Monday Poster Session
Category: IBD
P3173 - Obesity as an Independent Risk Factor for Colorectal Dysplasia in Inflammatory Bowel Disease
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Naveena Luke, MD (she/her/hers)
NYU Grossman School of Medicine
Brooklyn, NY
Presenting Author(s)
Award: ACG Presidential Poster Award
Naveena Luke, MD1, Jahnavi Udaikumar, MD2, Carlos Echeverria, MD2, Olivia Delau, MS3, Xucong Meng, MPH4, Adam Faye, MD, MS3, Jordan Axelrad, MD, MPH5
1NYU Grossman School of Medicine, Brooklyn, NY; 2NYU Grossman School of Medicine, Department of Medicine, New York, NY; 3NYU Langone Health, New York, NY; 4NYU Grossman School of Medicine, New York, NY; 5Division of Gastroenterology, Department of Medicine, NYU Grossman School of Medicine, New York, NY
Introduction: Obesity has been linked to an increased risk of colorectal cancer in the general population, but its relationship with dysplasia among patients with inflammatory bowel disease (IBD) remains uncertain. Given obesity’s pro-inflammatory effects, understanding its role in dysplasia development is increasingly relevant. This study aimed to determine whether obesity is independently associated with colorectal dysplasia among patients with IBD undergoing surveillance colonoscopy.
Methods: We performed a retrospective matched case-control study at a tertiary care center among patients who underwent surveillance colonoscopy from 2020 to 2025. Cases were matched 1:1 by age, sex, and IBD subtype. Obesity was defined as mean BMI ≥30 kg/m² within five years before colonoscopy. Demographics, clinical characteristics, and histologic findings were collected. Multivariable conditional logistic regression was used to identify independent risk factors for dysplasia.
Results: We identified 216 patients with IBD who underwent surveillance colonoscopy (108 with dysplasia, 108 matched non-dysplasia controls). On univariable analysis, obesity was more common among dysplasia cases (30.6%) compared to controls (23.2%), although this difference was not statistically significant (p=0.22). In a multivariable model adjusting for covariates such as disease duration, prior dysplasia, and histologic severity (inactive/mild/moderate/severe), obesity was independently associated with dysplasia (adjusted odds ratio [aOR] 2.44, 95% CI 1.04 - 5.71). Additional predictors included longer disease duration (aOR 1.05, 95% CI 1.02 - 1.08) and prior dysplasia (aOR 5.10, 95% CI 1.50 - 17.33). Mild histologic inflammation reduced the risk of dysplasia (aOR 0.33, 95% CI 0.14 - 0.78), and a greater number of prior colonoscopies was modestly protective (aOR 0.88, 95% CI 0.77 - 0.99). Other variables including family history of colorectal cancer, smoking, diabetes, pseudopolyps, and strictures were not significantly associated with dysplasia.
Discussion: Obesity was independently associated with more than a 2-fold increased odds of colorectal dysplasia in patients with IBD, even after adjusting for clinical and histologic risk factors. These findings support incorporating BMI into dysplasia risk models and suggest that obese patients may benefit from enhanced surveillance strategies.
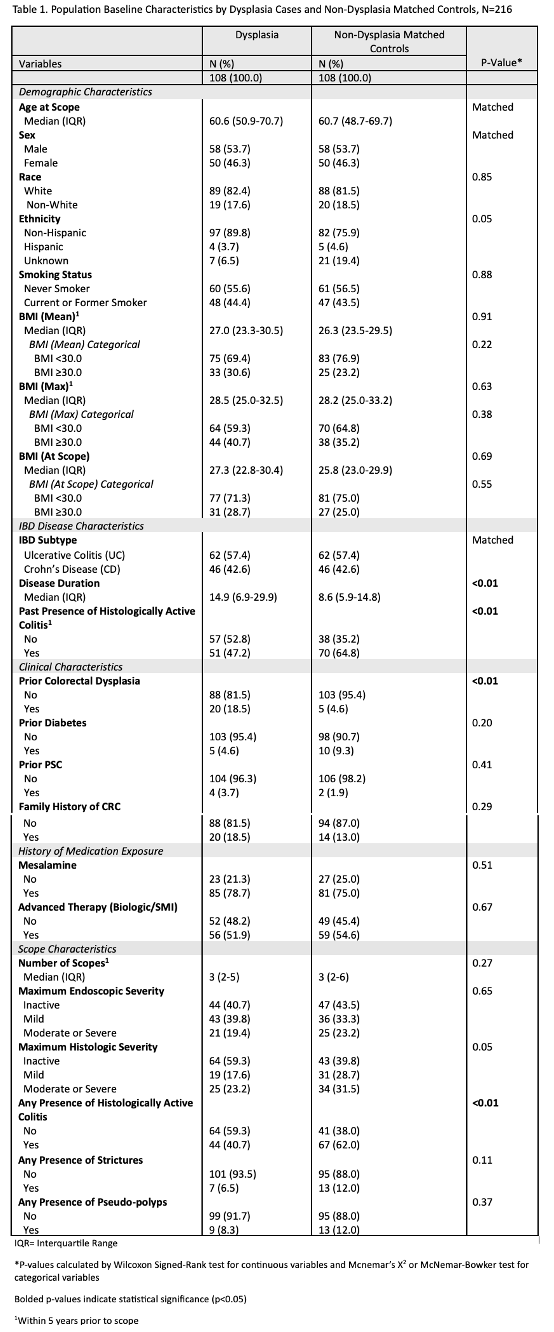
Figure: Table 1. Baseline demographic, clinical, and endoscopic characteristics of dysplasia cases and matched non-dysplasia controls (N=216). Groups were matched 1:1 by age, sex, race, and IBD subtype. Compared to controls, dysplasia cases had significantly longer disease duration, higher rates of prior colorectal dysplasia, and greater presence of histologically active colitis within the prior 5 years. No significant differences were observed in BMI, medication exposure, or maximum endoscopic severity. P-values <0.05 are bolded.
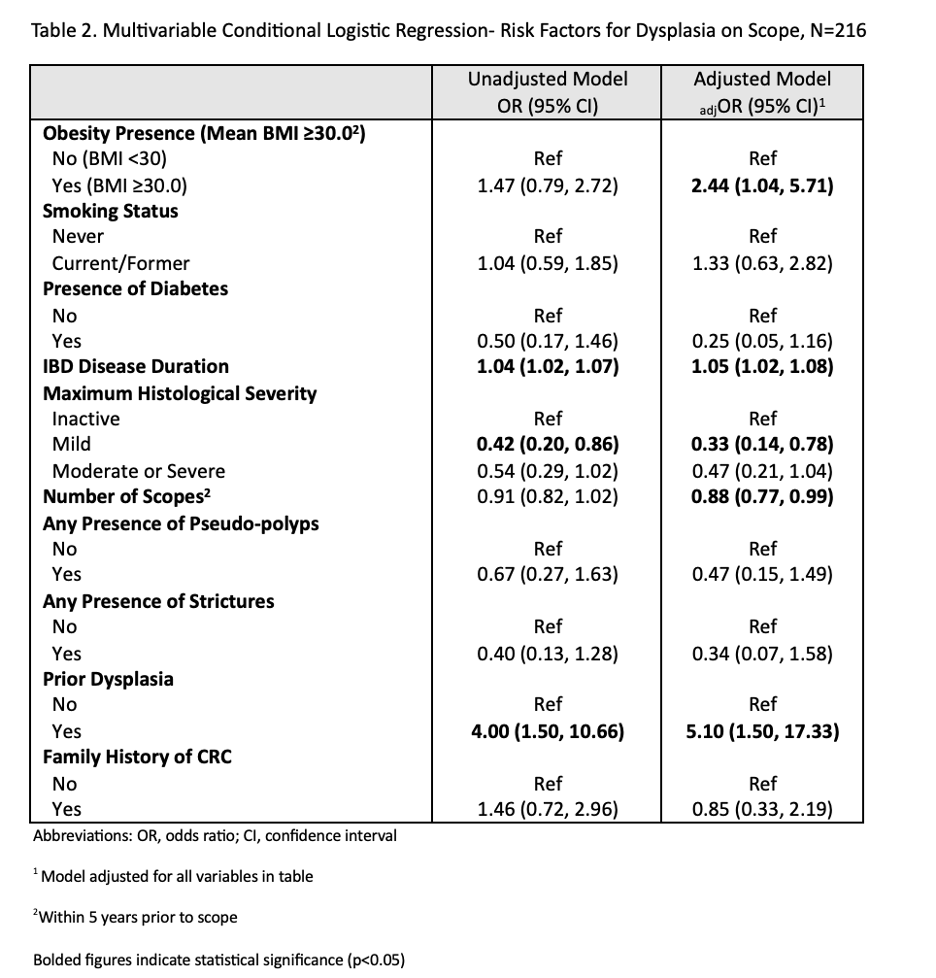
Figure: Table 2. Multivariable conditional logistic regression identifying risk factors associated with dysplasia on colonoscopy (N=216). In the adjusted model controlling for clinical and histologic variables, obesity (BMI ≥30.0), longer disease duration, and prior colorectal dysplasia were significantly associated with increased odds of dysplasia. Mild histologic inflammation was inversely associated with dysplasia compared to inactive disease. A greater number of colonoscopies within 5 years was also associated with reduced odds of dysplasia. Bolded values denote statistical significance (p < 0.05).
Disclosures:
Naveena Luke indicated no relevant financial relationships.
Jahnavi Udaikumar indicated no relevant financial relationships.
Carlos Echeverria indicated no relevant financial relationships.
Olivia Delau indicated no relevant financial relationships.
Xucong Meng indicated no relevant financial relationships.
Adam Faye: AbbVie – Honorarium. Eli Lilly – Consultant. NIH Grant K76AG083286 – Grant/Research Support. Takeda – Honorarium. The American College of Gastroenterology – Grant/Research Support. The Crohn's and Colitis Foundation – Grant/Research Support.
Jordan Axelrad: Abbvie – Advisory Committee/Board Member, Consultant, Honorarium. Abivax – Advisory Committee/Board Member, Consultant, Honorarium. Adiso – Advisory Committee/Board Member, Consultant, Honorarium. BioFire Diagnostics – Grant/Research Support. Biomerieux – Advisory Committee/Board Member, Consultant, Honorarium. Bristol-Myers Squibb – Advisory Committee/Board Member, Consultant, Honorarium. Celltrion – Advisory Committee/Board Member, Consultant, Honorarium. Ferring – Advisory Committee/Board Member, Consultant, Honorarium. Fresenius – Advisory Committee/Board Member, Consultant, Honorarium. Genentech – Grant/Research Support. Janssen – Advisory Committee/Board Member, Consultant. Janssen – Grant/Research Support. Janssen – Honorarium. Johnson & Johnson – Advisory Committee/Board Member, Consultant. Merck – Advisory Committee/Board Member, Consultant, Honorarium. NIH NIDDK Diseases K23DK124570 – Grant/Research Support. Pfizer – Advisory Committee/Board Member, Consultant, Honorarium. Sanofi – Advisory Committee/Board Member, Consultant, Honorarium. The Crohn's and Colitis Foundation (#878246) – Grant/Research Support. The Judith & Stewart Colton Center for Autoimmunity – Grant/Research Support. Vedanta – Advisory Committee/Board Member, Consultant, Honorarium.
Naveena Luke, MD1, Jahnavi Udaikumar, MD2, Carlos Echeverria, MD2, Olivia Delau, MS3, Xucong Meng, MPH4, Adam Faye, MD, MS3, Jordan Axelrad, MD, MPH5. P3173 - Obesity as an Independent Risk Factor for Colorectal Dysplasia in Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Naveena Luke, MD1, Jahnavi Udaikumar, MD2, Carlos Echeverria, MD2, Olivia Delau, MS3, Xucong Meng, MPH4, Adam Faye, MD, MS3, Jordan Axelrad, MD, MPH5
1NYU Grossman School of Medicine, Brooklyn, NY; 2NYU Grossman School of Medicine, Department of Medicine, New York, NY; 3NYU Langone Health, New York, NY; 4NYU Grossman School of Medicine, New York, NY; 5Division of Gastroenterology, Department of Medicine, NYU Grossman School of Medicine, New York, NY
Introduction: Obesity has been linked to an increased risk of colorectal cancer in the general population, but its relationship with dysplasia among patients with inflammatory bowel disease (IBD) remains uncertain. Given obesity’s pro-inflammatory effects, understanding its role in dysplasia development is increasingly relevant. This study aimed to determine whether obesity is independently associated with colorectal dysplasia among patients with IBD undergoing surveillance colonoscopy.
Methods: We performed a retrospective matched case-control study at a tertiary care center among patients who underwent surveillance colonoscopy from 2020 to 2025. Cases were matched 1:1 by age, sex, and IBD subtype. Obesity was defined as mean BMI ≥30 kg/m² within five years before colonoscopy. Demographics, clinical characteristics, and histologic findings were collected. Multivariable conditional logistic regression was used to identify independent risk factors for dysplasia.
Results: We identified 216 patients with IBD who underwent surveillance colonoscopy (108 with dysplasia, 108 matched non-dysplasia controls). On univariable analysis, obesity was more common among dysplasia cases (30.6%) compared to controls (23.2%), although this difference was not statistically significant (p=0.22). In a multivariable model adjusting for covariates such as disease duration, prior dysplasia, and histologic severity (inactive/mild/moderate/severe), obesity was independently associated with dysplasia (adjusted odds ratio [aOR] 2.44, 95% CI 1.04 - 5.71). Additional predictors included longer disease duration (aOR 1.05, 95% CI 1.02 - 1.08) and prior dysplasia (aOR 5.10, 95% CI 1.50 - 17.33). Mild histologic inflammation reduced the risk of dysplasia (aOR 0.33, 95% CI 0.14 - 0.78), and a greater number of prior colonoscopies was modestly protective (aOR 0.88, 95% CI 0.77 - 0.99). Other variables including family history of colorectal cancer, smoking, diabetes, pseudopolyps, and strictures were not significantly associated with dysplasia.
Discussion: Obesity was independently associated with more than a 2-fold increased odds of colorectal dysplasia in patients with IBD, even after adjusting for clinical and histologic risk factors. These findings support incorporating BMI into dysplasia risk models and suggest that obese patients may benefit from enhanced surveillance strategies.
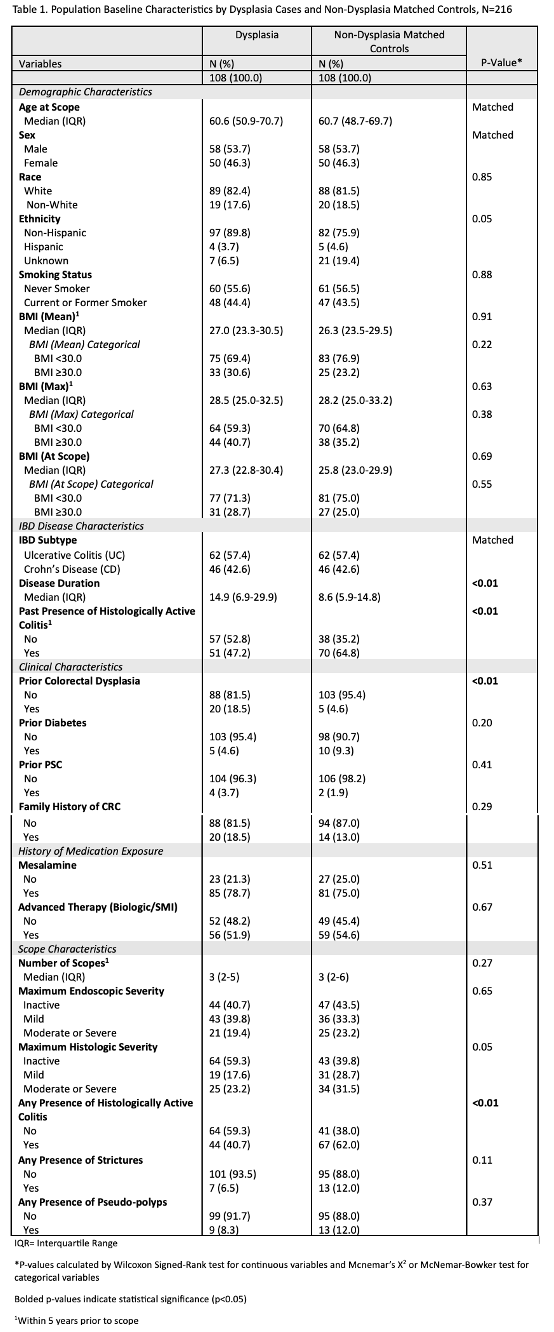
Figure: Table 1. Baseline demographic, clinical, and endoscopic characteristics of dysplasia cases and matched non-dysplasia controls (N=216). Groups were matched 1:1 by age, sex, race, and IBD subtype. Compared to controls, dysplasia cases had significantly longer disease duration, higher rates of prior colorectal dysplasia, and greater presence of histologically active colitis within the prior 5 years. No significant differences were observed in BMI, medication exposure, or maximum endoscopic severity. P-values <0.05 are bolded.
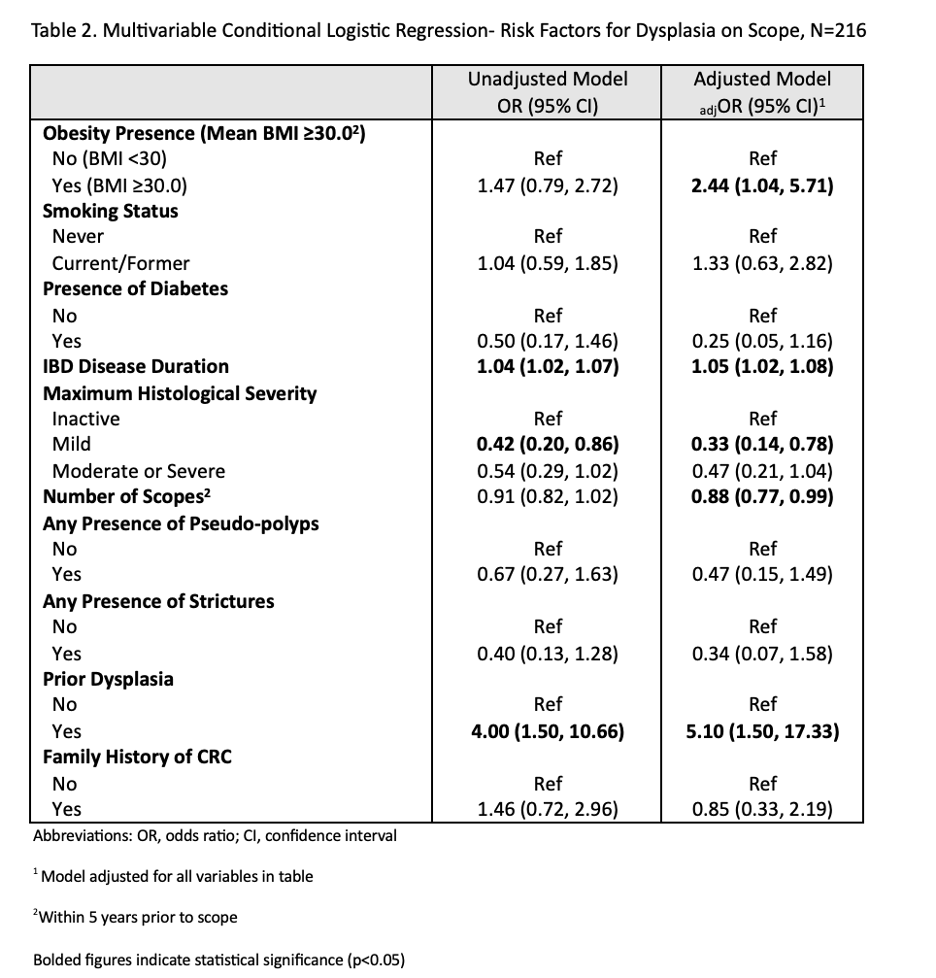
Figure: Table 2. Multivariable conditional logistic regression identifying risk factors associated with dysplasia on colonoscopy (N=216). In the adjusted model controlling for clinical and histologic variables, obesity (BMI ≥30.0), longer disease duration, and prior colorectal dysplasia were significantly associated with increased odds of dysplasia. Mild histologic inflammation was inversely associated with dysplasia compared to inactive disease. A greater number of colonoscopies within 5 years was also associated with reduced odds of dysplasia. Bolded values denote statistical significance (p < 0.05).
Disclosures:
Naveena Luke indicated no relevant financial relationships.
Jahnavi Udaikumar indicated no relevant financial relationships.
Carlos Echeverria indicated no relevant financial relationships.
Olivia Delau indicated no relevant financial relationships.
Xucong Meng indicated no relevant financial relationships.
Adam Faye: AbbVie – Honorarium. Eli Lilly – Consultant. NIH Grant K76AG083286 – Grant/Research Support. Takeda – Honorarium. The American College of Gastroenterology – Grant/Research Support. The Crohn's and Colitis Foundation – Grant/Research Support.
Jordan Axelrad: Abbvie – Advisory Committee/Board Member, Consultant, Honorarium. Abivax – Advisory Committee/Board Member, Consultant, Honorarium. Adiso – Advisory Committee/Board Member, Consultant, Honorarium. BioFire Diagnostics – Grant/Research Support. Biomerieux – Advisory Committee/Board Member, Consultant, Honorarium. Bristol-Myers Squibb – Advisory Committee/Board Member, Consultant, Honorarium. Celltrion – Advisory Committee/Board Member, Consultant, Honorarium. Ferring – Advisory Committee/Board Member, Consultant, Honorarium. Fresenius – Advisory Committee/Board Member, Consultant, Honorarium. Genentech – Grant/Research Support. Janssen – Advisory Committee/Board Member, Consultant. Janssen – Grant/Research Support. Janssen – Honorarium. Johnson & Johnson – Advisory Committee/Board Member, Consultant. Merck – Advisory Committee/Board Member, Consultant, Honorarium. NIH NIDDK Diseases K23DK124570 – Grant/Research Support. Pfizer – Advisory Committee/Board Member, Consultant, Honorarium. Sanofi – Advisory Committee/Board Member, Consultant, Honorarium. The Crohn's and Colitis Foundation (#878246) – Grant/Research Support. The Judith & Stewart Colton Center for Autoimmunity – Grant/Research Support. Vedanta – Advisory Committee/Board Member, Consultant, Honorarium.
Naveena Luke, MD1, Jahnavi Udaikumar, MD2, Carlos Echeverria, MD2, Olivia Delau, MS3, Xucong Meng, MPH4, Adam Faye, MD, MS3, Jordan Axelrad, MD, MPH5. P3173 - Obesity as an Independent Risk Factor for Colorectal Dysplasia in Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

