Monday Poster Session
Category: IBD
P3187 - Disability-Related Vulnerability at the Community Level Is Not Associated With Inflammatory Bowel Disease Outcomes
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Hannah Zuercher, MD, BS
University of Florida
Gainesville, FL
Presenting Author(s)
Hannah Zuercher, MD, BS, Tomas Potlach, BS, Mousumi Sinha, BS, Naveen Baskaran, MD, MSHI, Tianze Jiao, PhD, Ellen M. Zimmermann, MD, Naueen Chaudhry, MD
University of Florida, Gainesville, FL
Introduction: Social determinants of health are critical factors associated with adverse outcomes of IBD. The social vulnerability index (SVI) is a census-tract-derived metric from that measures the vulnerability of a community based on self-reported demographic and socioeconomic factors. This study aims to discern if self-reported community-level disability burden is associated with poor IBD outcomes.
Methods: A retrospective study was conducted from 2015-2024 using Epic Cosmos, an electronic health record database representing 277 million lives. Patients with >1 ICD-10 CM diagnosis codes for Crohn’s disease (CD) or ulcerative colitis (UC) were included. Chi-square tests and multivariate logistic regression compared the odds of exposure to IBD-specific medications and SVI outcomes.
Results: A total of 49,784 patients met study criteria. Disability SVI outcomes were classified by age (Table 1). Q2 females were more likely to receive anti-IL-12/23 biologics (OR 1.16, 95% CI [1.01, 1.33], p=0.039); Q3 females were less likely to have hospital admissions/endoscopies (OR 0.88, 95% CI [0.79, 1.00], p=0.042; OR 0.59, 95% CI [0.38, 0.91], p=0.018). Q2 Black patients were less likely to have hospital admissions and emergency department (ED) visits, and more likely to receive anti-IL-12/23 biologics than White patients. Q4 Black patients were less likely to receive anti-integrin biologics. Q4 Medicaid patients were less likely to have ED visits, and receive JAK-inhibitors and corticosteroids than Medicare patients. Q3 and Q4 Medicaid patients were less likely to receive S1P-modulators. Q2, Q3, and Q4 Medicaid patients were less likely to receive anti-TNF inhibitors. There were no SVI differences in surgical procedure exposure. Many Southeastern states have a higher mean disability SVI (Figure 1).
Discussion: SVI quartiles were associated with distinct patterns of IBD therapy and health‐care utilization but did not predict all adverse outcomes. Compared to the lowest‐vulnerability quartile, Q2–Q4 patients were more likely to receive advanced therapies in specific age groups; medication use differed by sex, race, and insurance status. Geographic mapping unveiled higher disability SVI in Southeastern states, suggesting regional social vulnerability. While disability SVI can help identify communities at risk for altered prescribing patterns, it does not uniformly predict ED admissions or procedural interventions—and thus should be used alongside other measures to gauge IBD quality of care.
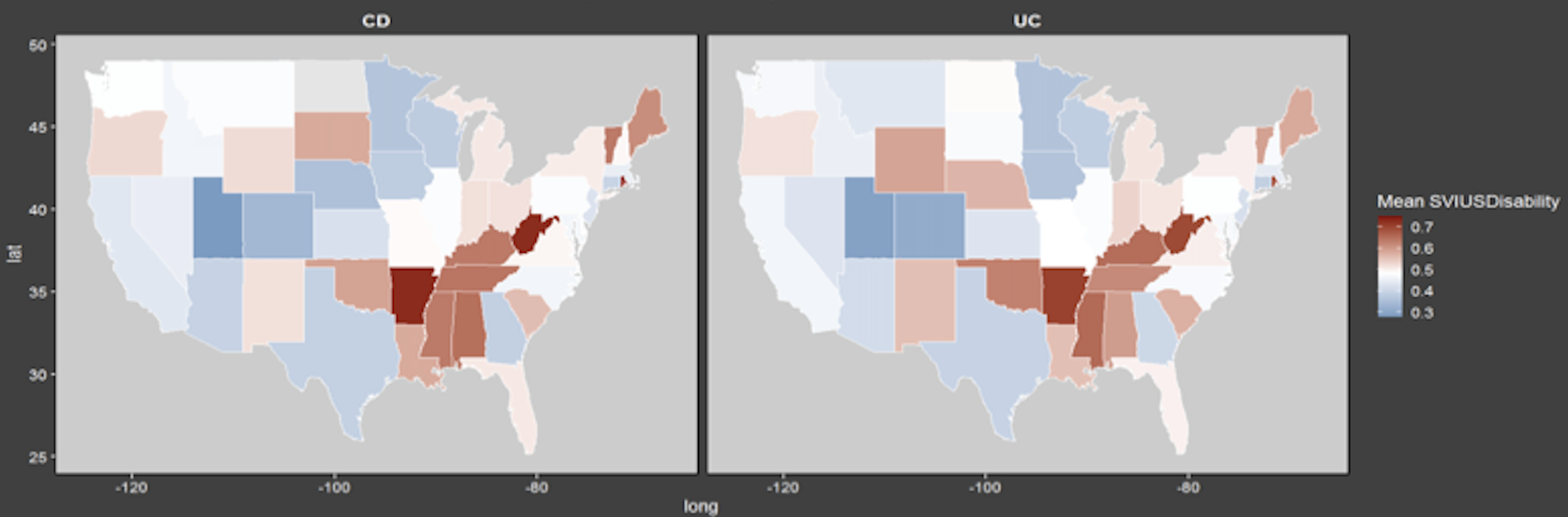
Figure: Table 1. Disability social-vulnerability index (SVI) quartile outcomes, with Q4 being the most vulnerable population, classified by age grouping (reference 18-25 years old) and medication usage.
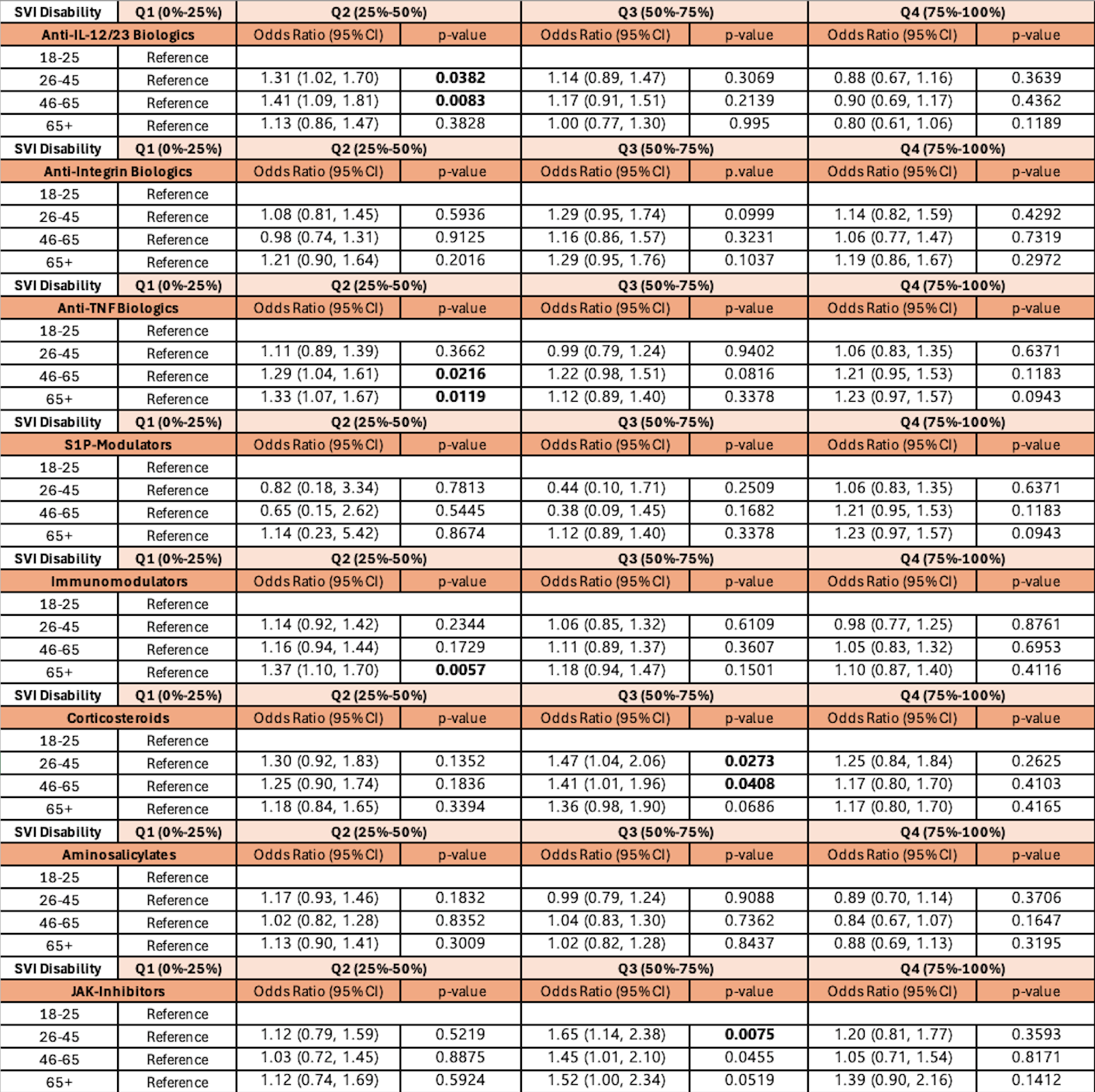
Figure: Figure 1. Disability SVI status classified at the state level.
Disclosures:
Hannah Zuercher indicated no relevant financial relationships.
Tomas Potlach indicated no relevant financial relationships.
Mousumi Sinha indicated no relevant financial relationships.
Naveen Baskaran indicated no relevant financial relationships.
Tianze Jiao indicated no relevant financial relationships.
Ellen Zimmermann indicated no relevant financial relationships.
Naueen Chaudhry indicated no relevant financial relationships.
Hannah Zuercher, MD, BS, Tomas Potlach, BS, Mousumi Sinha, BS, Naveen Baskaran, MD, MSHI, Tianze Jiao, PhD, Ellen M. Zimmermann, MD, Naueen Chaudhry, MD. P3187 - Disability-Related Vulnerability at the Community Level Is Not Associated With Inflammatory Bowel Disease Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Florida, Gainesville, FL
Introduction: Social determinants of health are critical factors associated with adverse outcomes of IBD. The social vulnerability index (SVI) is a census-tract-derived metric from that measures the vulnerability of a community based on self-reported demographic and socioeconomic factors. This study aims to discern if self-reported community-level disability burden is associated with poor IBD outcomes.
Methods: A retrospective study was conducted from 2015-2024 using Epic Cosmos, an electronic health record database representing 277 million lives. Patients with >1 ICD-10 CM diagnosis codes for Crohn’s disease (CD) or ulcerative colitis (UC) were included. Chi-square tests and multivariate logistic regression compared the odds of exposure to IBD-specific medications and SVI outcomes.
Results: A total of 49,784 patients met study criteria. Disability SVI outcomes were classified by age (Table 1). Q2 females were more likely to receive anti-IL-12/23 biologics (OR 1.16, 95% CI [1.01, 1.33], p=0.039); Q3 females were less likely to have hospital admissions/endoscopies (OR 0.88, 95% CI [0.79, 1.00], p=0.042; OR 0.59, 95% CI [0.38, 0.91], p=0.018). Q2 Black patients were less likely to have hospital admissions and emergency department (ED) visits, and more likely to receive anti-IL-12/23 biologics than White patients. Q4 Black patients were less likely to receive anti-integrin biologics. Q4 Medicaid patients were less likely to have ED visits, and receive JAK-inhibitors and corticosteroids than Medicare patients. Q3 and Q4 Medicaid patients were less likely to receive S1P-modulators. Q2, Q3, and Q4 Medicaid patients were less likely to receive anti-TNF inhibitors. There were no SVI differences in surgical procedure exposure. Many Southeastern states have a higher mean disability SVI (Figure 1).
Discussion: SVI quartiles were associated with distinct patterns of IBD therapy and health‐care utilization but did not predict all adverse outcomes. Compared to the lowest‐vulnerability quartile, Q2–Q4 patients were more likely to receive advanced therapies in specific age groups; medication use differed by sex, race, and insurance status. Geographic mapping unveiled higher disability SVI in Southeastern states, suggesting regional social vulnerability. While disability SVI can help identify communities at risk for altered prescribing patterns, it does not uniformly predict ED admissions or procedural interventions—and thus should be used alongside other measures to gauge IBD quality of care.
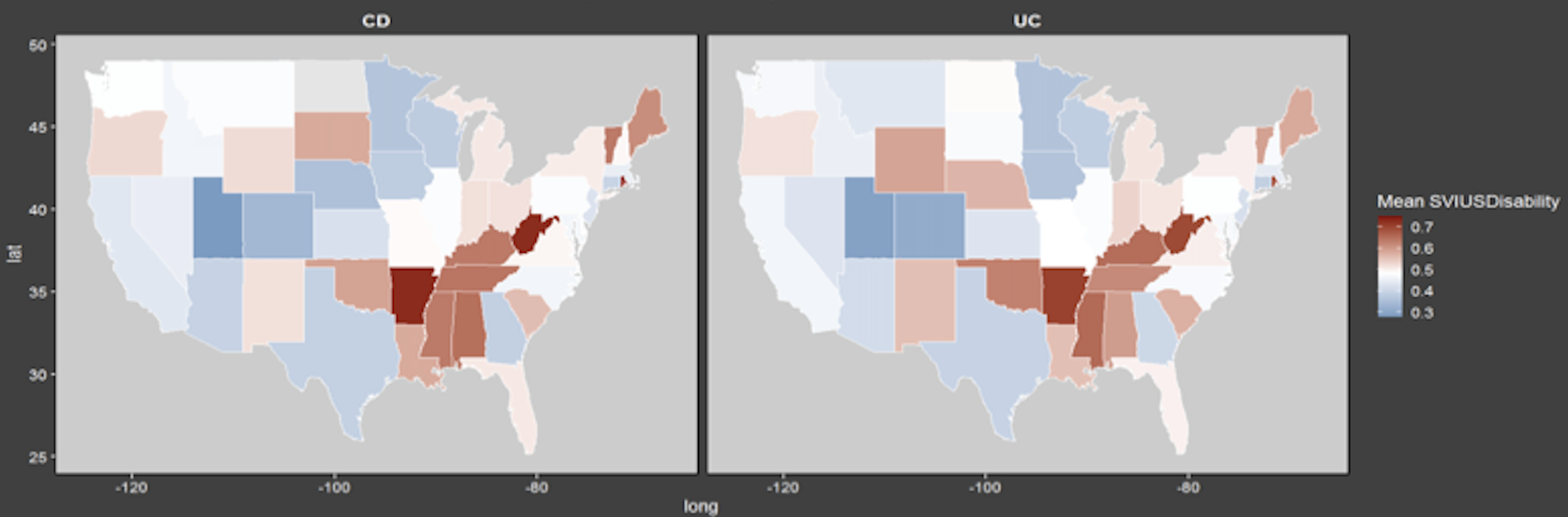
Figure: Table 1. Disability social-vulnerability index (SVI) quartile outcomes, with Q4 being the most vulnerable population, classified by age grouping (reference 18-25 years old) and medication usage.
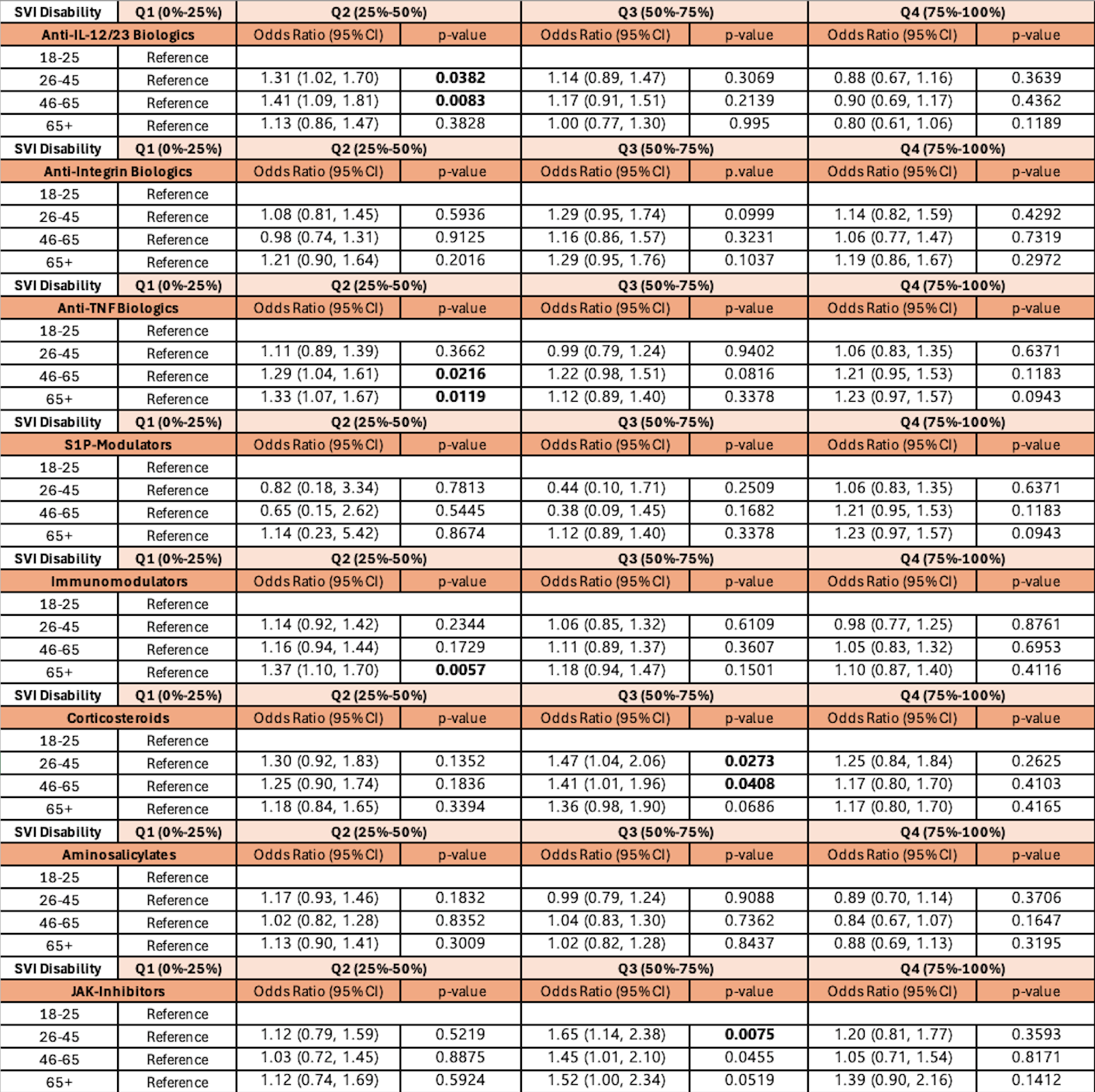
Figure: Figure 1. Disability SVI status classified at the state level.
Disclosures:
Hannah Zuercher indicated no relevant financial relationships.
Tomas Potlach indicated no relevant financial relationships.
Mousumi Sinha indicated no relevant financial relationships.
Naveen Baskaran indicated no relevant financial relationships.
Tianze Jiao indicated no relevant financial relationships.
Ellen Zimmermann indicated no relevant financial relationships.
Naueen Chaudhry indicated no relevant financial relationships.
Hannah Zuercher, MD, BS, Tomas Potlach, BS, Mousumi Sinha, BS, Naveen Baskaran, MD, MSHI, Tianze Jiao, PhD, Ellen M. Zimmermann, MD, Naueen Chaudhry, MD. P3187 - Disability-Related Vulnerability at the Community Level Is Not Associated With Inflammatory Bowel Disease Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
