Monday Poster Session
Category: IBD
P3258 - Human Papilloma Virus and Cervical Cancer Risk in Inflammatory Bowel Disease: Implications for Screening and Prevention in Women
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Pooja Viswanath, MS, DO
University of New Mexico Health Sciences Center
Albuquerque, NM
Presenting Author(s)
Pooja Viswanath, MS, DO1, Ahmed Telbany, MD2, Niven Wang, DO3, Abhishek Patel, MD1, Evelyn Inga, MD2, Swathi Paleti, MD1
1University of New Mexico Health Sciences Center, Albuquerque, NM; 2University of New Mexico, Albuquerque, NM; 3University of New Mexico Hospital, Albuquerque, NM
Introduction: Inflammatory bowel disease (IBD), including ulcerative colitis (UC) and Crohn’s disease (CD), is a chronic, immune-mediated disorder affecting the gastrointestinal (GI) tract. Long-term immunosuppressive therapy can increase infection susceptibility. Although women with IBD have a higher risk for cervical cancer, HPV vaccination rates remain suboptimal. This may be influenced by general vaccine hesitancy, exacerbated by the rise of the anti-vaccine movement. This study evaluates HPV prevalence and HPV related outcomes in women with and without IBD, stratified by vaccination status.
Methods: This retrospective study was performed using TriNetX from January 1st, 2007- September 30th, 2024. The IBD cohort included females aged 18-45 with ≥ 2 ICD-10 codes for UC or CD and ≥ 1 IBD-related medication. Controls were age-matched females without autoimmune disease. HPV infection was identified using ICD-10-CM codes for positive HPV laboratory test results. HPV-related complications, including cervical dysplasia, cervical cancer and anogenital warts were identified using ICD-10-CM codes. Statistical analyses included descriptive statistics, logistic regression-based 1:1 propensity score matching to control for key covariates, and post-matching comparisons of HPV infection and complication rates, reported as adjusted odds ratios (aOR) with 95% confidence intervals, to assess the impact of HPV vaccination in IBD and non-IBD cohorts.
Results: After matching, 4,821 women were included in each cohort. HPV vaccination was slightly more common in IBD patients (6.4% vs. 6.2%). Women with IBD had lower rates of cervical dysplasia (1.7% vs. 2.9%, aOR 1.70, 95% CI: 1.29–2.24, p< 0.001). Cervical neoplasm occurred equally in both groups at 0.2% (aOR 1.00, 95% CI: 0.42–2.41, p= 0.999). Anogenital wart rates were lower in IBD women (0.5% vs. 0.7%, aOR 1.41, 95% CI: 0.84–2.35, p= 0.194), though not significant.
Discussion: Contrary to expectation, HPV vaccination rates were marginally higher among women with IBD. IBD patients also had significantly lower cervical dysplasia rates. This may be due to more frequent interactions with specialists, better access to preventative care and increased awareness of infection risks in immunosuppressed populations. Equal rates of cervical neoplasm and non-significant differences in anogenital warts underscore the complexity of HPV-related disease. These findings emphasize the need to counteract vaccine hesitancy with targeted education, particularly in high-risk groups.
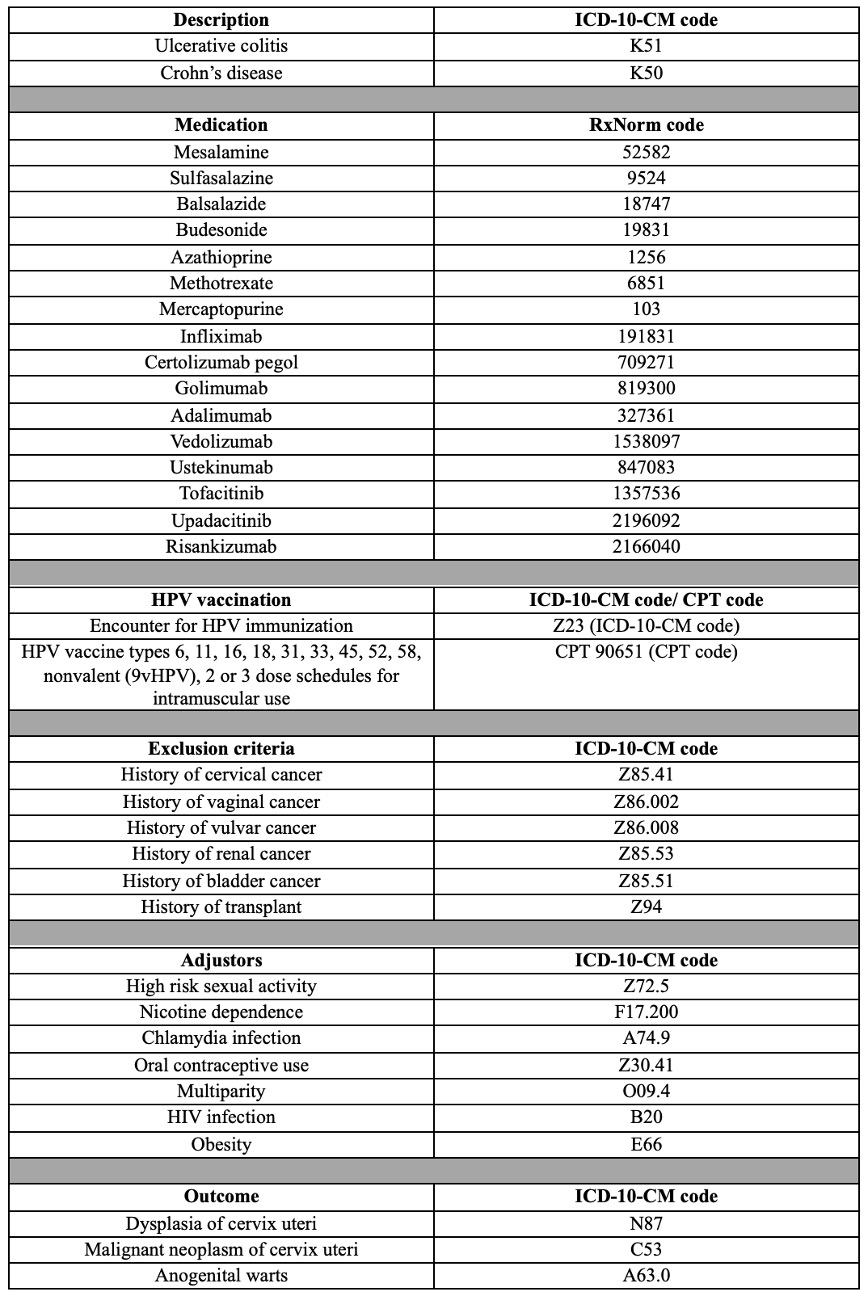
Figure: Table 1: List of ICD-10-CM, RxNorm and CPT codes used in cohort identification and outcome definition.
Disclosures:
Pooja Viswanath indicated no relevant financial relationships.
Ahmed Telbany indicated no relevant financial relationships.
Niven Wang indicated no relevant financial relationships.
Abhishek Patel indicated no relevant financial relationships.
Evelyn Inga indicated no relevant financial relationships.
Swathi Paleti indicated no relevant financial relationships.
Pooja Viswanath, MS, DO1, Ahmed Telbany, MD2, Niven Wang, DO3, Abhishek Patel, MD1, Evelyn Inga, MD2, Swathi Paleti, MD1. P3258 - Human Papilloma Virus and Cervical Cancer Risk in Inflammatory Bowel Disease: Implications for Screening and Prevention in Women, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of New Mexico Health Sciences Center, Albuquerque, NM; 2University of New Mexico, Albuquerque, NM; 3University of New Mexico Hospital, Albuquerque, NM
Introduction: Inflammatory bowel disease (IBD), including ulcerative colitis (UC) and Crohn’s disease (CD), is a chronic, immune-mediated disorder affecting the gastrointestinal (GI) tract. Long-term immunosuppressive therapy can increase infection susceptibility. Although women with IBD have a higher risk for cervical cancer, HPV vaccination rates remain suboptimal. This may be influenced by general vaccine hesitancy, exacerbated by the rise of the anti-vaccine movement. This study evaluates HPV prevalence and HPV related outcomes in women with and without IBD, stratified by vaccination status.
Methods: This retrospective study was performed using TriNetX from January 1st, 2007- September 30th, 2024. The IBD cohort included females aged 18-45 with ≥ 2 ICD-10 codes for UC or CD and ≥ 1 IBD-related medication. Controls were age-matched females without autoimmune disease. HPV infection was identified using ICD-10-CM codes for positive HPV laboratory test results. HPV-related complications, including cervical dysplasia, cervical cancer and anogenital warts were identified using ICD-10-CM codes. Statistical analyses included descriptive statistics, logistic regression-based 1:1 propensity score matching to control for key covariates, and post-matching comparisons of HPV infection and complication rates, reported as adjusted odds ratios (aOR) with 95% confidence intervals, to assess the impact of HPV vaccination in IBD and non-IBD cohorts.
Results: After matching, 4,821 women were included in each cohort. HPV vaccination was slightly more common in IBD patients (6.4% vs. 6.2%). Women with IBD had lower rates of cervical dysplasia (1.7% vs. 2.9%, aOR 1.70, 95% CI: 1.29–2.24, p< 0.001). Cervical neoplasm occurred equally in both groups at 0.2% (aOR 1.00, 95% CI: 0.42–2.41, p= 0.999). Anogenital wart rates were lower in IBD women (0.5% vs. 0.7%, aOR 1.41, 95% CI: 0.84–2.35, p= 0.194), though not significant.
Discussion: Contrary to expectation, HPV vaccination rates were marginally higher among women with IBD. IBD patients also had significantly lower cervical dysplasia rates. This may be due to more frequent interactions with specialists, better access to preventative care and increased awareness of infection risks in immunosuppressed populations. Equal rates of cervical neoplasm and non-significant differences in anogenital warts underscore the complexity of HPV-related disease. These findings emphasize the need to counteract vaccine hesitancy with targeted education, particularly in high-risk groups.
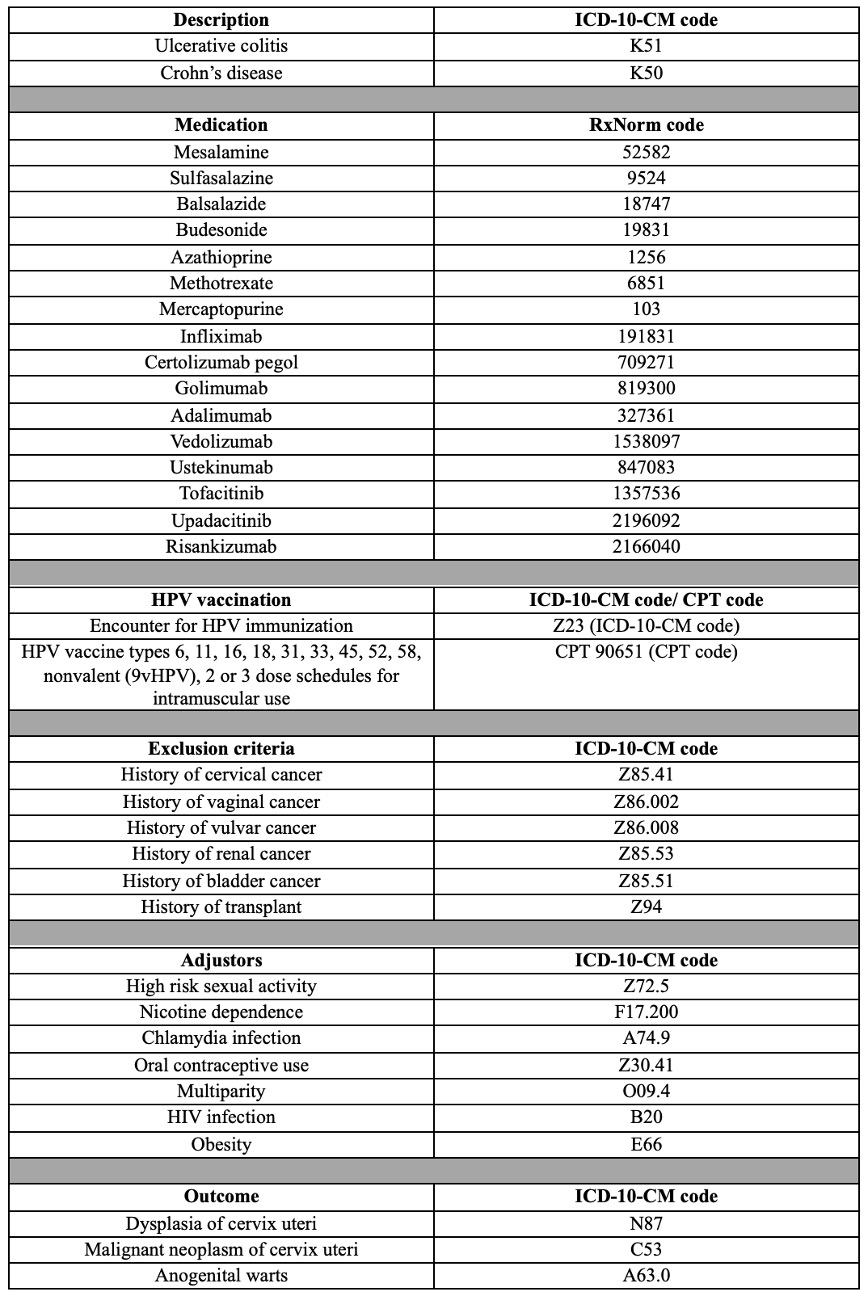
Figure: Table 1: List of ICD-10-CM, RxNorm and CPT codes used in cohort identification and outcome definition.
Disclosures:
Pooja Viswanath indicated no relevant financial relationships.
Ahmed Telbany indicated no relevant financial relationships.
Niven Wang indicated no relevant financial relationships.
Abhishek Patel indicated no relevant financial relationships.
Evelyn Inga indicated no relevant financial relationships.
Swathi Paleti indicated no relevant financial relationships.
Pooja Viswanath, MS, DO1, Ahmed Telbany, MD2, Niven Wang, DO3, Abhishek Patel, MD1, Evelyn Inga, MD2, Swathi Paleti, MD1. P3258 - Human Papilloma Virus and Cervical Cancer Risk in Inflammatory Bowel Disease: Implications for Screening and Prevention in Women, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
