Monday Poster Session
Category: IBD
P3198 - Implementation of a Modified Malnutrition Screening Tool in a Real-World Tertiary Care Center
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Taylor Riggs, MD
Baylor College of Medicine
Houston, TX
Presenting Author(s)
Taylor Riggs, MD, Megan Kelso, NP, Jared Sninsky, MD, MSCR, Stalin Subramanian, MD, Richa Shukla, MD, Jason Hou, MD, MS, FACG
Baylor College of Medicine, Houston, TX
Introduction: Malnutrition in inflammatory bowel disease (IBD) is common and is associated with negative clinical outcomes. Routine malnutrition screening is recommended in all IBD patients, however, screening rates in clinical practice remain low. An IBD nutrition care pathway was previously published, and pilot testing using the modified malnutrition universal screening tool (mMUST) demonstrated that 92% of patients completed malnutrition screening. We aimed to implement this screening tool at a tertiary IBD clinic to better identify patients at risk of malnutrition who may benefit from referral to a dietitian.
Methods: Implementation was performed in our tertiary care IBD clinic in Houston, Texas, between April and July 2024. The implementation process involved training rooming staff (medical assistants) and incorporating an mMUST prompt into the electronic medical record using an Epic “dot phrase” during clinic intake. If a patient answered “yes” to any of the questions, the provider was prompted to place a dietary referral. A chart review was conducted to assess the characteristics of patients who screened positive, including disease activity. Rates of micronutrient lab orders and prescriptions were also assessed.
Results: The mMUST was completed in 126 out of 497 patients (25%). Of those who completed the screening, 34 patients (27%) answered yes to at least one question, indicating risk of malnutrition. Only 4 out of the 34 at-risk patients (12%) were referred to a dietitian. Most of the patients who screened positive were not in clinical remission (85%). There were numerically higher rates of micronutrient labs ordered and micronutrient deficiencies found in the positive mMUST group compared to the negative, but this did not reach statistical significance.
Discussion: Rates of malnutrition screening and dietary referrals remained low despite attempts at the implementation of universal screening in our clinic. Most of the patients who screened positive had active disease, requiring optimization of medical management. Numerically higher rates of micronutrient deficiencies in these patients highlight the need for co-management with a dietitian. Barriers to dietary referral, such as the lack of a local IBD-educated dietitian, may have played a role in the low referral rates. Future directions include identifying ways to improve access to IBD-educated dietitians to improve rates of multidisciplinary management.
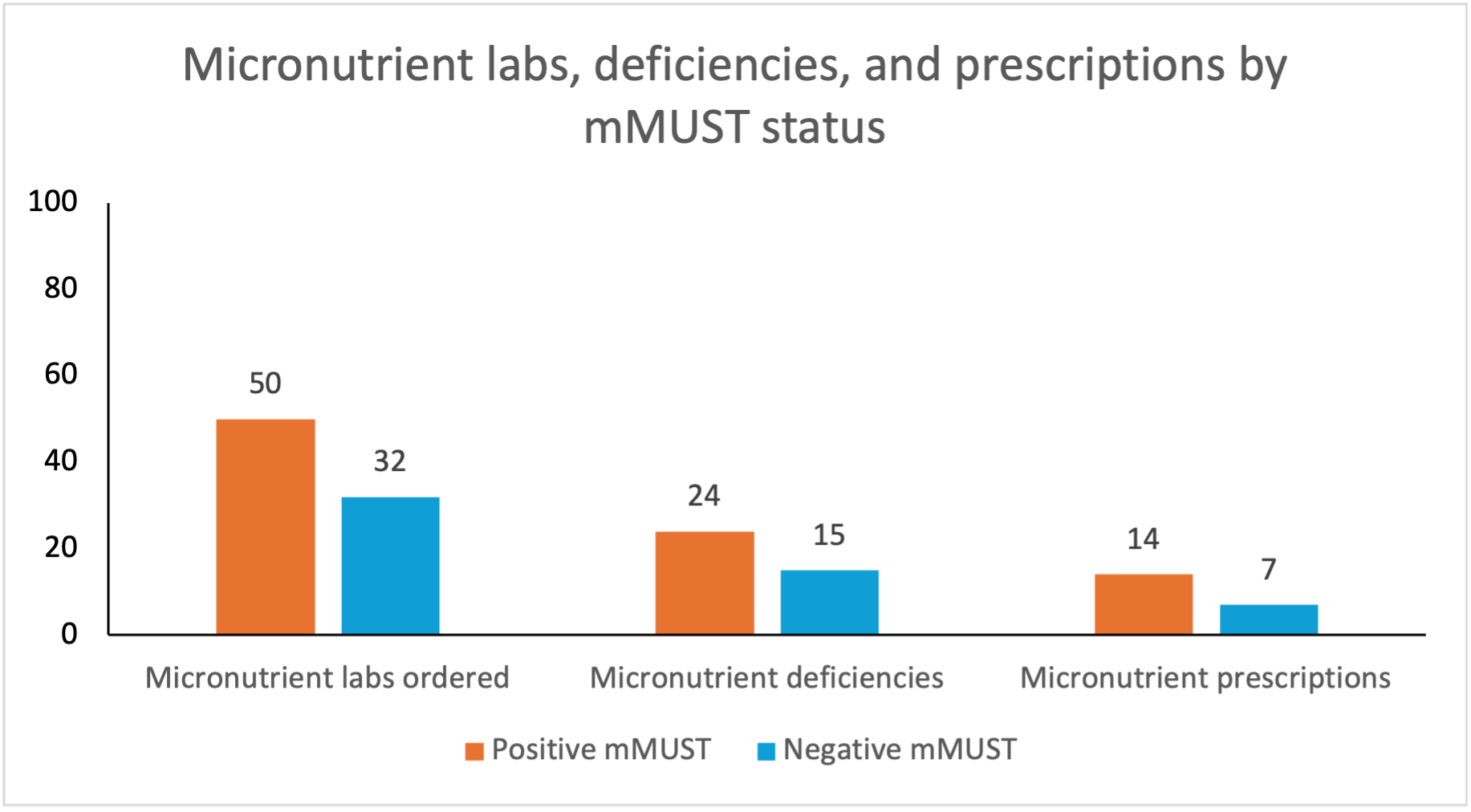
Figure: Micronutrient labs, deficiencies, and prescriptions by mMUST status
Disclosures:
Taylor Riggs indicated no relevant financial relationships.
Megan Kelso indicated no relevant financial relationships.
Jared Sninsky indicated no relevant financial relationships.
Stalin Subramanian indicated no relevant financial relationships.
Richa Shukla: Abbvie, Lilly – Speakers Bureau.
Jason Hou: Abbvie – Grant/Research Support. Eli-Lilly – Grant/Research Support. Janssen – Grant/Research Support. Pfizer – Grant/Research Support. Vedanta – Grant/Research Support.
Taylor Riggs, MD, Megan Kelso, NP, Jared Sninsky, MD, MSCR, Stalin Subramanian, MD, Richa Shukla, MD, Jason Hou, MD, MS, FACG. P3198 - Implementation of a Modified Malnutrition Screening Tool in a Real-World Tertiary Care Center, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Baylor College of Medicine, Houston, TX
Introduction: Malnutrition in inflammatory bowel disease (IBD) is common and is associated with negative clinical outcomes. Routine malnutrition screening is recommended in all IBD patients, however, screening rates in clinical practice remain low. An IBD nutrition care pathway was previously published, and pilot testing using the modified malnutrition universal screening tool (mMUST) demonstrated that 92% of patients completed malnutrition screening. We aimed to implement this screening tool at a tertiary IBD clinic to better identify patients at risk of malnutrition who may benefit from referral to a dietitian.
Methods: Implementation was performed in our tertiary care IBD clinic in Houston, Texas, between April and July 2024. The implementation process involved training rooming staff (medical assistants) and incorporating an mMUST prompt into the electronic medical record using an Epic “dot phrase” during clinic intake. If a patient answered “yes” to any of the questions, the provider was prompted to place a dietary referral. A chart review was conducted to assess the characteristics of patients who screened positive, including disease activity. Rates of micronutrient lab orders and prescriptions were also assessed.
Results: The mMUST was completed in 126 out of 497 patients (25%). Of those who completed the screening, 34 patients (27%) answered yes to at least one question, indicating risk of malnutrition. Only 4 out of the 34 at-risk patients (12%) were referred to a dietitian. Most of the patients who screened positive were not in clinical remission (85%). There were numerically higher rates of micronutrient labs ordered and micronutrient deficiencies found in the positive mMUST group compared to the negative, but this did not reach statistical significance.
Discussion: Rates of malnutrition screening and dietary referrals remained low despite attempts at the implementation of universal screening in our clinic. Most of the patients who screened positive had active disease, requiring optimization of medical management. Numerically higher rates of micronutrient deficiencies in these patients highlight the need for co-management with a dietitian. Barriers to dietary referral, such as the lack of a local IBD-educated dietitian, may have played a role in the low referral rates. Future directions include identifying ways to improve access to IBD-educated dietitians to improve rates of multidisciplinary management.
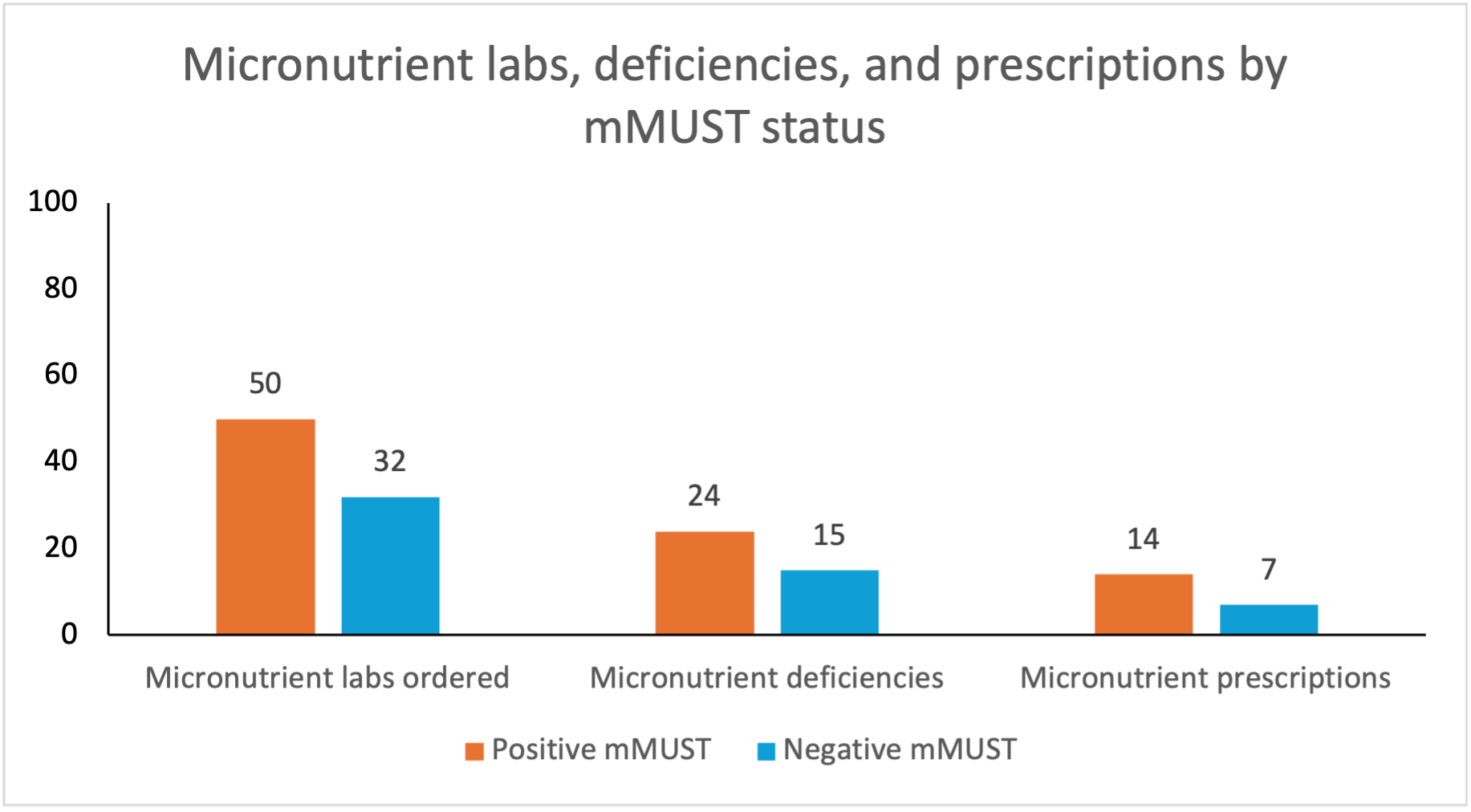
Figure: Micronutrient labs, deficiencies, and prescriptions by mMUST status
Disclosures:
Taylor Riggs indicated no relevant financial relationships.
Megan Kelso indicated no relevant financial relationships.
Jared Sninsky indicated no relevant financial relationships.
Stalin Subramanian indicated no relevant financial relationships.
Richa Shukla: Abbvie, Lilly – Speakers Bureau.
Jason Hou: Abbvie – Grant/Research Support. Eli-Lilly – Grant/Research Support. Janssen – Grant/Research Support. Pfizer – Grant/Research Support. Vedanta – Grant/Research Support.
Taylor Riggs, MD, Megan Kelso, NP, Jared Sninsky, MD, MSCR, Stalin Subramanian, MD, Richa Shukla, MD, Jason Hou, MD, MS, FACG. P3198 - Implementation of a Modified Malnutrition Screening Tool in a Real-World Tertiary Care Center, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

