Monday Poster Session
Category: IBD
P3163 - Prevalence of and Risk Factors for Fatigue in Inflammatory Bowel Disease in a Tertiary Care Center
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Meredith R. Kline, MD (she/her/hers)
University of Chicago Medicine, Inflammatory Bowel Disease Center
Chicago, IL
Presenting Author(s)
Meredith R. Kline, MD1, Jeremy A.. Klein, MD1, Alexandra R. McDermott, BS2, Alyse Bedell, PhD2, David T. Rubin, MD3
1University of Chicago Medicine, Inflammatory Bowel Disease Center, Chicago, IL; 2University of Chicago, Chicago, IL; 3University of Chicago Medicine Inflammatory Bowel Disease Center, Chicago, IL, USA, Chicago, IL
Introduction: Fatigue is an increasingly recognized and multifactorial extra-intestinal manifestation of inflammatory bowel disease (IBD) that significantly impacts quality of life for up to 70% of patients (pts) with active IBD but also for pts in remission. We aimed to further characterize clinical, biochemical, and mental health risk factors for fatigue in a tertiary outpatient IBD clinic.
Methods: This was a prospective study of pts with IBD who completed the Functional Assessment of Chronic Illness Therapy-Fatigue (FACIT-F), Pittsburgh Sleep Quality Index (PSQI) questionnaires, and the Patient Health Questionnaire-9 (PHQ-9) and Generalized Anxiety Disorder-7 (GAD-7) before or during clinic visits from Sept 2024 to May 2025. We also collected demographic, disease, laboratory, endoscopic, and radiologic data. Standard severity of fatigue scores were used (FACIT-F < 30 is severe and 31-39 is moderate). Univariate analysis was conducted along with Chi-square and Wilcoxon rank-sum test. Simple linear regressions were fit for each predictor to estimate β-coefficients (change in FACIT-F score per unit change in predictor).
Results: Among 220 pts, 77 (35%) had at least moderate fatigue. 129 (58.6%) were female, and 148 (67.3%) had CD, the median age was 42.4 years [IQR 33.1-55.5 years] (Table 1). 151 pts completed a PHQ-9, and 42 (28%) had at least mild depression; 125 pts completed the GAD-7, and 34 (27%) had at least mild anxiety. On univariate analysis, clinically active IBD (β=-9.99, p< 0.001), greater anxiety (GAD-7; β=-1.57 per point, p< 0.001), history of mental health disorder (p< 0.001) and poorer sleep quality (PSQI; β=-9.84, p< 0.001) were significantly associated with more severe fatigue. Higher disease activity scores in IBD correlated with more severe fatigue (β=-2.08, p< 0.005, β=-5.71, p < 0.012, respectively). In pts with severe fatigue, 88% reported poor sleep quality versus 44% among those with mild or no fatigue (p< 0.001).
Discussion: We identify a high rate of fatigue in our pts with IBD and suggest a bidirectional relationship between inflammatory burden and fatigue which is also related to mental health disorders and poor sleep quality. These findings underpin the need for routine fatigue assessment and an integrated behavioral health, psychotherapy, and adjunctive medication plan in IBD management.
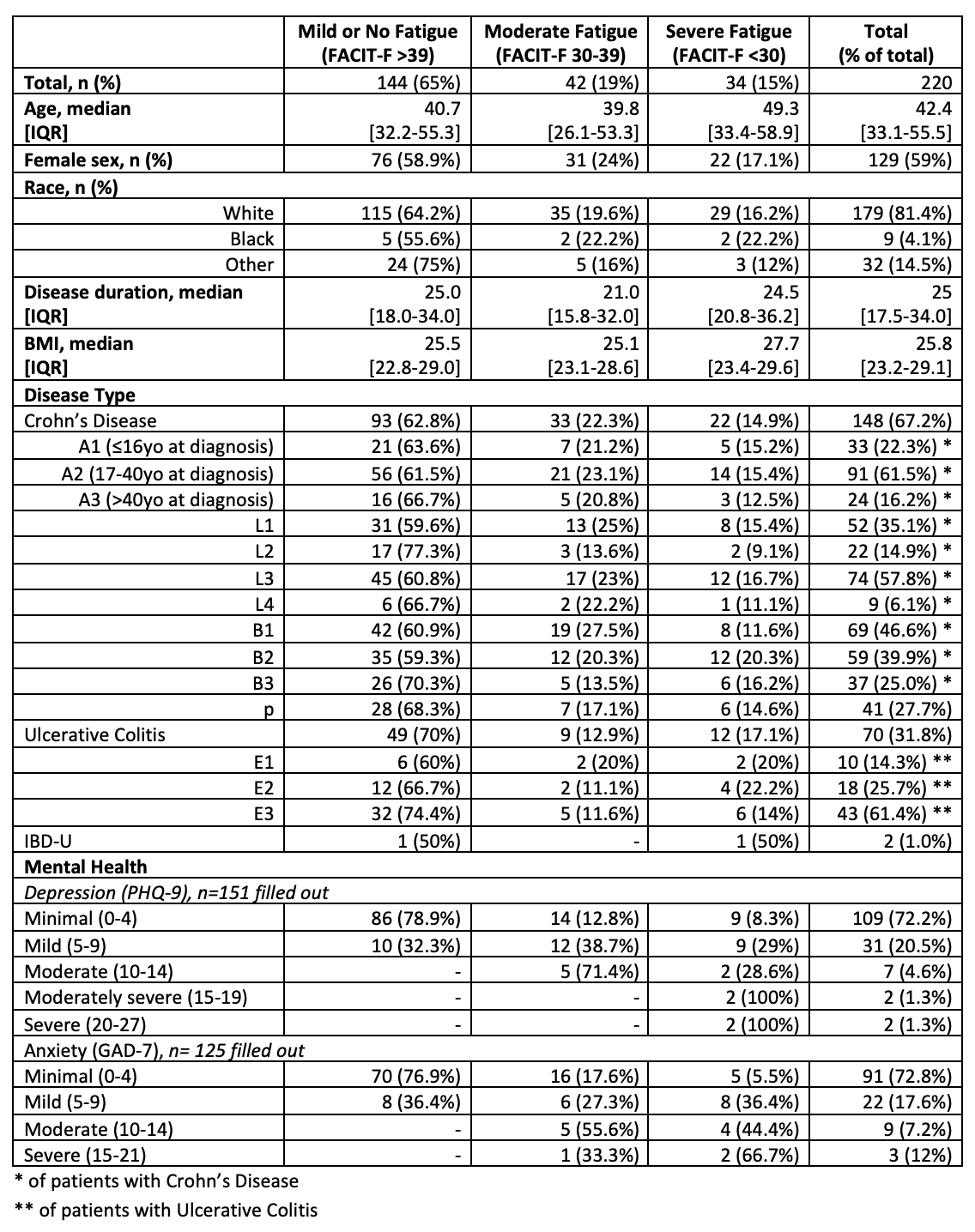
Figure: Table 1: Patient Characteristics and Disease Activity by Fatigue Severity
Disclosures:
Meredith Kline indicated no relevant financial relationships.
Jeremy Klein indicated no relevant financial relationships.
Alexandra McDermott indicated no relevant financial relationships.
Alyse Bedell indicated no relevant financial relationships.
David Rubin: AbbVie – Advisory Committee/Board Member, Consultant, Speaker fees. Abivax SA – Consultant. Altrubio – Advisory Committee/Board Member, Consultant, Speaker feees, Stock Options. Avalo – Advisory Committee/Board Member, Consultant, Speaker fees. Bausch Health – Consultant. Bristol Myers Squibb – Advisory Committee/Board Member, Consultant, Speaker fees. Buhlmann Diagnostics – Advisory Committee/Board Member, Consultant, Speaker fees. Celltrion – Consultant. ClostraBio – Consultant. Connect BioPharma – Consultant. Cornerstones Health, Inc – Board of Directors membership. Douglas Pharmaceuticals – Consultant. Eli Lilly & Co. – Consultant. Foresee, Genentech (Roche) Inc. – Consultant. Image Analysis Group – Consultant. InDex Pharmaceutical – Consultant. Intouch Group – Advisory Committee/Board Member, Consultant, Speaker fees. Iterative Health – Advisory Committee/Board Member, Consultant, Speaker fees. Iterative Health – Stock Options. Janssen Pharmaceuticals – Consultant. Lilly – Advisory Committee/Board Member, Consultant, Speaker fees. Odyssey Therapeutics – Consultant. Pfizer – Advisory Committee/Board Member, Consultant, Speaker fees. Sanofi – Consultant. Takeda – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speaker fees. Throne – Consultant. Vedanta – Consultant.
Meredith R. Kline, MD1, Jeremy A.. Klein, MD1, Alexandra R. McDermott, BS2, Alyse Bedell, PhD2, David T. Rubin, MD3. P3163 - Prevalence of and Risk Factors for Fatigue in Inflammatory Bowel Disease in a Tertiary Care Center, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Chicago Medicine, Inflammatory Bowel Disease Center, Chicago, IL; 2University of Chicago, Chicago, IL; 3University of Chicago Medicine Inflammatory Bowel Disease Center, Chicago, IL, USA, Chicago, IL
Introduction: Fatigue is an increasingly recognized and multifactorial extra-intestinal manifestation of inflammatory bowel disease (IBD) that significantly impacts quality of life for up to 70% of patients (pts) with active IBD but also for pts in remission. We aimed to further characterize clinical, biochemical, and mental health risk factors for fatigue in a tertiary outpatient IBD clinic.
Methods: This was a prospective study of pts with IBD who completed the Functional Assessment of Chronic Illness Therapy-Fatigue (FACIT-F), Pittsburgh Sleep Quality Index (PSQI) questionnaires, and the Patient Health Questionnaire-9 (PHQ-9) and Generalized Anxiety Disorder-7 (GAD-7) before or during clinic visits from Sept 2024 to May 2025. We also collected demographic, disease, laboratory, endoscopic, and radiologic data. Standard severity of fatigue scores were used (FACIT-F < 30 is severe and 31-39 is moderate). Univariate analysis was conducted along with Chi-square and Wilcoxon rank-sum test. Simple linear regressions were fit for each predictor to estimate β-coefficients (change in FACIT-F score per unit change in predictor).
Results: Among 220 pts, 77 (35%) had at least moderate fatigue. 129 (58.6%) were female, and 148 (67.3%) had CD, the median age was 42.4 years [IQR 33.1-55.5 years] (Table 1). 151 pts completed a PHQ-9, and 42 (28%) had at least mild depression; 125 pts completed the GAD-7, and 34 (27%) had at least mild anxiety. On univariate analysis, clinically active IBD (β=-9.99, p< 0.001), greater anxiety (GAD-7; β=-1.57 per point, p< 0.001), history of mental health disorder (p< 0.001) and poorer sleep quality (PSQI; β=-9.84, p< 0.001) were significantly associated with more severe fatigue. Higher disease activity scores in IBD correlated with more severe fatigue (β=-2.08, p< 0.005, β=-5.71, p < 0.012, respectively). In pts with severe fatigue, 88% reported poor sleep quality versus 44% among those with mild or no fatigue (p< 0.001).
Discussion: We identify a high rate of fatigue in our pts with IBD and suggest a bidirectional relationship between inflammatory burden and fatigue which is also related to mental health disorders and poor sleep quality. These findings underpin the need for routine fatigue assessment and an integrated behavioral health, psychotherapy, and adjunctive medication plan in IBD management.
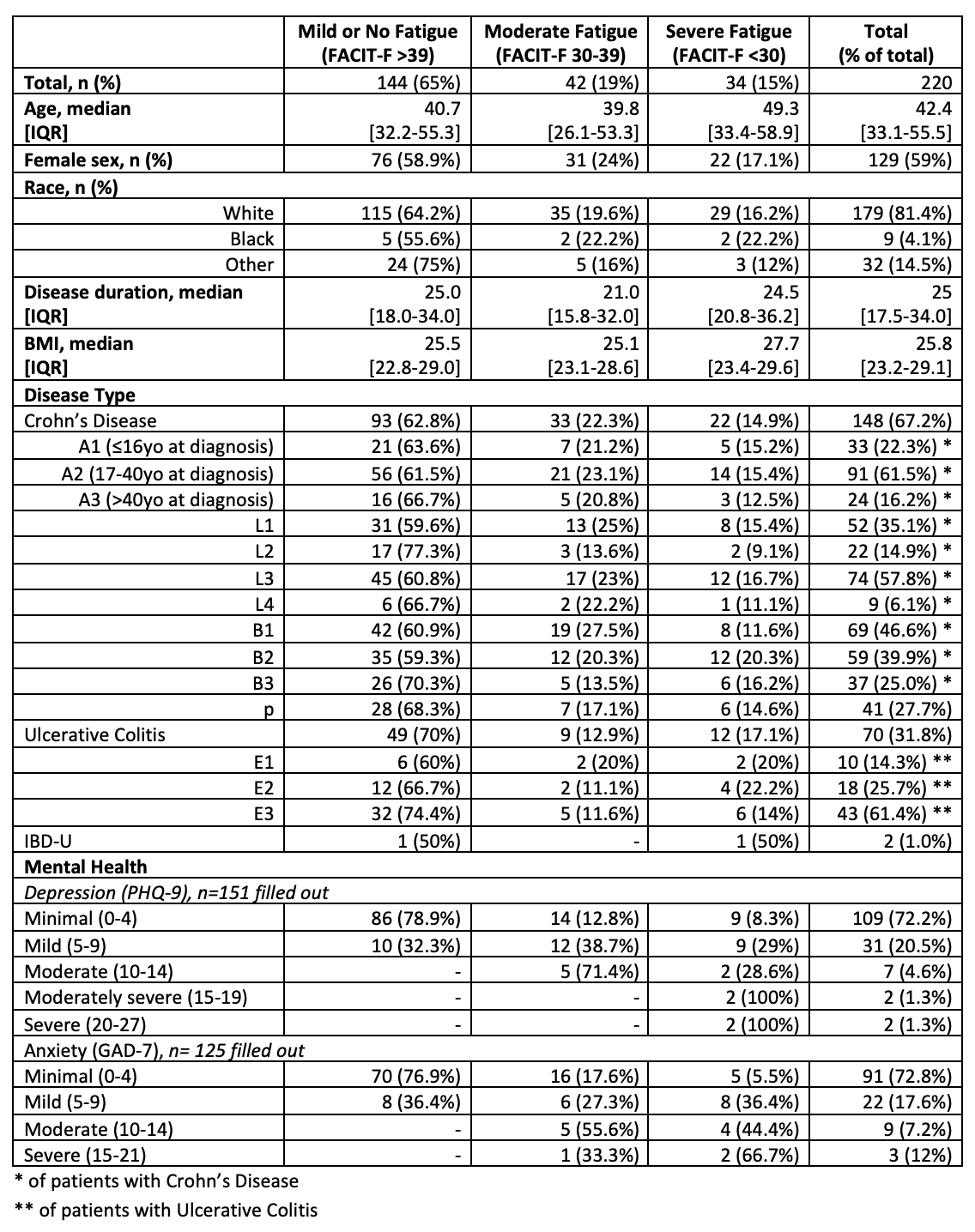
Figure: Table 1: Patient Characteristics and Disease Activity by Fatigue Severity
Disclosures:
Meredith Kline indicated no relevant financial relationships.
Jeremy Klein indicated no relevant financial relationships.
Alexandra McDermott indicated no relevant financial relationships.
Alyse Bedell indicated no relevant financial relationships.
David Rubin: AbbVie – Advisory Committee/Board Member, Consultant, Speaker fees. Abivax SA – Consultant. Altrubio – Advisory Committee/Board Member, Consultant, Speaker feees, Stock Options. Avalo – Advisory Committee/Board Member, Consultant, Speaker fees. Bausch Health – Consultant. Bristol Myers Squibb – Advisory Committee/Board Member, Consultant, Speaker fees. Buhlmann Diagnostics – Advisory Committee/Board Member, Consultant, Speaker fees. Celltrion – Consultant. ClostraBio – Consultant. Connect BioPharma – Consultant. Cornerstones Health, Inc – Board of Directors membership. Douglas Pharmaceuticals – Consultant. Eli Lilly & Co. – Consultant. Foresee, Genentech (Roche) Inc. – Consultant. Image Analysis Group – Consultant. InDex Pharmaceutical – Consultant. Intouch Group – Advisory Committee/Board Member, Consultant, Speaker fees. Iterative Health – Advisory Committee/Board Member, Consultant, Speaker fees. Iterative Health – Stock Options. Janssen Pharmaceuticals – Consultant. Lilly – Advisory Committee/Board Member, Consultant, Speaker fees. Odyssey Therapeutics – Consultant. Pfizer – Advisory Committee/Board Member, Consultant, Speaker fees. Sanofi – Consultant. Takeda – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speaker fees. Throne – Consultant. Vedanta – Consultant.
Meredith R. Kline, MD1, Jeremy A.. Klein, MD1, Alexandra R. McDermott, BS2, Alyse Bedell, PhD2, David T. Rubin, MD3. P3163 - Prevalence of and Risk Factors for Fatigue in Inflammatory Bowel Disease in a Tertiary Care Center, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
