Monday Poster Session
Category: IBD
P3233 - Prevalence and Impact of Prediabetes on Cardiovascular and Cerebrovascular Outcomes in Inflammatory Bowel Disease: A Population-Based Nationwide Analysis (2022)
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Pranay T. Vaghela, MBBS (he/him/his)
The Maharaja Sayajirao University of Baroda
Navsari, Gujarat, India
Presenting Author(s)
Pranay T. Vaghela, MBBS1, Rohan Raj, MBBS2, Jithin Kolli, MBBS3, Jyoti Yadav, MBBS4, Yousuf Hassan Syed, MD5, Nandini Hemant. Patel, MBBS6, Hari Priya Nistala, MBBS7, Rupak Desai, MBBS8
1The Maharaja Sayajirao University of Baroda, Navsari, Gujarat, India; 2Memorial Hospital at Gulfport, Gulfport, MS; 3JSS MEDICAL COLLEGE, Andra Pradesh, Andhra Pradesh, India; 4JSS Medical college, Mysore, Karnataka, India; 5Team Health, Las Vegas, NV; 6Pramukhswami Medical College, Gujarat, India, Anand, Gujarat, India; 7Maharajah's Institute of Medical Sciences, Leander, TX; 8Independent Outcomes Researcher, Atlanta, GA
Introduction: While inflammatory bowel disease (IBD) is known to increase cardiovascular risk and its association with diabetes has been evaluated before, large-scale data on the burden and impact of prediabetes (pDM) in this population remain unclear. This study aimed to evaluate the burden of pDM in IBD-related hospitalizations and its association with cardiovascular and cerebrovascular events using a population-based analysis.
Methods: Using ICD-10 codes, we conducted a retrospective analysis of the 2022 National Inpatient Sample (NIS) including adult IBD hospitalizations without established diabetes. Patients were stratified by pDM status. Baseline demographics and comorbidities were compared, and multivariable logistic regression assessed odds ratios (OR) for acute myocardial infarction (AMI), ischemic stroke (AIS), atrial fibrillation (AF), venous thromboembolism (VTE), cardiac arrest, and in-hospital mortality. Subgroup analysis was performed for younger [18-44] IBD patients. A p value < 0.05 was considered statistically significant.
Results: Of 259,505 adult IBD hospitalizations, 3,220 (1.2%) had a concurrent diagnosis of pDM. Patients with pDM were older (median age 63 vs. 54), more likely to be male (46.1% vs. 42.8%), and had higher prevalence among Black (14.4% vs. 11.2%) and Hispanic (11.3% vs. 7.1%) groups. Patients with pDM had higher comorbidity burdens, including chronic pulmonary disease (25.3% vs. 19.6%), complicated hypertension (18.1% vs. 13.9%), and smoking history (43.1% vs. 37.1%). In the full cohort, pDM was independently associated with increased odds of AMI (OR 1.91; 95% CI: 1.29-2.82; p< 0.001) and AIS (OR 2.14; 95% CI: 1.25-3.67; p=0.006). Other outcomes including AF, VTE, cardiac arrest, and in-hospital mortality were not significantly different. Among younger patients, no outcome reached significance, though AIS showed a trend (OR 6.88; p=0.052).
Discussion: Prediabetes is uncommon among IBD hospitalizations but is associated with significantly increased cardiovascular and cerebrovascular risk. These findings highlight the importance of early metabolic risk screening and intervention in this population.
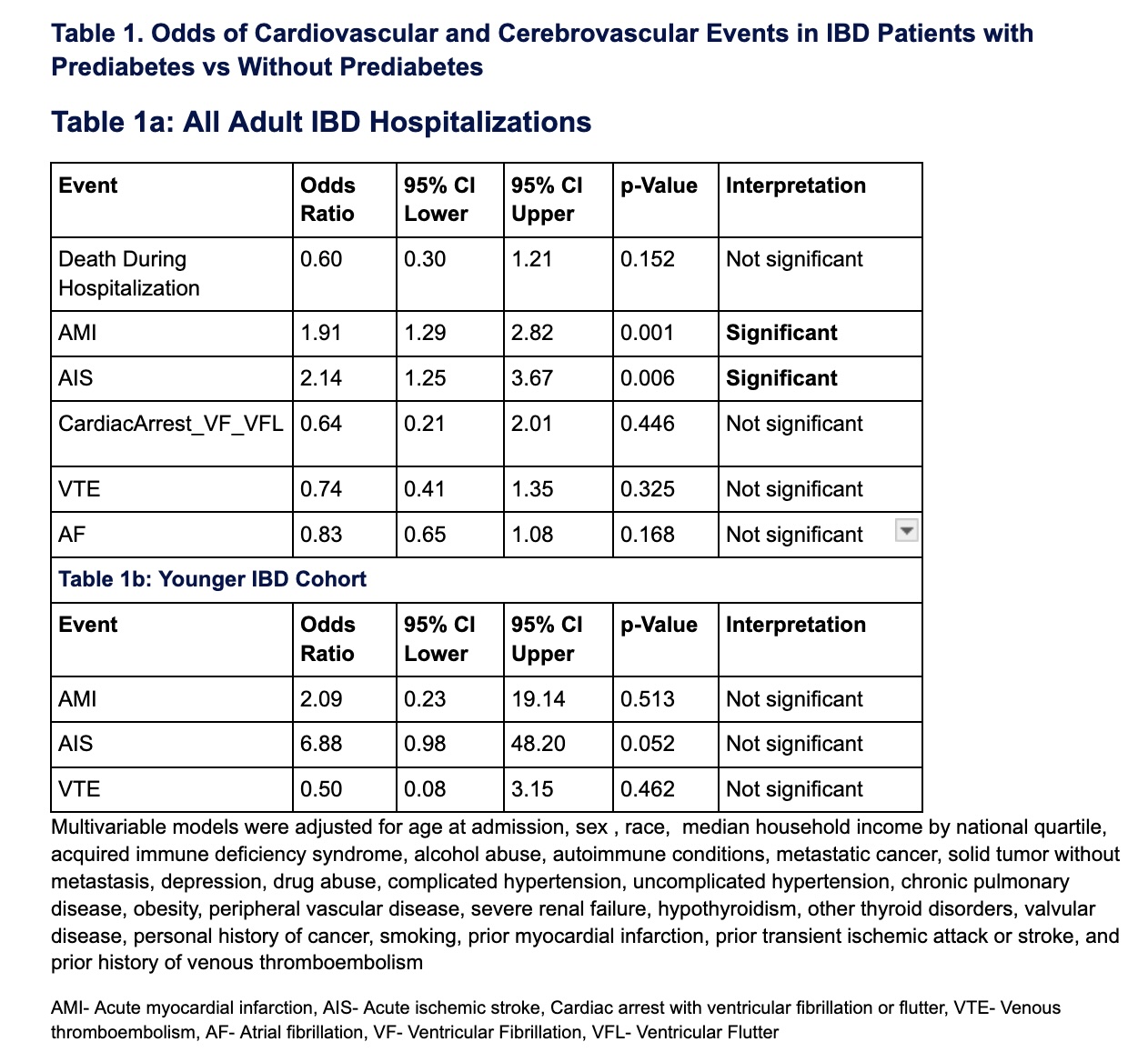
Figure: Table 1. Odds of cardiovascular and cerebroovascular events in IBD patients with prediabetes v/s without prediabetes.
Disclosures:
Pranay Vaghela indicated no relevant financial relationships.
Rohan Raj indicated no relevant financial relationships.
Jithin Kolli indicated no relevant financial relationships.
Jyoti Yadav indicated no relevant financial relationships.
Yousuf Hassan Syed indicated no relevant financial relationships.
Nandini Patel indicated no relevant financial relationships.
Hari Priya Nistala indicated no relevant financial relationships.
Rupak Desai indicated no relevant financial relationships.
Pranay T. Vaghela, MBBS1, Rohan Raj, MBBS2, Jithin Kolli, MBBS3, Jyoti Yadav, MBBS4, Yousuf Hassan Syed, MD5, Nandini Hemant. Patel, MBBS6, Hari Priya Nistala, MBBS7, Rupak Desai, MBBS8. P3233 - Prevalence and Impact of Prediabetes on Cardiovascular and Cerebrovascular Outcomes in Inflammatory Bowel Disease: A Population-Based Nationwide Analysis (2022), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1The Maharaja Sayajirao University of Baroda, Navsari, Gujarat, India; 2Memorial Hospital at Gulfport, Gulfport, MS; 3JSS MEDICAL COLLEGE, Andra Pradesh, Andhra Pradesh, India; 4JSS Medical college, Mysore, Karnataka, India; 5Team Health, Las Vegas, NV; 6Pramukhswami Medical College, Gujarat, India, Anand, Gujarat, India; 7Maharajah's Institute of Medical Sciences, Leander, TX; 8Independent Outcomes Researcher, Atlanta, GA
Introduction: While inflammatory bowel disease (IBD) is known to increase cardiovascular risk and its association with diabetes has been evaluated before, large-scale data on the burden and impact of prediabetes (pDM) in this population remain unclear. This study aimed to evaluate the burden of pDM in IBD-related hospitalizations and its association with cardiovascular and cerebrovascular events using a population-based analysis.
Methods: Using ICD-10 codes, we conducted a retrospective analysis of the 2022 National Inpatient Sample (NIS) including adult IBD hospitalizations without established diabetes. Patients were stratified by pDM status. Baseline demographics and comorbidities were compared, and multivariable logistic regression assessed odds ratios (OR) for acute myocardial infarction (AMI), ischemic stroke (AIS), atrial fibrillation (AF), venous thromboembolism (VTE), cardiac arrest, and in-hospital mortality. Subgroup analysis was performed for younger [18-44] IBD patients. A p value < 0.05 was considered statistically significant.
Results: Of 259,505 adult IBD hospitalizations, 3,220 (1.2%) had a concurrent diagnosis of pDM. Patients with pDM were older (median age 63 vs. 54), more likely to be male (46.1% vs. 42.8%), and had higher prevalence among Black (14.4% vs. 11.2%) and Hispanic (11.3% vs. 7.1%) groups. Patients with pDM had higher comorbidity burdens, including chronic pulmonary disease (25.3% vs. 19.6%), complicated hypertension (18.1% vs. 13.9%), and smoking history (43.1% vs. 37.1%). In the full cohort, pDM was independently associated with increased odds of AMI (OR 1.91; 95% CI: 1.29-2.82; p< 0.001) and AIS (OR 2.14; 95% CI: 1.25-3.67; p=0.006). Other outcomes including AF, VTE, cardiac arrest, and in-hospital mortality were not significantly different. Among younger patients, no outcome reached significance, though AIS showed a trend (OR 6.88; p=0.052).
Discussion: Prediabetes is uncommon among IBD hospitalizations but is associated with significantly increased cardiovascular and cerebrovascular risk. These findings highlight the importance of early metabolic risk screening and intervention in this population.
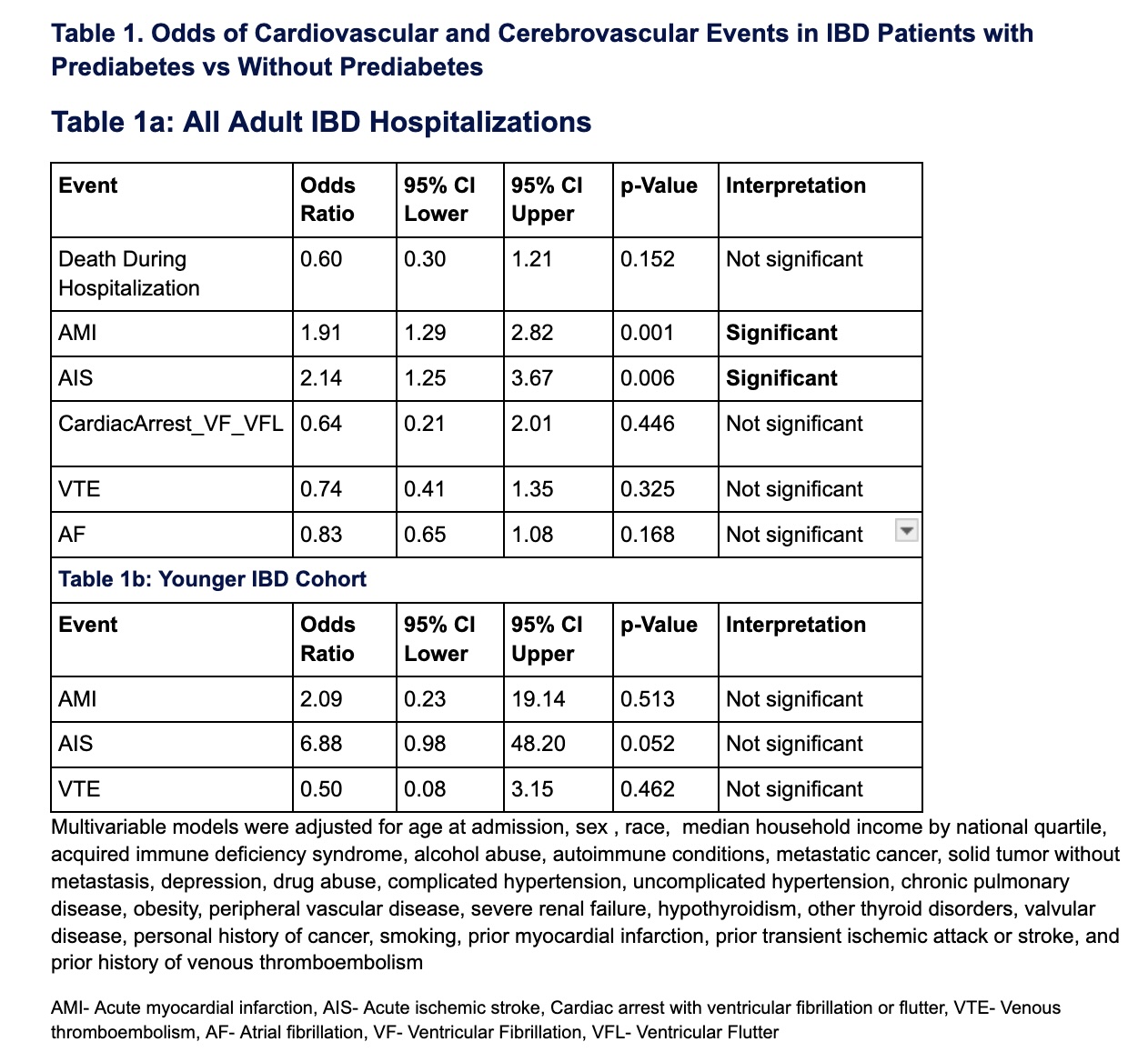
Figure: Table 1. Odds of cardiovascular and cerebroovascular events in IBD patients with prediabetes v/s without prediabetes.
Disclosures:
Pranay Vaghela indicated no relevant financial relationships.
Rohan Raj indicated no relevant financial relationships.
Jithin Kolli indicated no relevant financial relationships.
Jyoti Yadav indicated no relevant financial relationships.
Yousuf Hassan Syed indicated no relevant financial relationships.
Nandini Patel indicated no relevant financial relationships.
Hari Priya Nistala indicated no relevant financial relationships.
Rupak Desai indicated no relevant financial relationships.
Pranay T. Vaghela, MBBS1, Rohan Raj, MBBS2, Jithin Kolli, MBBS3, Jyoti Yadav, MBBS4, Yousuf Hassan Syed, MD5, Nandini Hemant. Patel, MBBS6, Hari Priya Nistala, MBBS7, Rupak Desai, MBBS8. P3233 - Prevalence and Impact of Prediabetes on Cardiovascular and Cerebrovascular Outcomes in Inflammatory Bowel Disease: A Population-Based Nationwide Analysis (2022), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
