Monday Poster Session
Category: IBD
P3316 - Influence of Social Determinants of Health on Peri- and Postoperative Crohn’s Disease
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Garrett J. Weskamp, MD (he/him/his)
University of Colorado Anschutz Medical Campus
Denver, CO
Presenting Author(s)
Garrett J. Weskamp, MD1, Camille Hcochheimer, PhD2, Shravya Pothula, MD3, Joseph M. Gaballa, MD4, Benjamin Click, MD, MS5
1University of Colorado Anschutz Medical Campus, Denver, CO; 2Colorado School of Public Health, Aurora, CO; 3University of Colorado Anschutz Medical Campus, Aurora, CO; 4University of Colorado Anschutz Medical Campus, Los Angeles, CA; 5University of Colorado, Denver, CO
Introduction: Social determinants of health (SDOH) significantly influence disease outcomes in inflammatory bowel disease (IBD). The Social Vulnerability Index (SVI) aggregates census-tract-level data to quantify a community’s social vulnerability. To determine the impact of SDOH on peri- and postoperative outcomes, we evaluated a cohort of Crohn’s disease (CD) patients undergoing ileocolonic resection (ICR) by SVI strata.
Methods: Using a single-center database of CD patients who underwent ICR, we geocoded patients' addresses to census tracts and matched them with SVI data. Patients were stratified into four SVI quartiles (low to high vulnerability). We compared demographics, perioperative disease features, and postoperative endoscopic, radiographic, and surgical recurrence across quartiles.
Results: 83 patients were included in the study; 66% had low or low-medium overall SVI percentile and 34% medium-high or high percentile. Sex and age at surgery and diagnosis were not significantly different by SVI quartile. Higher SVI was significantly associated with active smoking (21% vs 9%, p = 0.006). Examining disease characteristics, higher SVI was associated with perianal disease (32% vs 13%, p = 0.009) and urgent or emergent surgery timing (32% vs 11%, p = 0.024). Postoperative biologic prophylaxis was utilized in 53% of the cohort and median postop follow-up was 3.3 years with no difference by SVI quartile. Postop endoscopy monitoring was similar across SVI quartiles at 1 (61%), 3 (77%), and 5 years (81%) with no difference in endoscopic recurrence (p=0.28). Radiographic surveillance within 1 year post-ICR was significantly more frequent in higher SVI quartiles (32% vs 16%, p = 0.048) with higher rates of 1-year radiographic recurrence (14% vs 7%, p = 0.005). No differences in radiographic assessment or recurrence at 3 and 5 years were seen. Surgical recurrence was rare (4.8%) with no difference by SVI.
Discussion: Higher social vulnerability is associated with smoking, perianal disease, and more urgent surgical presentations in CD – indicators of complex and potentially delayed disease management. Fortunately, postoperative prophylaxis and endoscopic monitoring is evenly utilized across SVI quartiles. Postoperative radiographic assessments and disease activity may differ early but equilibrate. These findings underscore the need for targeted social risk screening and interventions to promote equitable outcomes in CD care, particularly modifiable risk factors such as smoking.
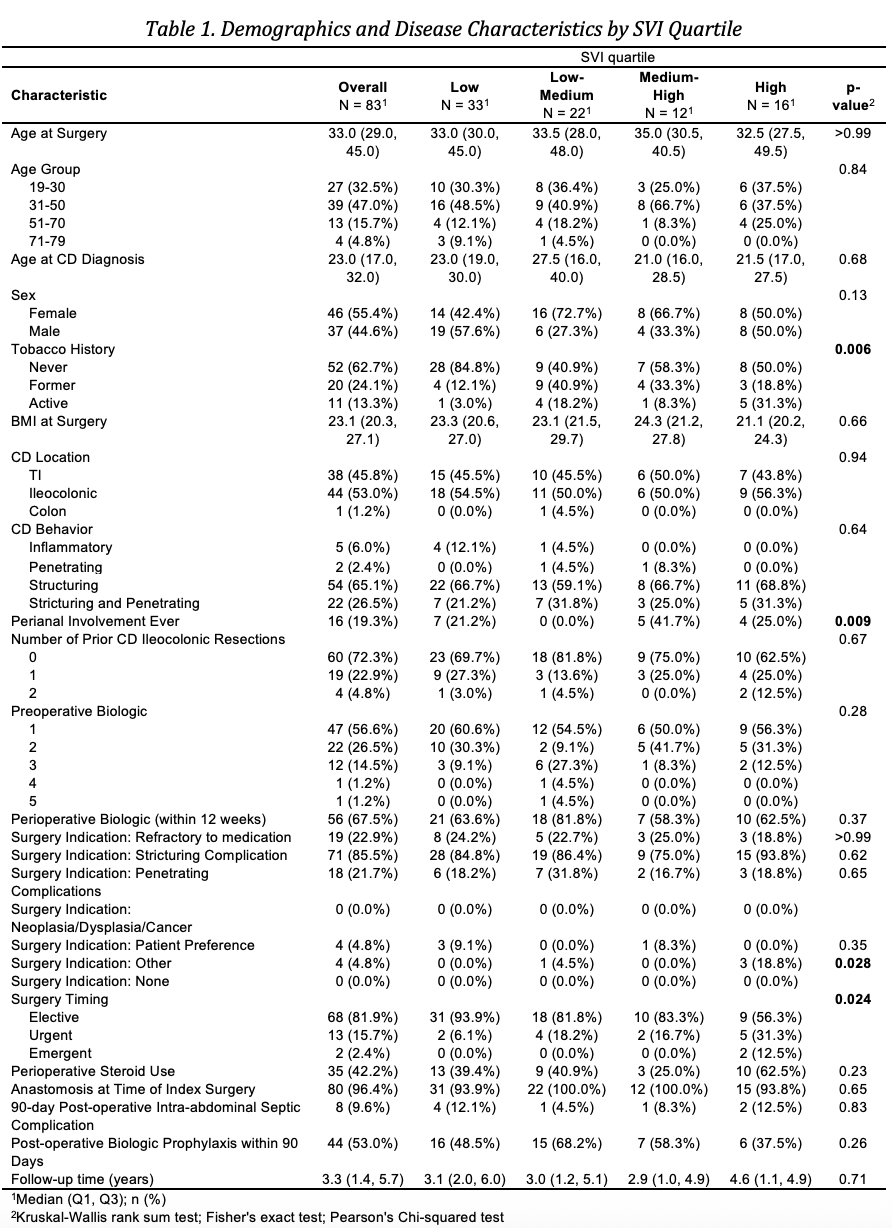
Figure: Demographics and Disease Characteristics by SVI Quartile
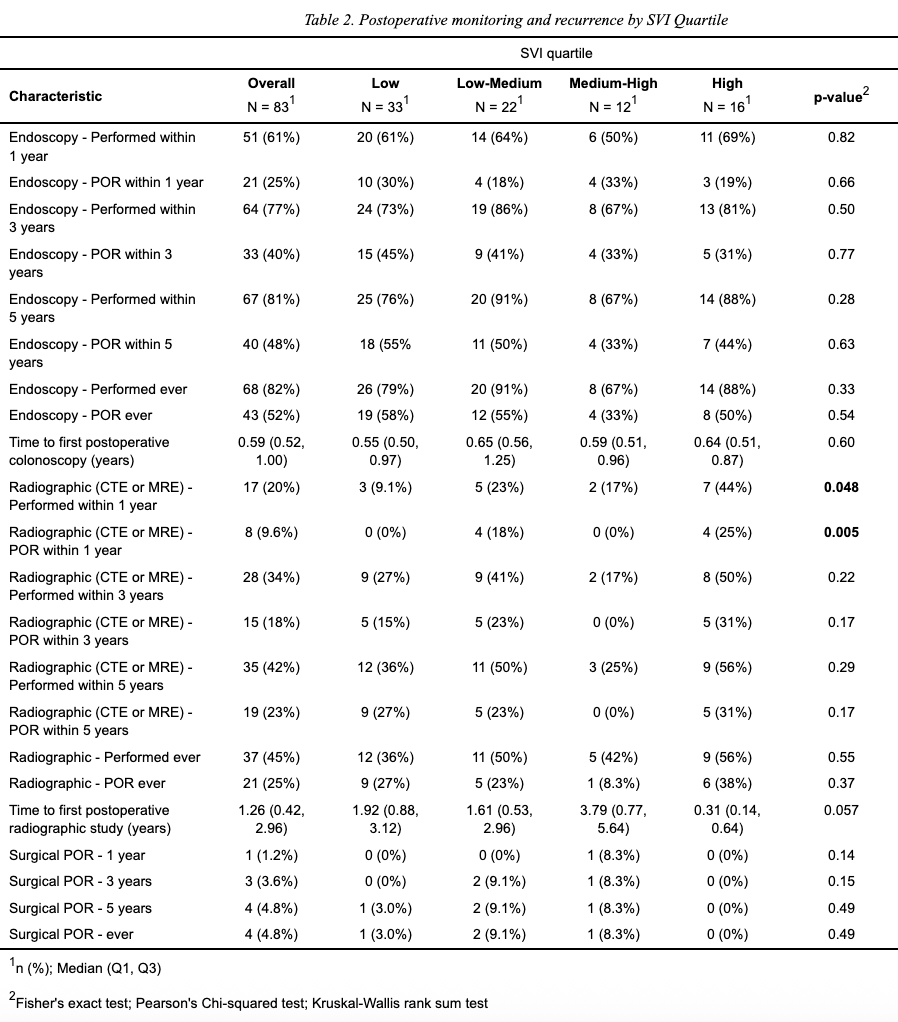
Figure: Postoperative monitoring and recurrence by SVI Quartile
Disclosures:
Garrett Weskamp indicated no relevant financial relationships.
Camille Hcochheimer indicated no relevant financial relationships.
Shravya Pothula indicated no relevant financial relationships.
Joseph Gaballa indicated no relevant financial relationships.
Benjamin Click indicated no relevant financial relationships.
Garrett J. Weskamp, MD1, Camille Hcochheimer, PhD2, Shravya Pothula, MD3, Joseph M. Gaballa, MD4, Benjamin Click, MD, MS5. P3316 - Influence of Social Determinants of Health on Peri- and Postoperative Crohn’s Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Colorado Anschutz Medical Campus, Denver, CO; 2Colorado School of Public Health, Aurora, CO; 3University of Colorado Anschutz Medical Campus, Aurora, CO; 4University of Colorado Anschutz Medical Campus, Los Angeles, CA; 5University of Colorado, Denver, CO
Introduction: Social determinants of health (SDOH) significantly influence disease outcomes in inflammatory bowel disease (IBD). The Social Vulnerability Index (SVI) aggregates census-tract-level data to quantify a community’s social vulnerability. To determine the impact of SDOH on peri- and postoperative outcomes, we evaluated a cohort of Crohn’s disease (CD) patients undergoing ileocolonic resection (ICR) by SVI strata.
Methods: Using a single-center database of CD patients who underwent ICR, we geocoded patients' addresses to census tracts and matched them with SVI data. Patients were stratified into four SVI quartiles (low to high vulnerability). We compared demographics, perioperative disease features, and postoperative endoscopic, radiographic, and surgical recurrence across quartiles.
Results: 83 patients were included in the study; 66% had low or low-medium overall SVI percentile and 34% medium-high or high percentile. Sex and age at surgery and diagnosis were not significantly different by SVI quartile. Higher SVI was significantly associated with active smoking (21% vs 9%, p = 0.006). Examining disease characteristics, higher SVI was associated with perianal disease (32% vs 13%, p = 0.009) and urgent or emergent surgery timing (32% vs 11%, p = 0.024). Postoperative biologic prophylaxis was utilized in 53% of the cohort and median postop follow-up was 3.3 years with no difference by SVI quartile. Postop endoscopy monitoring was similar across SVI quartiles at 1 (61%), 3 (77%), and 5 years (81%) with no difference in endoscopic recurrence (p=0.28). Radiographic surveillance within 1 year post-ICR was significantly more frequent in higher SVI quartiles (32% vs 16%, p = 0.048) with higher rates of 1-year radiographic recurrence (14% vs 7%, p = 0.005). No differences in radiographic assessment or recurrence at 3 and 5 years were seen. Surgical recurrence was rare (4.8%) with no difference by SVI.
Discussion: Higher social vulnerability is associated with smoking, perianal disease, and more urgent surgical presentations in CD – indicators of complex and potentially delayed disease management. Fortunately, postoperative prophylaxis and endoscopic monitoring is evenly utilized across SVI quartiles. Postoperative radiographic assessments and disease activity may differ early but equilibrate. These findings underscore the need for targeted social risk screening and interventions to promote equitable outcomes in CD care, particularly modifiable risk factors such as smoking.
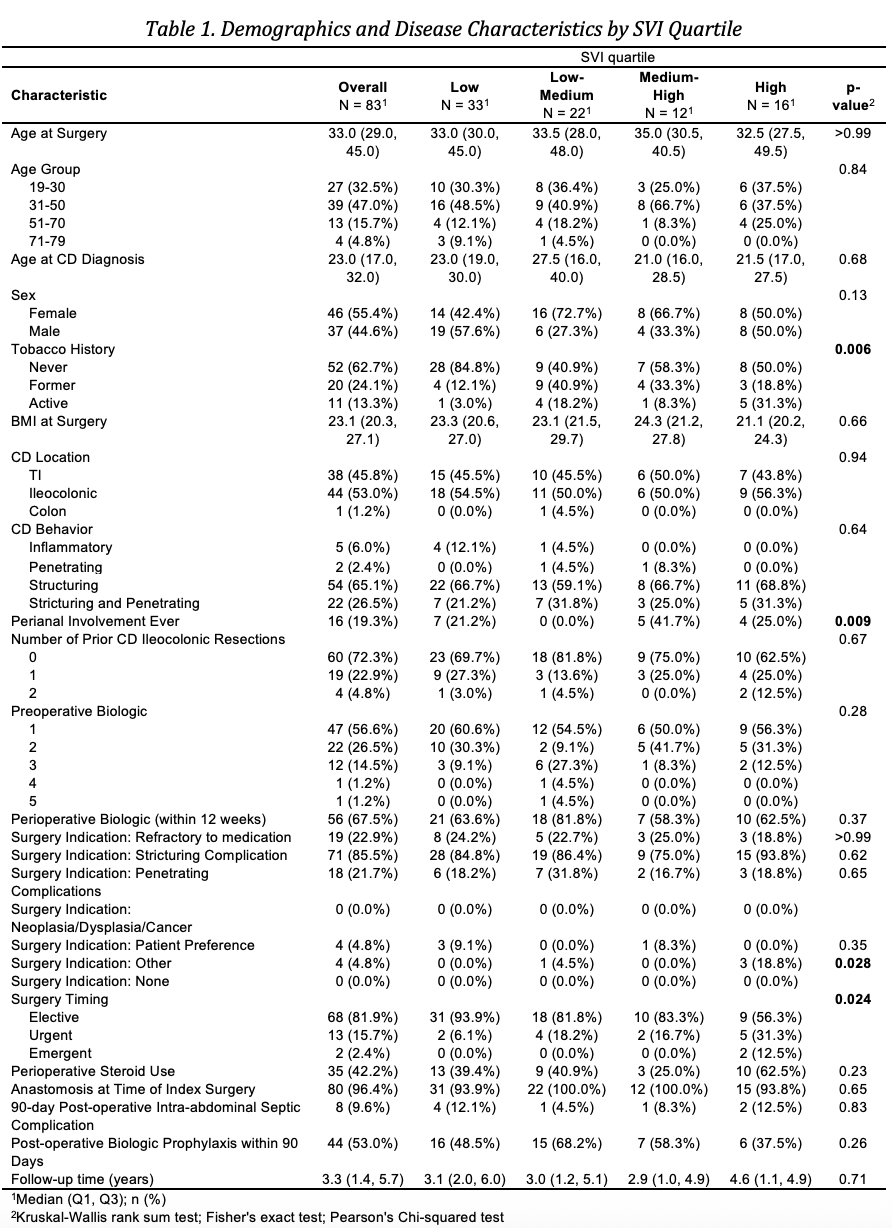
Figure: Demographics and Disease Characteristics by SVI Quartile
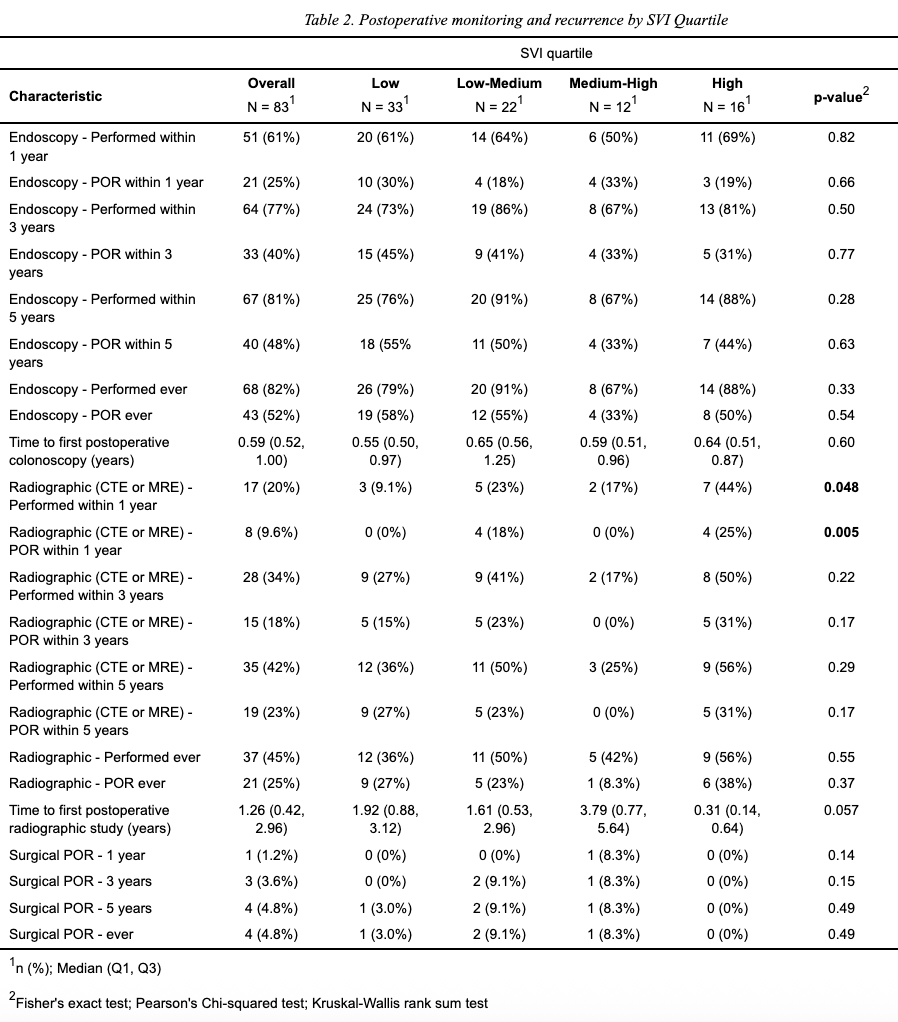
Figure: Postoperative monitoring and recurrence by SVI Quartile
Disclosures:
Garrett Weskamp indicated no relevant financial relationships.
Camille Hcochheimer indicated no relevant financial relationships.
Shravya Pothula indicated no relevant financial relationships.
Joseph Gaballa indicated no relevant financial relationships.
Benjamin Click indicated no relevant financial relationships.
Garrett J. Weskamp, MD1, Camille Hcochheimer, PhD2, Shravya Pothula, MD3, Joseph M. Gaballa, MD4, Benjamin Click, MD, MS5. P3316 - Influence of Social Determinants of Health on Peri- and Postoperative Crohn’s Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

