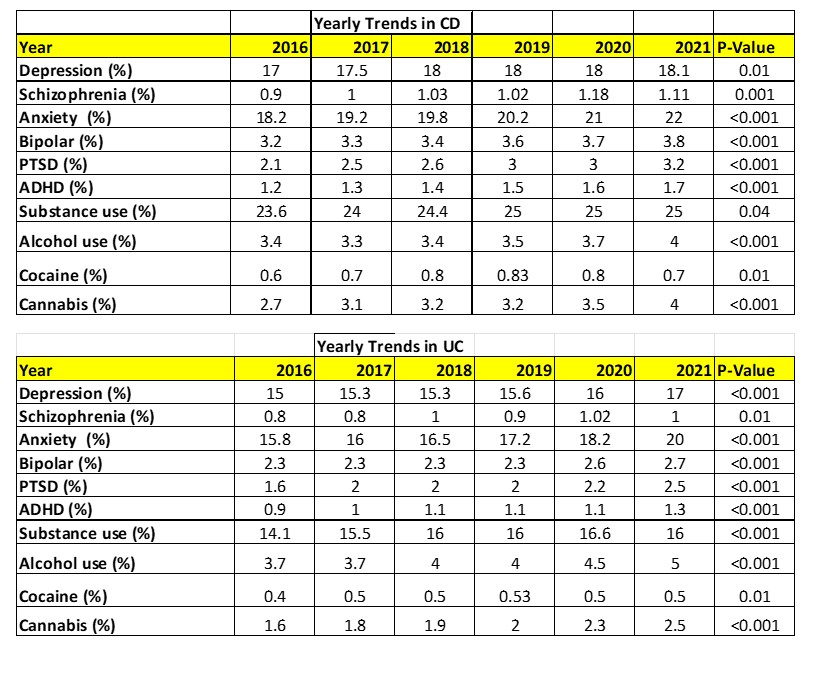
Figure: Mental Health and Substance use Yearly Trends of CD and UC
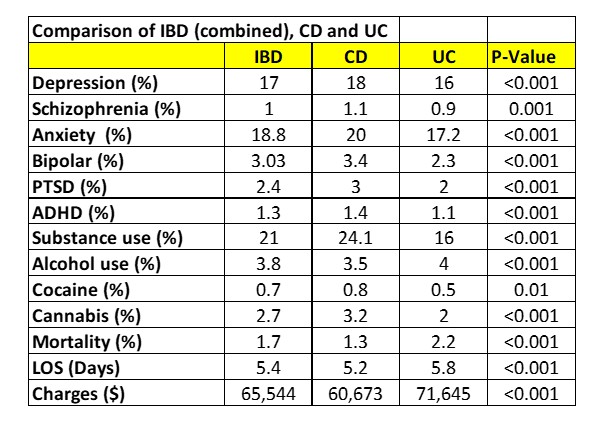
Figure: Comparison of IBD versus CD versus UC
Disclosures:
Silpa Choday indicated no relevant financial relationships.
Keng-Yu Chuang indicated no relevant financial relationships.
Savio Reddymasu indicated no relevant financial relationships.
Neil Vyas indicated no relevant financial relationships.
Silpa Choday, MD1, Keng-Yu Chuang, MD2, Savio Reddymasu, MD1, Neil Vyas, MD1. P3327 - The Hidden Burden of Mental Health in Inflammatory Bowel Disease: A 6-Year National Readmissions Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Creighton University School of Medicine, Phoenix, AZ; 2GI Alliance, Phoenix, AZ
Introduction: Inflammatory Bowel Disease (IBD), encompassing Crohn’s Disease (CD) and Ulcerative Colitis (UC), is associated with a range of psychiatric disorder (d/o) and substance use comorbidities. This study aims to assess the trends in these comorbidities over time in IBD patients.
Methods: We used data from Nationwide Readmissions Database (2016-2021) on the prevalence of mental health d/o and substance use for CD and UC. Inflation-adjusted costs were adjusted to 2021 U.S. dollars
Results: We identified 2,580,740 records, out of which 201, 052 has 30-day and 333, 585 has 90-day readmissions (P< 0.001). The mean age is 53.34 years, with females comprising of 56% admissions. For CD, significant increases were observed in the prevalence of depression and anxiety (18% and 20%, P< 0.01) compared to UC (16% and 17.2%, P< 0.001), with similar trends observed for bipolar d/o, post-traumatic stress d/o (PTSD) and attention-deficit/hyperactivity d/o (ADHD) (P< 0.001). Schizophrenia rates were consistent across groups at approximately 1% (P< 0.001).
Substance use d/o were notably higher in CD patients (24.1%) compared to UC patients (16%), with higher cannabis and cocaine use in CD patients (P< 0.001). However, alcohol use was slightly higher in UC (4% vs. 3.5% in CD). Clinically, UC patients had longer hospital stays (5.8 vs. 5.2 days), higher hospital charges ($71,645 vs. $60,673), and greater mortality (2.2% vs. 1.3%) compared to CD, indicating severe inpatient outcomes in UC
Yearly trends from 2016 to 2021 showed a significant increase in the prevalence of psychiatric d/o and substance use in both CD and UC patients. In CD, depression increased from 17% to 18.1% (P = 0.01), anxiety rose from 18.2% to 22% (P < 0.001), and substance use d/o increased from 23.6% to 25% (P= 0.04). Cannabis use nearly doubled from 2.7% to 4% (P < 0.001). In UC, depression rose from 15% to 17% (P < 0.001), anxiety from 15.8% to 20% (P < 0.001), and substance use increased from 14.1% to 16% (P < 0.001). Alcohol (3.7% to 5%, P < 0.001) and cannabis use (1.6% to 2.5%, P < 0.001) also increased significantly in UC.
Discussion: CD patients exhibited higher rates of mental health d/o and substance use, particularly cannabis and cocaine, while UC patients experienced more severe clinical outcomes, including longer hospital stays, higher healthcare costs, and increased mortality. Both CD and UC had upward trends in depression, anxiety, PTSD, ADHD, and substance use.
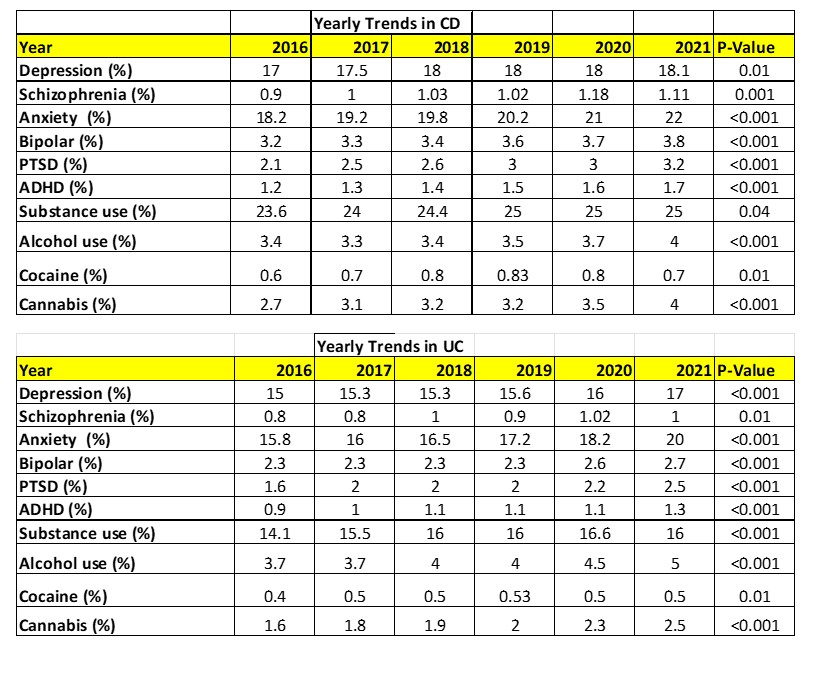
Figure: Mental Health and Substance use Yearly Trends of CD and UC
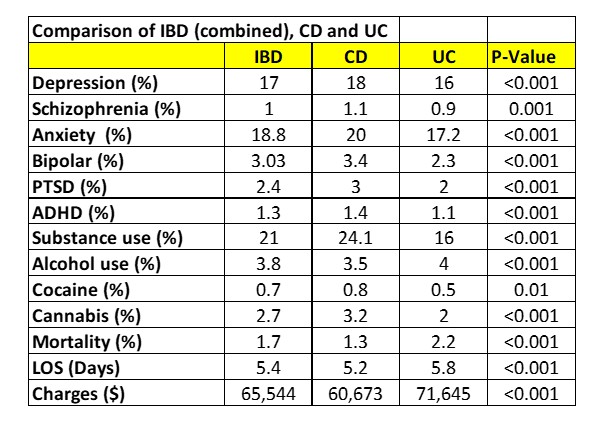
Figure: Comparison of IBD versus CD versus UC
Disclosures:
Silpa Choday indicated no relevant financial relationships.
Keng-Yu Chuang indicated no relevant financial relationships.
Savio Reddymasu indicated no relevant financial relationships.
Neil Vyas indicated no relevant financial relationships.
Silpa Choday, MD1, Keng-Yu Chuang, MD2, Savio Reddymasu, MD1, Neil Vyas, MD1. P3327 - The Hidden Burden of Mental Health in Inflammatory Bowel Disease: A 6-Year National Readmissions Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
