Monday Poster Session
Category: IBD
P3174 - Trends in Inflammatory Bowel Disease-Associated Colorectal Cancer Mortality in the US (1999– 2023): A CDC WONDER Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- VC
Vineet R. Chandak, MBBS (he/him/his)
Seth Gordhandas Sundardas Medical College and KEM Hospital
Mumbai, Maharashtra, India
Presenting Author(s)
Vineet R. Chandak, MBBS1, Medhansh Biradar, MBBS2, Neha Waseem, MBBS3, Maurya Patel, 1, Waleed Tariq, MBBS4, Sushrut Ingawale, MD, DNB, MBBS5
1Seth Gordhandas Sundardas Medical College and KEM Hospital, Mumbai, Maharashtra, India; 2All India Institute of Medical Sciences, Raipur, Chhattisgarh, India; 3F M H College of Medicine and Dentistry, Lahore, Punjab, Pakistan; 4Fatima Memorial Hospital, Lahore, Punjab, Pakistan; 5Quinnipiac University - Frank H Netter MD School of Medicine, Bridgeport, CT
Introduction: Inflammatory bowel disease (IBD)-associated colorectal cancer represents a significant and rising cause of morbidity and mortality in the United States. However, the national-level trends across demographic groups remain poorly characterised. We aim to study trends and disparities in IBD-associated colorectal cancer mortality among U.S. adults ≥25 years old, from 1999–2023.
Methods: Data from CDC WONDER (1999–2023) identified U.S. decedents with IBD (ICD-10: K50–K51) and colorectal cancer (ICD-10: C18–C20). Age-adjusted mortality rates (AAMR) per 100,000 were stratified by sex, ethnicity, age, region, state, and urbanisation. Trends were analysed using Joinpoint regression to estimate annual percentage change (APC) and average annual percentage change (AAPC) with 95% confidence intervals and significance at p < 0.05.
Results: From 1999–2023, IBD-associated colorectal cancer caused 3,323 deaths in the U.S. AAMRs declined from 0.061 in 1999 to 0.045 in 2016 (APC: –1.492; 95% CI: –3.673 to 0.738), then rose to 0.064 in 2023 (APC: 8.741; 95% CI: 1.449 to 16.557). Overall AAPC was 1.389 (95% CI: –1.032 to 3.869). In men AAMR dropped from 0.059 in 1999 to 0.040 in 2017 (APC: –0.973; 95% CI: –2.122 to 0.190), then increased to 0.099 in 2023 (APC: 8.535; 95% CI: 3.323 to 14.010); while it progressively increased in women with AAPC of 2.585; 95% CI: 0.589 to 4.620. The Non-Hispanic White population showed a declining AAMR from 0.068 in 1999 to 0.042 in 2017 (APC: –0.802; 95% CI: –2.728 to 1.161), followed by a significant increase to 0.088 in 2023 (APC: 11.733; 95% CI: 1.987 to 22.410). Adults aged ≥65 years had the highest mortality rates, with a notable increase from 0.137 in 2018 to 0.260 in 2023 (APC: 13.542; 95% CI: 5.471 to 22.231). From 1999-2023, AAMR declined in those aged 45–64 years (AAPC: –1.562) and mortality was lowest in those aged 25-44 years. Regionally, AAMR rose in the Midwest (AAPC: 1.724) and West (AAPC: 0.931) and in the South, rates fell from 0.052 in 1999 to 0.009 in 2014 (APC: –2.802), then increased significantly to 0.068 in 2023 (APC: 17.735). Majority of deaths occurred at the decedent's home (37.9%).
Discussion: IBD-associated colorectal cancer mortality in U.S. adults (25+ years) declined till 2016, followed by an increasing trend through 2023. The Mortality rates were higher in males, older adults (65+ years), Whites, the South region and in California. The observed disparities hence warrants targeted public health intervention especially for the vulnerable groups.
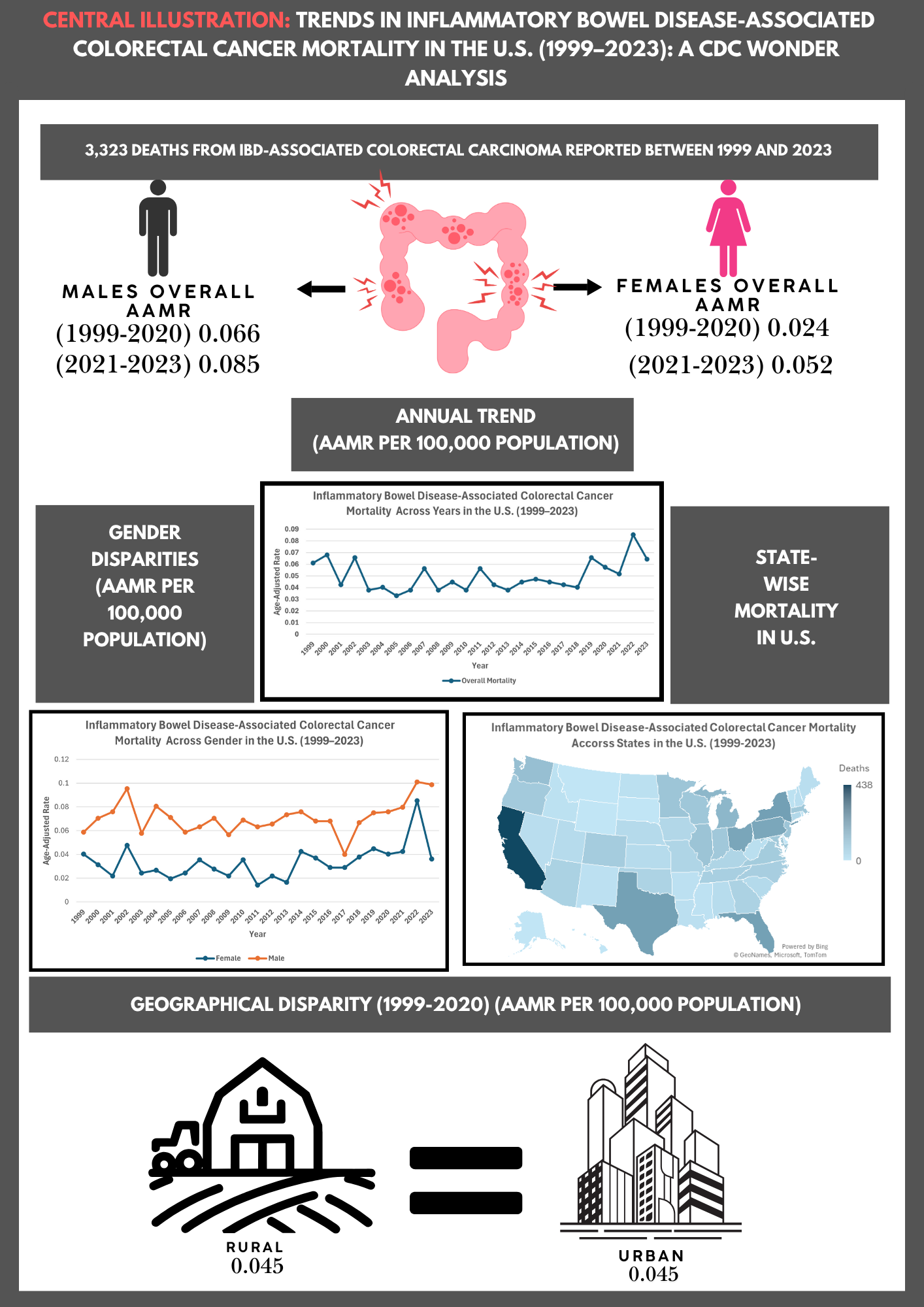
Figure: Disparities in IBD Associated Colorectal Cancer Mortality in the US:
25 year overview (1999 to 2023 )
Disclosures:
Vineet Chandak indicated no relevant financial relationships.
Medhansh Biradar indicated no relevant financial relationships.
Neha Waseem indicated no relevant financial relationships.
Maurya Patel indicated no relevant financial relationships.
Waleed Tariq indicated no relevant financial relationships.
Sushrut Ingawale indicated no relevant financial relationships.
Vineet R. Chandak, MBBS1, Medhansh Biradar, MBBS2, Neha Waseem, MBBS3, Maurya Patel, 1, Waleed Tariq, MBBS4, Sushrut Ingawale, MD, DNB, MBBS5. P3174 - Trends in Inflammatory Bowel Disease-Associated Colorectal Cancer Mortality in the US (1999– 2023): A CDC WONDER Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Seth Gordhandas Sundardas Medical College and KEM Hospital, Mumbai, Maharashtra, India; 2All India Institute of Medical Sciences, Raipur, Chhattisgarh, India; 3F M H College of Medicine and Dentistry, Lahore, Punjab, Pakistan; 4Fatima Memorial Hospital, Lahore, Punjab, Pakistan; 5Quinnipiac University - Frank H Netter MD School of Medicine, Bridgeport, CT
Introduction: Inflammatory bowel disease (IBD)-associated colorectal cancer represents a significant and rising cause of morbidity and mortality in the United States. However, the national-level trends across demographic groups remain poorly characterised. We aim to study trends and disparities in IBD-associated colorectal cancer mortality among U.S. adults ≥25 years old, from 1999–2023.
Methods: Data from CDC WONDER (1999–2023) identified U.S. decedents with IBD (ICD-10: K50–K51) and colorectal cancer (ICD-10: C18–C20). Age-adjusted mortality rates (AAMR) per 100,000 were stratified by sex, ethnicity, age, region, state, and urbanisation. Trends were analysed using Joinpoint regression to estimate annual percentage change (APC) and average annual percentage change (AAPC) with 95% confidence intervals and significance at p < 0.05.
Results: From 1999–2023, IBD-associated colorectal cancer caused 3,323 deaths in the U.S. AAMRs declined from 0.061 in 1999 to 0.045 in 2016 (APC: –1.492; 95% CI: –3.673 to 0.738), then rose to 0.064 in 2023 (APC: 8.741; 95% CI: 1.449 to 16.557). Overall AAPC was 1.389 (95% CI: –1.032 to 3.869). In men AAMR dropped from 0.059 in 1999 to 0.040 in 2017 (APC: –0.973; 95% CI: –2.122 to 0.190), then increased to 0.099 in 2023 (APC: 8.535; 95% CI: 3.323 to 14.010); while it progressively increased in women with AAPC of 2.585; 95% CI: 0.589 to 4.620. The Non-Hispanic White population showed a declining AAMR from 0.068 in 1999 to 0.042 in 2017 (APC: –0.802; 95% CI: –2.728 to 1.161), followed by a significant increase to 0.088 in 2023 (APC: 11.733; 95% CI: 1.987 to 22.410). Adults aged ≥65 years had the highest mortality rates, with a notable increase from 0.137 in 2018 to 0.260 in 2023 (APC: 13.542; 95% CI: 5.471 to 22.231). From 1999-2023, AAMR declined in those aged 45–64 years (AAPC: –1.562) and mortality was lowest in those aged 25-44 years. Regionally, AAMR rose in the Midwest (AAPC: 1.724) and West (AAPC: 0.931) and in the South, rates fell from 0.052 in 1999 to 0.009 in 2014 (APC: –2.802), then increased significantly to 0.068 in 2023 (APC: 17.735). Majority of deaths occurred at the decedent's home (37.9%).
Discussion: IBD-associated colorectal cancer mortality in U.S. adults (25+ years) declined till 2016, followed by an increasing trend through 2023. The Mortality rates were higher in males, older adults (65+ years), Whites, the South region and in California. The observed disparities hence warrants targeted public health intervention especially for the vulnerable groups.
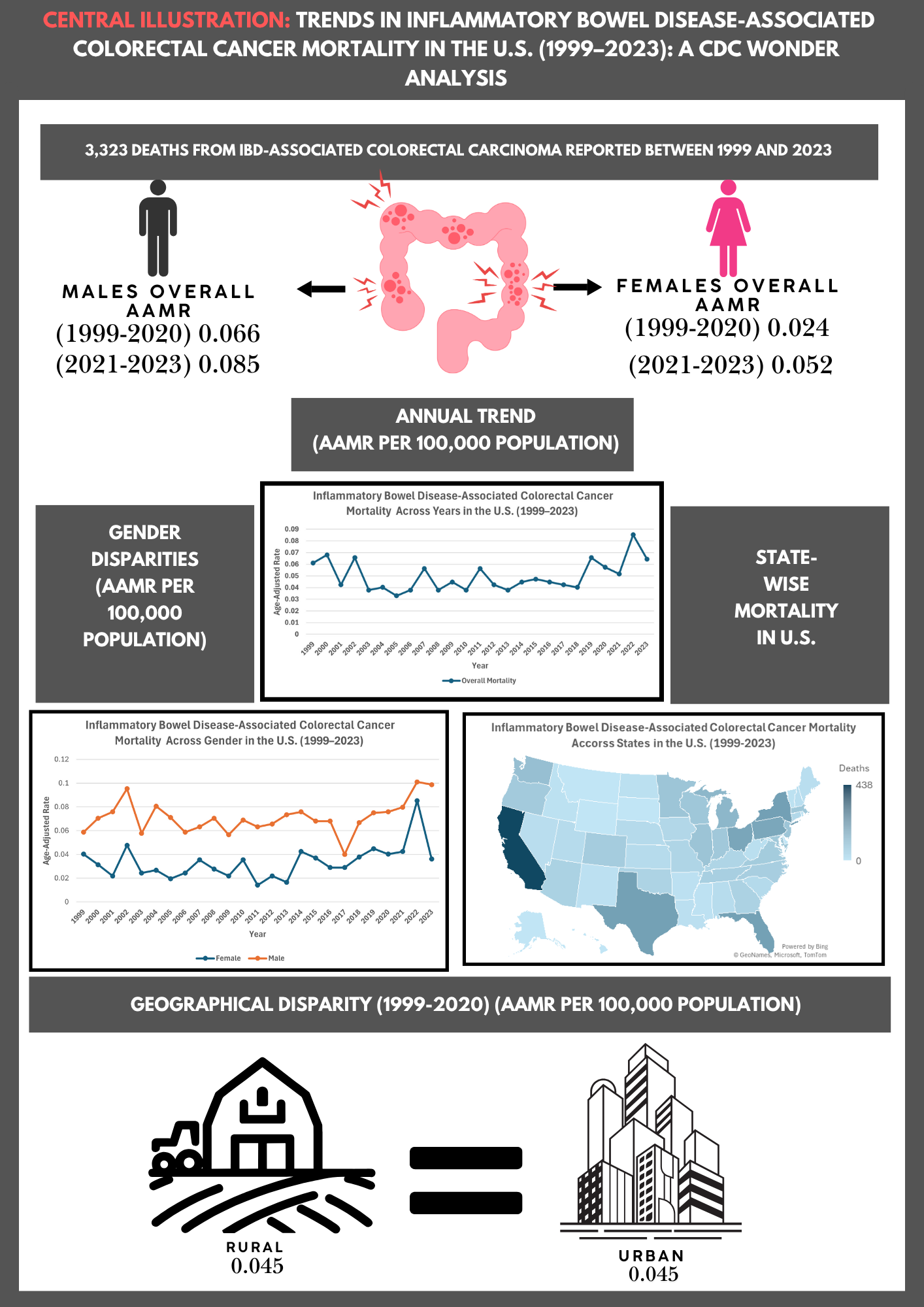
Figure: Disparities in IBD Associated Colorectal Cancer Mortality in the US:
25 year overview (1999 to 2023 )
Disclosures:
Vineet Chandak indicated no relevant financial relationships.
Medhansh Biradar indicated no relevant financial relationships.
Neha Waseem indicated no relevant financial relationships.
Maurya Patel indicated no relevant financial relationships.
Waleed Tariq indicated no relevant financial relationships.
Sushrut Ingawale indicated no relevant financial relationships.
Vineet R. Chandak, MBBS1, Medhansh Biradar, MBBS2, Neha Waseem, MBBS3, Maurya Patel, 1, Waleed Tariq, MBBS4, Sushrut Ingawale, MD, DNB, MBBS5. P3174 - Trends in Inflammatory Bowel Disease-Associated Colorectal Cancer Mortality in the US (1999– 2023): A CDC WONDER Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

