Monday Poster Session
Category: IBD
P3259 - Ulcerative Colitis with Comorbid Osteoporosis: A Retrospective Analysis of Inpatient Outcomes and Healthcare Utilization
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Anwar Uddin, MD (he/him/his)
SUNY Downstate Health Sciences University
Brooklyn, NY
Presenting Author(s)
Anwar Uddin, MD, Madia Ahad, MD, Rafat Uddin, MS, Peter Lymberopoulos, MD, Savanna Thor, DO, MPH
SUNY Downstate Health Sciences University, Brooklyn, NY
Introduction: Ulcerative colitis (UC) is a chronic inflammatory bowel disease often requiring hospitalization for disease flares and complications. Patients with UC are at increased risk for osteoporosis due to chronic inflammation, corticosteroid exposure, malnutrition, and reduced mobility. However, the impact of osteoporosis on hospitalization outcomes in this population remains poorly understood. This study aimed to evaluate clinical outcomes among hospitalized adults with UC, comparing those with and without a comorbid diagnosis of osteoporosis.
Methods: We conducted a retrospective cohort study using the National Inpatient Sample (2016–2020). Adults ≥18 years with ulcerative colitis (ICD-10 K51.00–K51.919) listed among the first 10 discharge diagnoses were included. Patients were stratified by comorbid osteoporosis (ICD-10 M81.0, M81.6, M81.8, M80.0, M80.8). Outcomes included mortality, LOS, cost, GI bleeding, fractures, malnutrition, anemia, and electrolyte derangements. Multivariable logistic regression adjusted for age, sex, race, and Charlson Comorbidity Index. Costs were modeled using gamma regression with log-link and adjusted to 2020 USD using the Consumer Price Index.
Results: Among patients hospitalized with UC, those with comorbid osteoporosis had a higher mean hospital cost ($16,476.7 vs. $14,900.5; OR 1.09, 95% CI 1.05–1.13) and increased odds of fractures (1.0% vs. 0.2%; OR 2.96, 95% CI 1.99–4.41) and malnutrition (10.0% vs. 8.1%; OR 1.30, 95% CI 1.17–1.46). Conversely, these patients had lower odds of gastrointestinal bleeding (2.2% vs. 3.8%; OR 0.61, 95% CI 0.49–0.76) and inpatient mortality (1.5% vs. 1.3%; OR 0.69, 95% CI 0.53–0.91). There were no significant differences in length of stay (5.3 vs. 5.2 days; OR 0.99, 95% CI 0.96–1.03) or anemia rates (17% vs. 19%; OR 1.00, 95% CI 0.91–1.09). Electrolyte derangements were slightly less common in the osteoporosis group (29% in both groups; OR 0.86, 95% CI 0.80–0.93).
Discussion: Hospitalized UC patients with comorbid osteoporosis experienced higher inpatient costs and increased rates of fractures and malnutrition, along with lower odds of gastrointestinal bleeding, inpatient mortality, and electrolyte abnormalities. No differences were observed in length of stay or anemia. Further study is needed to evaluate causal factors and potential interventions to improve outcomes in this subgroup.
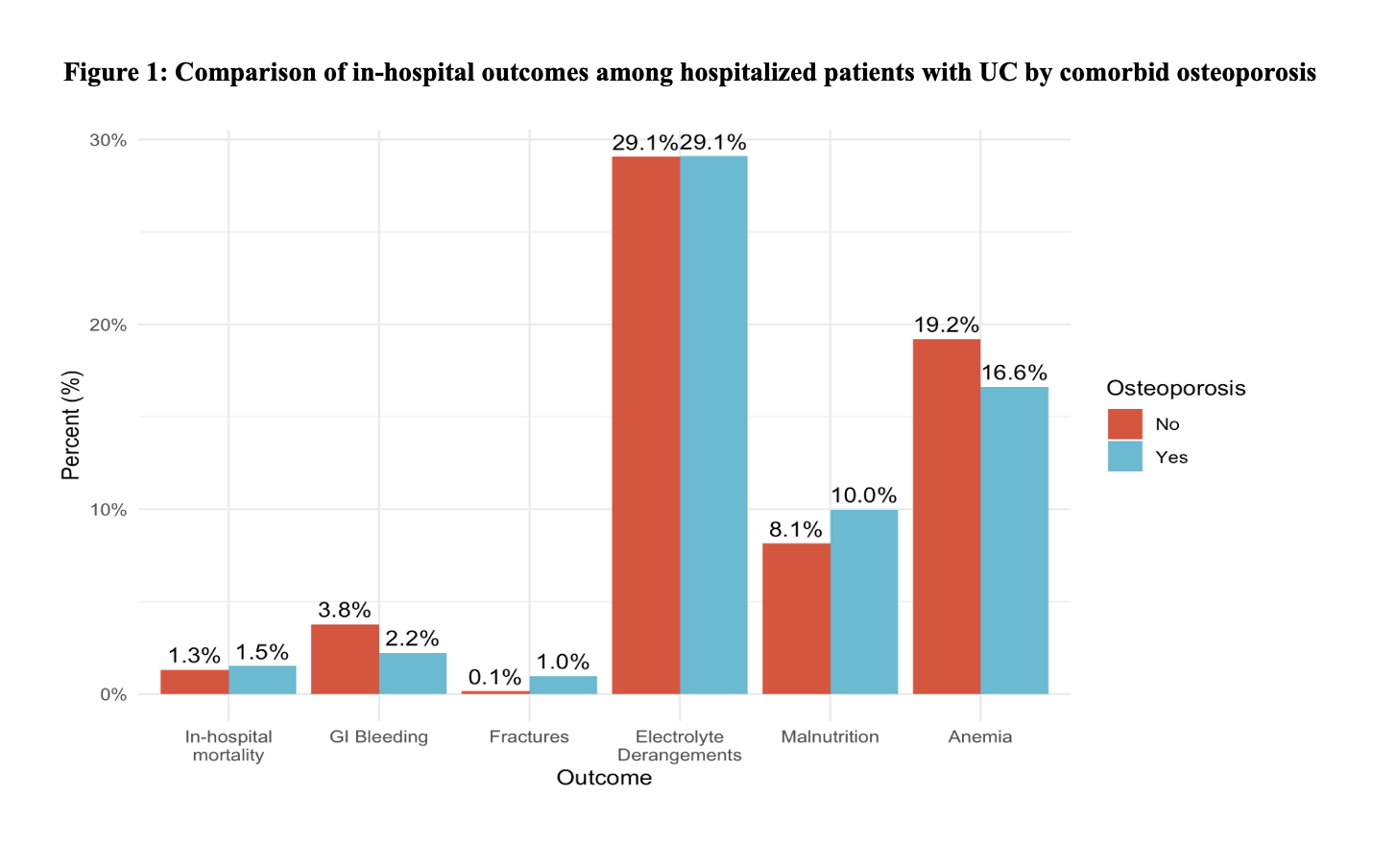
Figure: Table 1: Comparison of in-hospital outcomes among hospitalized patients with UC by comorbid osteoporosis
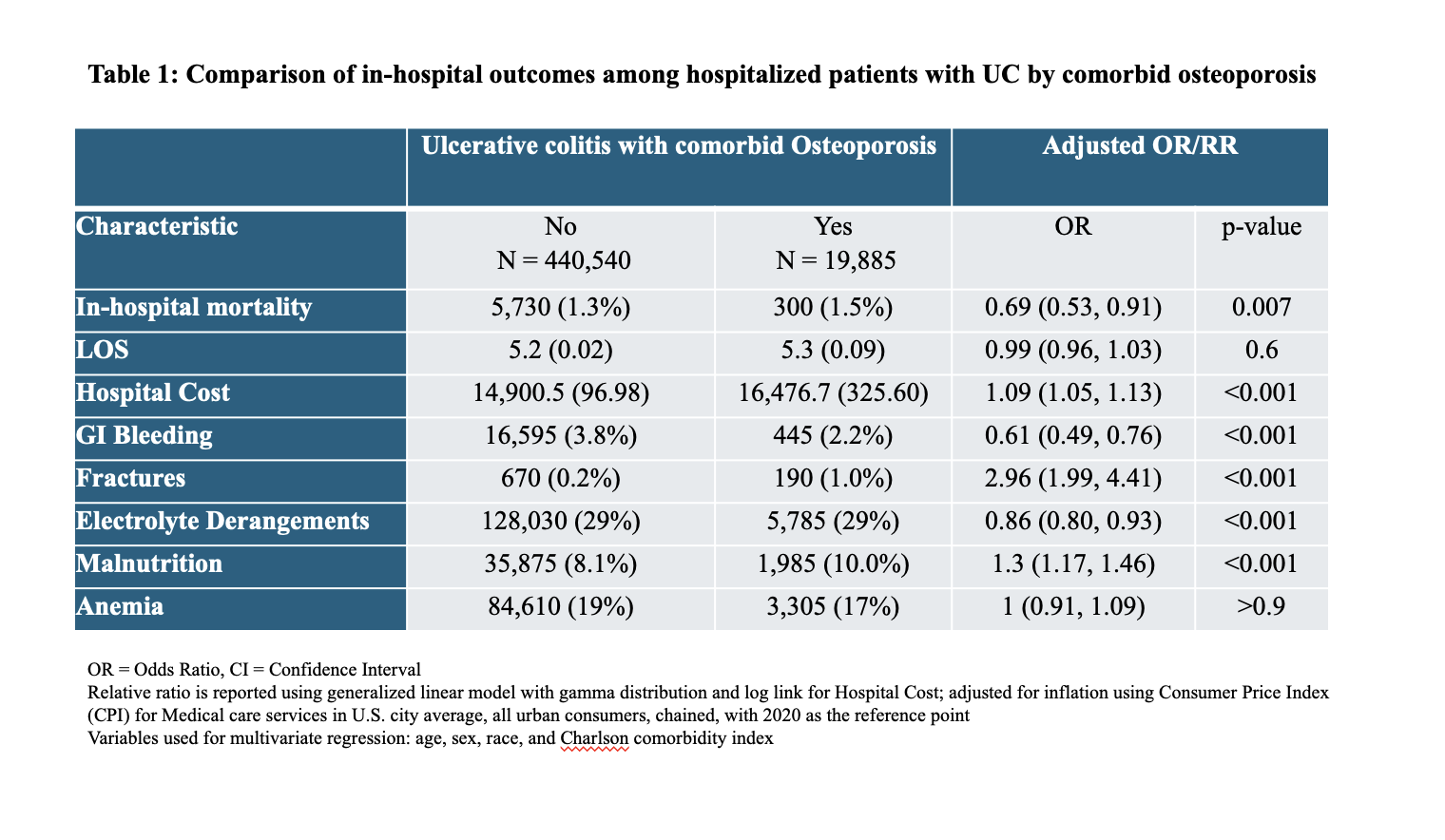
Figure: Figure 1: Bar Chart of in-hospital outcomes among hospitalized patients with UC by comorbid osteoporosis
Disclosures:
Anwar Uddin indicated no relevant financial relationships.
Madia Ahad indicated no relevant financial relationships.
Rafat Uddin indicated no relevant financial relationships.
Peter Lymberopoulos indicated no relevant financial relationships.
Savanna Thor indicated no relevant financial relationships.
Anwar Uddin, MD, Madia Ahad, MD, Rafat Uddin, MS, Peter Lymberopoulos, MD, Savanna Thor, DO, MPH. P3259 - Ulcerative Colitis with Comorbid Osteoporosis: A Retrospective Analysis of Inpatient Outcomes and Healthcare Utilization, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
SUNY Downstate Health Sciences University, Brooklyn, NY
Introduction: Ulcerative colitis (UC) is a chronic inflammatory bowel disease often requiring hospitalization for disease flares and complications. Patients with UC are at increased risk for osteoporosis due to chronic inflammation, corticosteroid exposure, malnutrition, and reduced mobility. However, the impact of osteoporosis on hospitalization outcomes in this population remains poorly understood. This study aimed to evaluate clinical outcomes among hospitalized adults with UC, comparing those with and without a comorbid diagnosis of osteoporosis.
Methods: We conducted a retrospective cohort study using the National Inpatient Sample (2016–2020). Adults ≥18 years with ulcerative colitis (ICD-10 K51.00–K51.919) listed among the first 10 discharge diagnoses were included. Patients were stratified by comorbid osteoporosis (ICD-10 M81.0, M81.6, M81.8, M80.0, M80.8). Outcomes included mortality, LOS, cost, GI bleeding, fractures, malnutrition, anemia, and electrolyte derangements. Multivariable logistic regression adjusted for age, sex, race, and Charlson Comorbidity Index. Costs were modeled using gamma regression with log-link and adjusted to 2020 USD using the Consumer Price Index.
Results: Among patients hospitalized with UC, those with comorbid osteoporosis had a higher mean hospital cost ($16,476.7 vs. $14,900.5; OR 1.09, 95% CI 1.05–1.13) and increased odds of fractures (1.0% vs. 0.2%; OR 2.96, 95% CI 1.99–4.41) and malnutrition (10.0% vs. 8.1%; OR 1.30, 95% CI 1.17–1.46). Conversely, these patients had lower odds of gastrointestinal bleeding (2.2% vs. 3.8%; OR 0.61, 95% CI 0.49–0.76) and inpatient mortality (1.5% vs. 1.3%; OR 0.69, 95% CI 0.53–0.91). There were no significant differences in length of stay (5.3 vs. 5.2 days; OR 0.99, 95% CI 0.96–1.03) or anemia rates (17% vs. 19%; OR 1.00, 95% CI 0.91–1.09). Electrolyte derangements were slightly less common in the osteoporosis group (29% in both groups; OR 0.86, 95% CI 0.80–0.93).
Discussion: Hospitalized UC patients with comorbid osteoporosis experienced higher inpatient costs and increased rates of fractures and malnutrition, along with lower odds of gastrointestinal bleeding, inpatient mortality, and electrolyte abnormalities. No differences were observed in length of stay or anemia. Further study is needed to evaluate causal factors and potential interventions to improve outcomes in this subgroup.
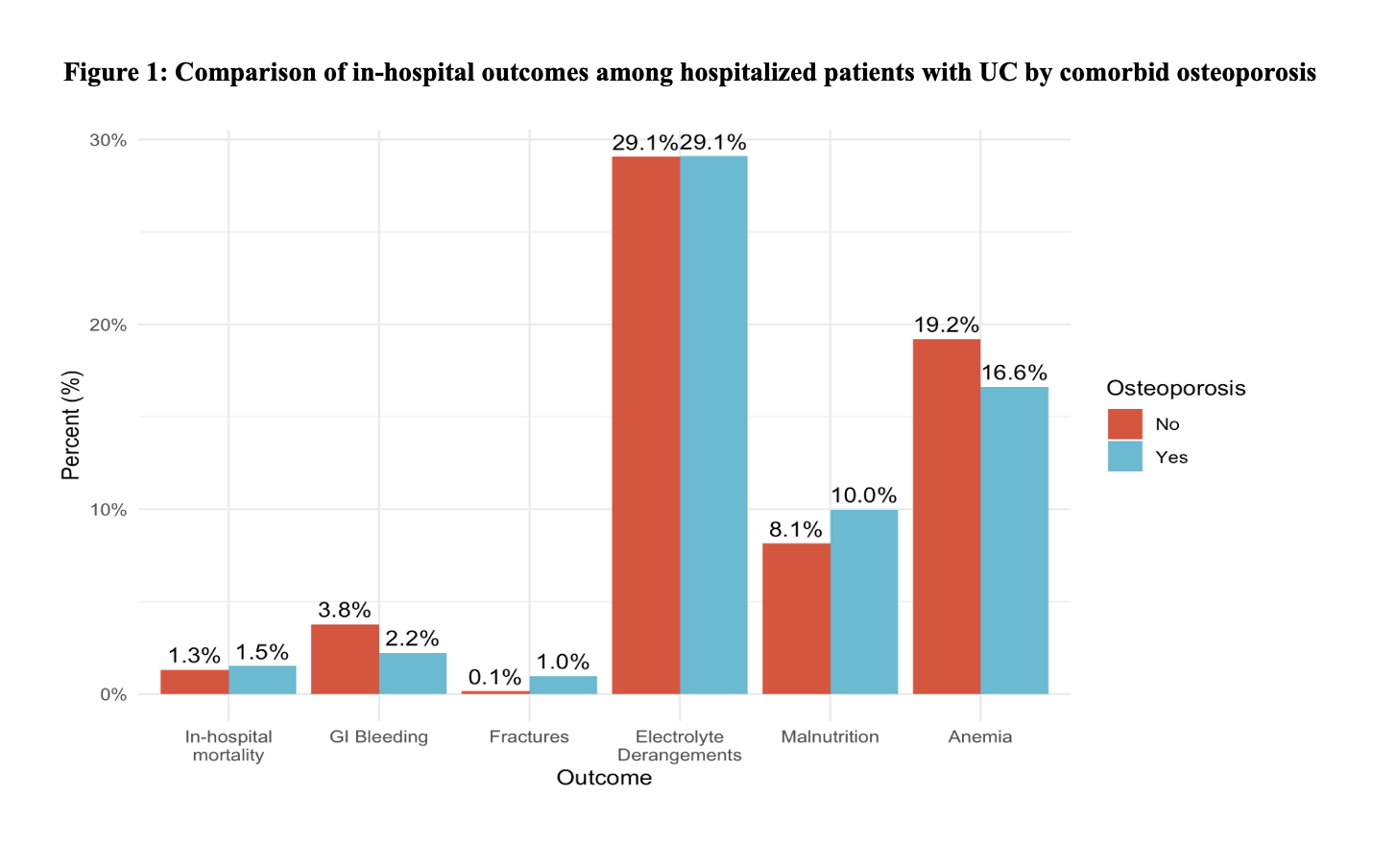
Figure: Table 1: Comparison of in-hospital outcomes among hospitalized patients with UC by comorbid osteoporosis
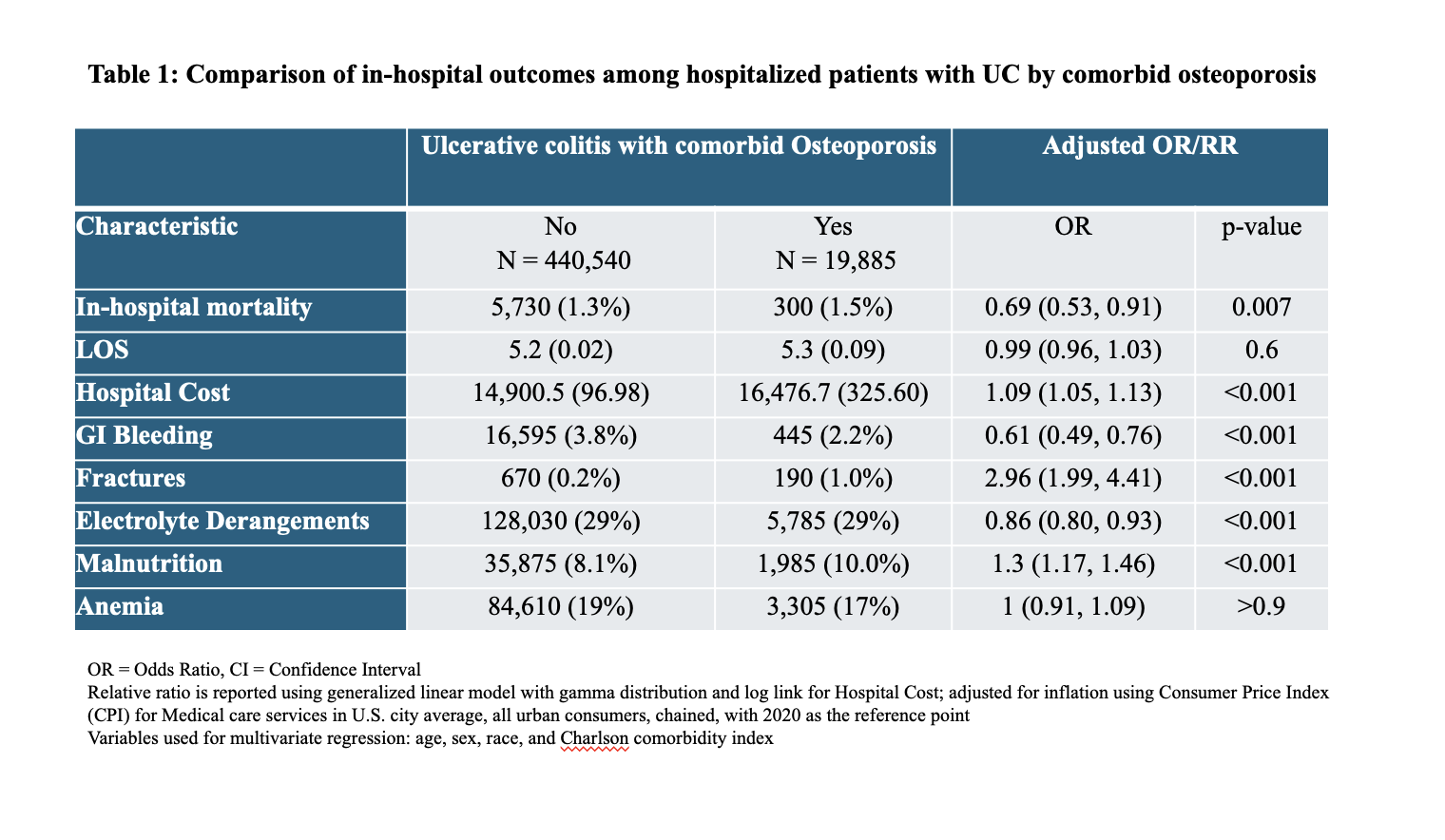
Figure: Figure 1: Bar Chart of in-hospital outcomes among hospitalized patients with UC by comorbid osteoporosis
Disclosures:
Anwar Uddin indicated no relevant financial relationships.
Madia Ahad indicated no relevant financial relationships.
Rafat Uddin indicated no relevant financial relationships.
Peter Lymberopoulos indicated no relevant financial relationships.
Savanna Thor indicated no relevant financial relationships.
Anwar Uddin, MD, Madia Ahad, MD, Rafat Uddin, MS, Peter Lymberopoulos, MD, Savanna Thor, DO, MPH. P3259 - Ulcerative Colitis with Comorbid Osteoporosis: A Retrospective Analysis of Inpatient Outcomes and Healthcare Utilization, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
