Monday Poster Session
Category: GI Bleeding
P3135 - Enteroiliac Fistula Presenting as Occult Small Bowel Bleeding in a Pancreas Transplant Recipient
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Nader Al Souky, MD
University of Kansas School of Medicine
Wichita, KS
Presenting Author(s)
Nader Al Souky, MD1, Najib Nassani, MD2
1University of Kansas School of Medicine, Wichita, KS; 2Carle Foundation hospital, Urbana, IL
Introduction: Arterioenteric fistulas are a rare but life-threatening cause of gastrointestinal (GI) bleeding. In pancreas transplant recipients, pseudoaneurysms can develop years after transplantation and may erode into adjacent bowel segments, creating vascular-enteric fistulas. Diagnosis is challenging due to intermittent bleeding and limitations of conventional endoscopy.
Case Description/
Methods: A 56-year-old man with type 1 diabetes mellitus, kidney transplant, and failed pancreas transplant (19 years prior) presented with recurrent hematochezia. He was on dual antiplatelet therapy following a recent ischemic stroke. Initial hemoglobin was 12 g/dL, and dropped to 7.1 g/dL, requiring five units of PRBCs. Despite ongoing bleeding, he remained hemodynamically stable and had no abdominal pain.
Extensive workup included two colonoscopies, upper endoscopy, and push enteroscopy, were all unrevealing. CT angiography showed distal ileal mural thickening and a right external iliac artery pseudoaneurysm. Meckel scan and tagged RBC scan were negative. Capsule endoscopy revealed active bleeding in the distal ileum. The retrograde double-balloon enteroscopy identified a large, ulcerated lesion with a pulsatile vessel, unsuitable for endoscopic therapy (Figure A). The site was marked with clips and a tattoo.
Interventional radiology confirmed the pseudoaneurysm adjacent to the clips (Figure B), and a vascular covered stent was placed. The following day, the patient developed acute limb ischemia due to in-stent thrombosis, requiring emergent embolectomy. Exploratory laparotomy revealed a fistula between the distal ileum and the right external iliac artery at the prior transplant site. Small bowel resection, pseudoaneurysm debridement, placement of antibiotic beads, and an omental patch were performed.
Discussion: This case illustrates an enteroiliac fistula as a rare cause of small bowel bleeding post-pancreas transplant. Pseudoaneurysms may develop years later, eroding into bowels and causing hemorrhage. Standard endoscopy often fails to localize bleeding; thus, capsule endoscopy and deep enteroscopy are crucial. Imaging and angiography aid in diagnosis and allow for temporizing endovascular intervention. However, definitive management requires surgical resection to prevent recurrence or infection. Clinicians must maintain a high index of suspicion for arterioenteric fistula in transplant recipients with unexplained GI bleeding.
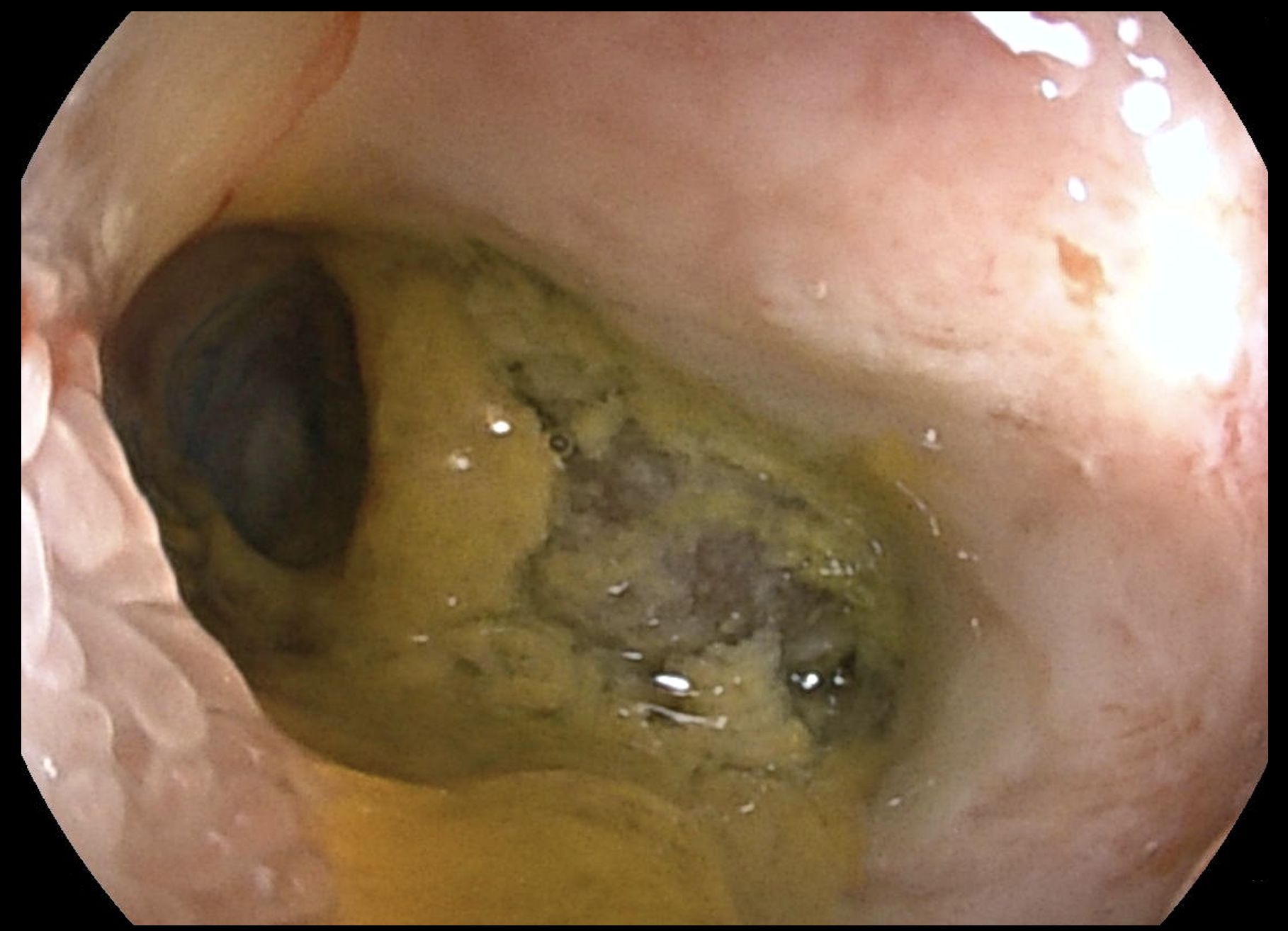
Figure: Lower Double Balloon Enteroscopy Identified Lesion
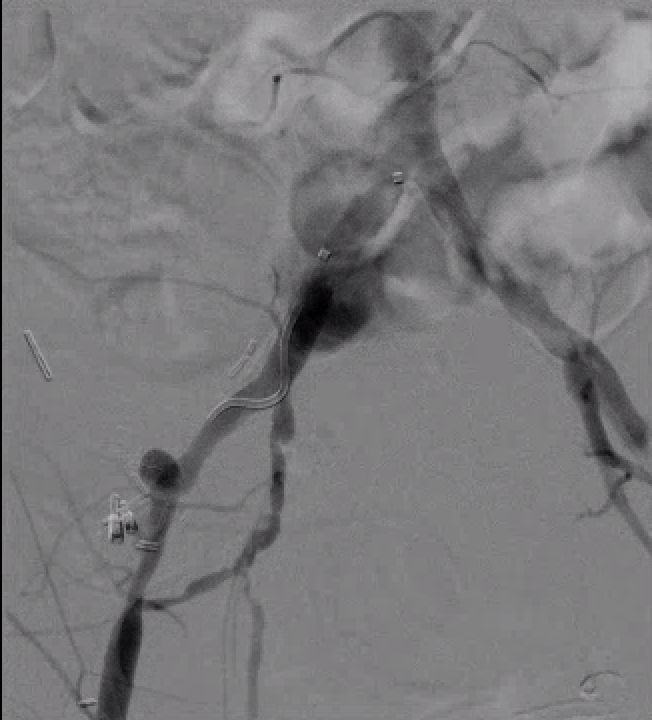
Figure: Angiography Showing The Pseudoaneurysm Adjacent To The Two Hemostatic Clips
Disclosures:
Nader Al Souky indicated no relevant financial relationships.
Najib Nassani indicated no relevant financial relationships.
Nader Al Souky, MD1, Najib Nassani, MD2. P3135 - Enteroiliac Fistula Presenting as Occult Small Bowel Bleeding in a Pancreas Transplant Recipient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Kansas School of Medicine, Wichita, KS; 2Carle Foundation hospital, Urbana, IL
Introduction: Arterioenteric fistulas are a rare but life-threatening cause of gastrointestinal (GI) bleeding. In pancreas transplant recipients, pseudoaneurysms can develop years after transplantation and may erode into adjacent bowel segments, creating vascular-enteric fistulas. Diagnosis is challenging due to intermittent bleeding and limitations of conventional endoscopy.
Case Description/
Methods: A 56-year-old man with type 1 diabetes mellitus, kidney transplant, and failed pancreas transplant (19 years prior) presented with recurrent hematochezia. He was on dual antiplatelet therapy following a recent ischemic stroke. Initial hemoglobin was 12 g/dL, and dropped to 7.1 g/dL, requiring five units of PRBCs. Despite ongoing bleeding, he remained hemodynamically stable and had no abdominal pain.
Extensive workup included two colonoscopies, upper endoscopy, and push enteroscopy, were all unrevealing. CT angiography showed distal ileal mural thickening and a right external iliac artery pseudoaneurysm. Meckel scan and tagged RBC scan were negative. Capsule endoscopy revealed active bleeding in the distal ileum. The retrograde double-balloon enteroscopy identified a large, ulcerated lesion with a pulsatile vessel, unsuitable for endoscopic therapy (Figure A). The site was marked with clips and a tattoo.
Interventional radiology confirmed the pseudoaneurysm adjacent to the clips (Figure B), and a vascular covered stent was placed. The following day, the patient developed acute limb ischemia due to in-stent thrombosis, requiring emergent embolectomy. Exploratory laparotomy revealed a fistula between the distal ileum and the right external iliac artery at the prior transplant site. Small bowel resection, pseudoaneurysm debridement, placement of antibiotic beads, and an omental patch were performed.
Discussion: This case illustrates an enteroiliac fistula as a rare cause of small bowel bleeding post-pancreas transplant. Pseudoaneurysms may develop years later, eroding into bowels and causing hemorrhage. Standard endoscopy often fails to localize bleeding; thus, capsule endoscopy and deep enteroscopy are crucial. Imaging and angiography aid in diagnosis and allow for temporizing endovascular intervention. However, definitive management requires surgical resection to prevent recurrence or infection. Clinicians must maintain a high index of suspicion for arterioenteric fistula in transplant recipients with unexplained GI bleeding.
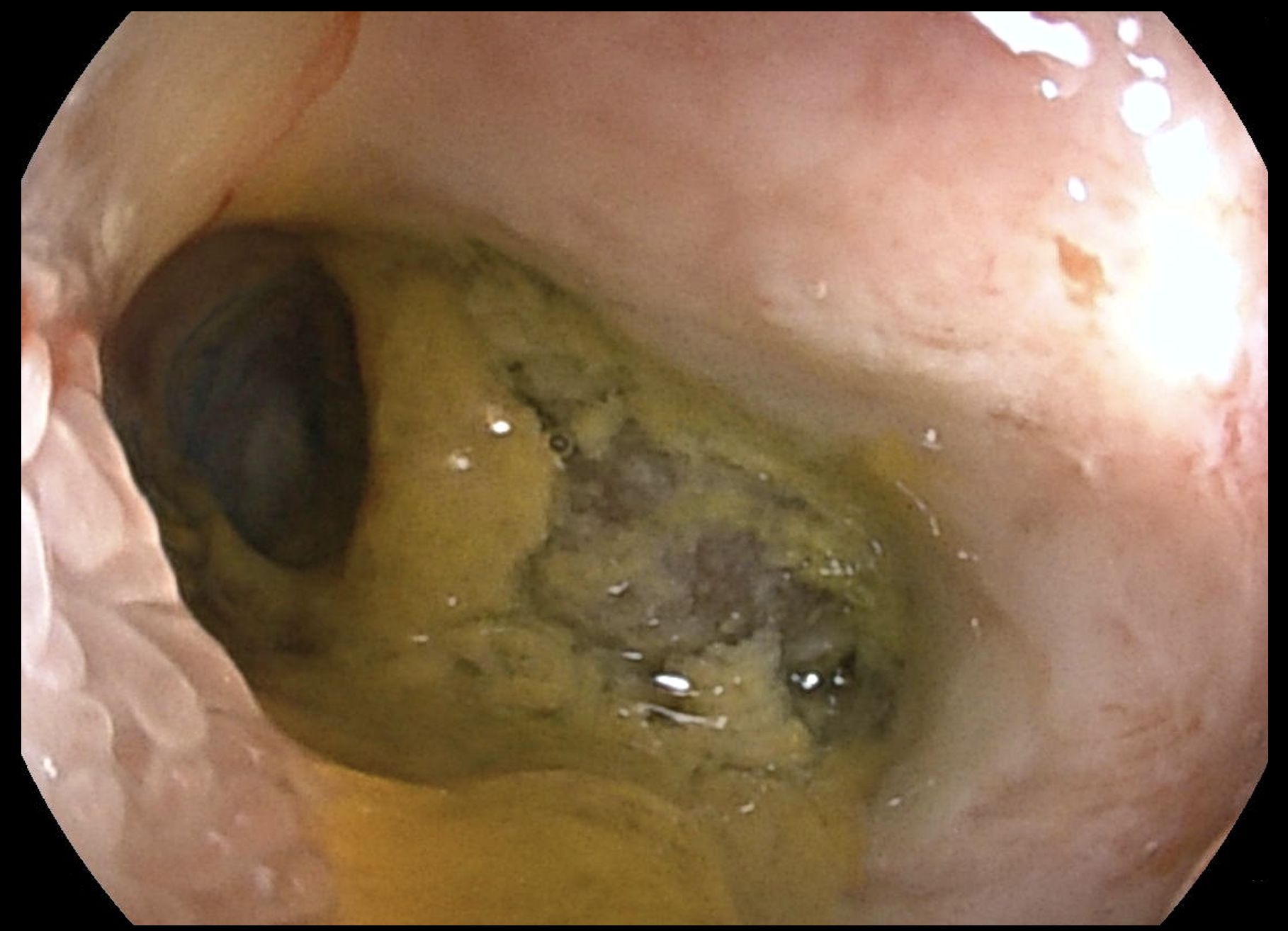
Figure: Lower Double Balloon Enteroscopy Identified Lesion
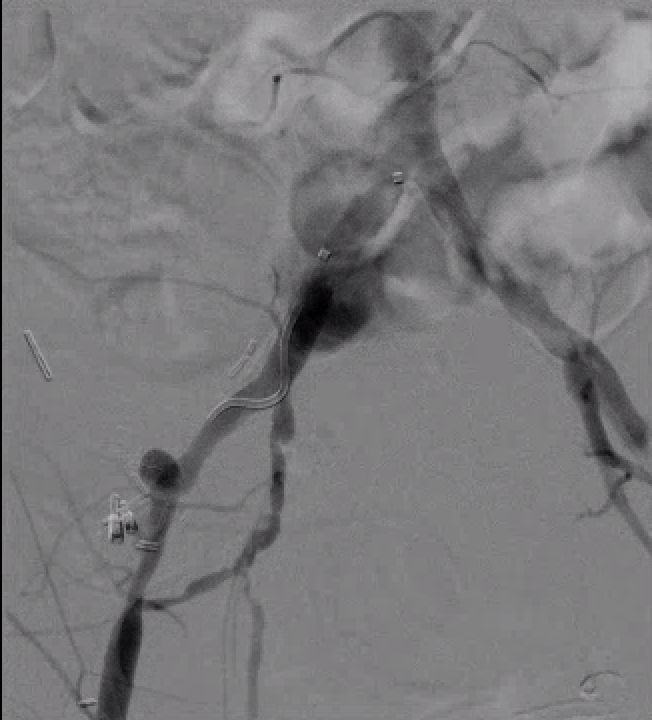
Figure: Angiography Showing The Pseudoaneurysm Adjacent To The Two Hemostatic Clips
Disclosures:
Nader Al Souky indicated no relevant financial relationships.
Najib Nassani indicated no relevant financial relationships.
Nader Al Souky, MD1, Najib Nassani, MD2. P3135 - Enteroiliac Fistula Presenting as Occult Small Bowel Bleeding in a Pancreas Transplant Recipient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
