Monday Poster Session
Category: IBD
P3326 - Vitamin A Deficiency in IBD: A Large-Scale Population-Based Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Sabtain Saroya, BS (he/him/his)
College of Medicine, Howard University
Washington, DC
Presenting Author(s)
Sabtain Saroya, BS1, Armando Ugarte, 1, Matthew DeLeary, 1, Luke Nelson, 1, Kira Yates, 1, Mudasir Rashid, PhD2, Elizbeth Beyene, 2, Mekdem Bisrat, 1, Daniel Larbi, MD2, Miriam Michael, MD2
1College of Medicine, Howard University, Washington, DC; 2Howard University Hospital, Washington, DC
Introduction: Vitamin A, present as preformed retinoids and provitamin A carotenoids, is essential for vision, epithelial integrity, immune regulation, and mucosal maintenance. Although rare in developed nations, vitamin A deficiency (VAD) can arise from malabsorption, hepatic dysfunction, or inadequate intake. Inflammatory bowel disease (IBD) may predispose individuals to VAD through chronic inflammation and impaired nutrient absorption. This study investigates the prevalence and demographic distribution of VAD in IBD patients across a large U.S. population.
Methods: We conducted a retrospective cohort study using the TriNetX Research Network, comprising over 163 million patient records. A total of 829,248 patients with IBD were identified. We compared the prevalence and incidence of VAD between IBD and non-IBD populations and analyzed demographic trends, including age, sex, and race/ethnicity.
Results: In the general population, VAD incidence was 0.015%, with a prevalence of 0.016%. Among IBD patients, the incidence increased to 0.17% and prevalence to 0.183%—representing an over 11-fold increase. Females accounted for 52.68% of IBD cases, and VAD was disproportionately more common among White female patients.
Discussion: The markedly higher burden of VAD in IBD patients highlights a critical intersection between chronic inflammation, malabsorption, and increased micronutrient demands. The observed demographic disparity—particularly among White females—suggests a multifactorial etiology involving genetic, hormonal, and dietary influences. These findings support the incorporation of routine vitamin A screening into IBD management protocols. Early identification and targeted supplementation could mitigate nutritional deficiencies, reduce complications, and optimize clinical outcomes. Future research should focus on elucidating the underlying mechanisms and evaluating the therapeutic impact of vitamin A repletion in this high-risk population.
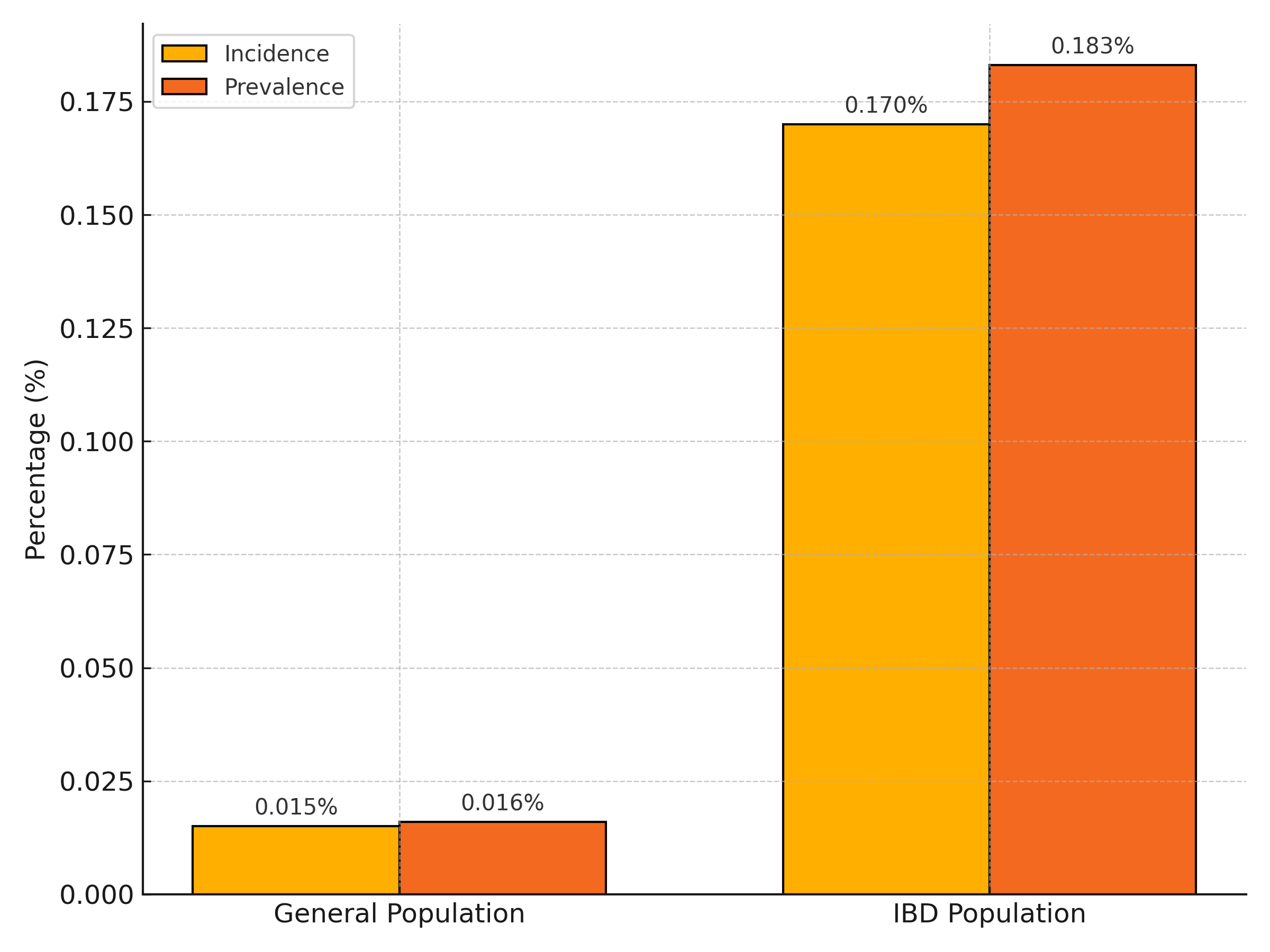
Figure: Figure 1. Elevated Rates of Vitamin A Deficiency in IBD Patients Compared to the General Population
Comparison of the incidence and prevalence of vitamin A deficiency (VAD) in patients with inflammatory bowel disease (IBD) versus the general population. VAD was over 11 times more common in the IBD cohort, highlighting a significant nutritional vulnerability in this group.
Disclosures:
Sabtain Saroya indicated no relevant financial relationships.
Armando Ugarte indicated no relevant financial relationships.
Matthew DeLeary indicated no relevant financial relationships.
Luke Nelson indicated no relevant financial relationships.
Kira Yates indicated no relevant financial relationships.
Mudasir Rashid indicated no relevant financial relationships.
Elizbeth Beyene indicated no relevant financial relationships.
Mekdem Bisrat indicated no relevant financial relationships.
Daniel Larbi indicated no relevant financial relationships.
Miriam Michael indicated no relevant financial relationships.
Sabtain Saroya, BS1, Armando Ugarte, 1, Matthew DeLeary, 1, Luke Nelson, 1, Kira Yates, 1, Mudasir Rashid, PhD2, Elizbeth Beyene, 2, Mekdem Bisrat, 1, Daniel Larbi, MD2, Miriam Michael, MD2. P3326 - Vitamin A Deficiency in IBD: A Large-Scale Population-Based Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1College of Medicine, Howard University, Washington, DC; 2Howard University Hospital, Washington, DC
Introduction: Vitamin A, present as preformed retinoids and provitamin A carotenoids, is essential for vision, epithelial integrity, immune regulation, and mucosal maintenance. Although rare in developed nations, vitamin A deficiency (VAD) can arise from malabsorption, hepatic dysfunction, or inadequate intake. Inflammatory bowel disease (IBD) may predispose individuals to VAD through chronic inflammation and impaired nutrient absorption. This study investigates the prevalence and demographic distribution of VAD in IBD patients across a large U.S. population.
Methods: We conducted a retrospective cohort study using the TriNetX Research Network, comprising over 163 million patient records. A total of 829,248 patients with IBD were identified. We compared the prevalence and incidence of VAD between IBD and non-IBD populations and analyzed demographic trends, including age, sex, and race/ethnicity.
Results: In the general population, VAD incidence was 0.015%, with a prevalence of 0.016%. Among IBD patients, the incidence increased to 0.17% and prevalence to 0.183%—representing an over 11-fold increase. Females accounted for 52.68% of IBD cases, and VAD was disproportionately more common among White female patients.
Discussion: The markedly higher burden of VAD in IBD patients highlights a critical intersection between chronic inflammation, malabsorption, and increased micronutrient demands. The observed demographic disparity—particularly among White females—suggests a multifactorial etiology involving genetic, hormonal, and dietary influences. These findings support the incorporation of routine vitamin A screening into IBD management protocols. Early identification and targeted supplementation could mitigate nutritional deficiencies, reduce complications, and optimize clinical outcomes. Future research should focus on elucidating the underlying mechanisms and evaluating the therapeutic impact of vitamin A repletion in this high-risk population.
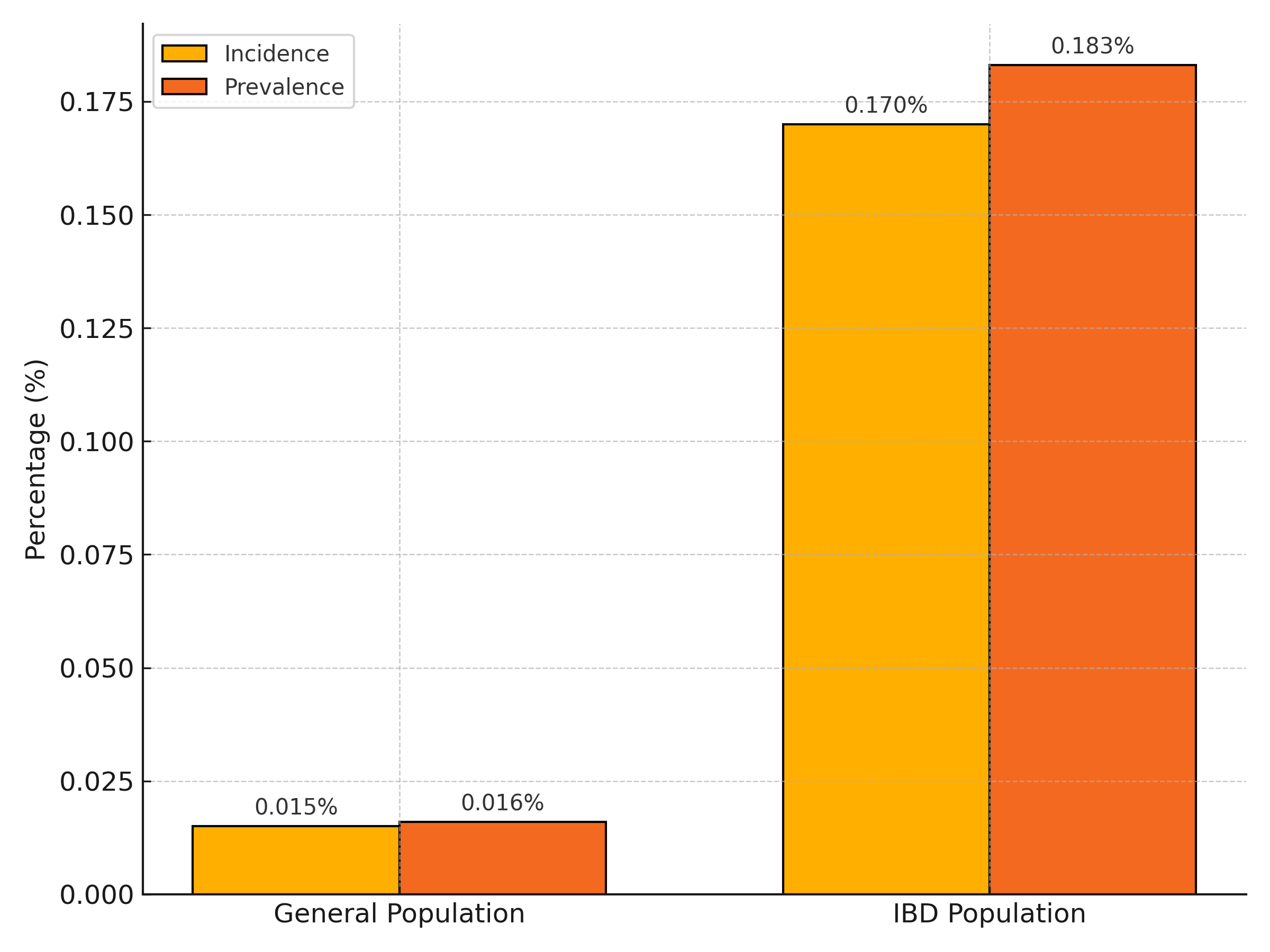
Figure: Figure 1. Elevated Rates of Vitamin A Deficiency in IBD Patients Compared to the General Population
Comparison of the incidence and prevalence of vitamin A deficiency (VAD) in patients with inflammatory bowel disease (IBD) versus the general population. VAD was over 11 times more common in the IBD cohort, highlighting a significant nutritional vulnerability in this group.
Disclosures:
Sabtain Saroya indicated no relevant financial relationships.
Armando Ugarte indicated no relevant financial relationships.
Matthew DeLeary indicated no relevant financial relationships.
Luke Nelson indicated no relevant financial relationships.
Kira Yates indicated no relevant financial relationships.
Mudasir Rashid indicated no relevant financial relationships.
Elizbeth Beyene indicated no relevant financial relationships.
Mekdem Bisrat indicated no relevant financial relationships.
Daniel Larbi indicated no relevant financial relationships.
Miriam Michael indicated no relevant financial relationships.
Sabtain Saroya, BS1, Armando Ugarte, 1, Matthew DeLeary, 1, Luke Nelson, 1, Kira Yates, 1, Mudasir Rashid, PhD2, Elizbeth Beyene, 2, Mekdem Bisrat, 1, Daniel Larbi, MD2, Miriam Michael, MD2. P3326 - Vitamin A Deficiency in IBD: A Large-Scale Population-Based Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
