Monday Poster Session
Category: GI Bleeding
P3112 - An Acquired Double Pylorus Sign: A Rare Consequence of Recurrent Peptic Ulcer Disease
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- SS
Sinclair Strange, DO (she/her/hers)
UNC Health Blue Ridge
Morganton, NC
Presenting Author(s)
Sinclair Strange, DO, Sadie De Silva, MD, Muhannad Kurtom, DO, Dustin Kilpatrick, DO
UNC Health Blue Ridge, Morganton, NC
Introduction: Double pylorus is a rare gastrointestinal finding characterized by the presence of two distinct channels connecting the gastric antrum to the duodenal bulb. It may arise as either a congenital anomaly or as an acquired complication of peptic ulcer disease which has an estimated prevalence of 0.001–0.4%. We present a case of double pylorus identified during endoscopic evaluation, explore its potential etiologies, and review relevant management strategies and clinical implications.
Case Description/
Methods: A 67-year-old male with a history of decompensated alcoholic cirrhosis, prior perforated gastric ulcer requiring Graham patch repair, and chronic NSAID use for pain management presented with melena. On arrival, he was hypotensive and tachycardic. Laboratory evaluation revealed a hemoglobin level of 10.7 g/dL (reference range: 13.5–17.5 g/dL), decreased from his baseline of 12.1 g/dL. He was emergently transfused with two units of packed red blood cells, started on an octreotide infusion, and received intravenous pantoprazole. Esophagogastroduodenoscopy (EGD) demonstrated non-bleeding type 2 gastroesophageal varices, portal hypertensive gastropathy, a cratered duodenal ulcer without active bleeding, and a double pylorus (Figure 1b). We suspected that the double pylorus was acquired in setting of previous perforated gastric ulcer as was not seen on a prior EGD performed several years earlier (Figure 1a). At discharge, the patient was advised to discontinue NSAIDs, transitioned to oral pantoprazole and scheduled for outpatient gastroenterology follow-up, including a repeat EGD in six weeks.
Discussion: Penetrating gastroduodenal ulcers can form a fistulous tract between the stomach and duodenum, resulting in an acquired double pylorus. This condition is often discovered incidentally during endoscopy, as was the case with our patient. Management typically involves discontinuation of NSAIDs, initiation of proton pump inhibitor (PPI) therapy, and eradication of Helicobacter pylori, if present. While repeat endoscopy may be considered to assess healing and evaluate for fistula closure, the tract often persists as a stable anatomic variant. This case underscores the importance of recognizing double pylorus as a potential complication of peptic ulcer disease, particularly in the context of chronic NSAID use. Early identification and targeted management of the underlying etiology are essential to minimizing further gastrointestinal morbidity.
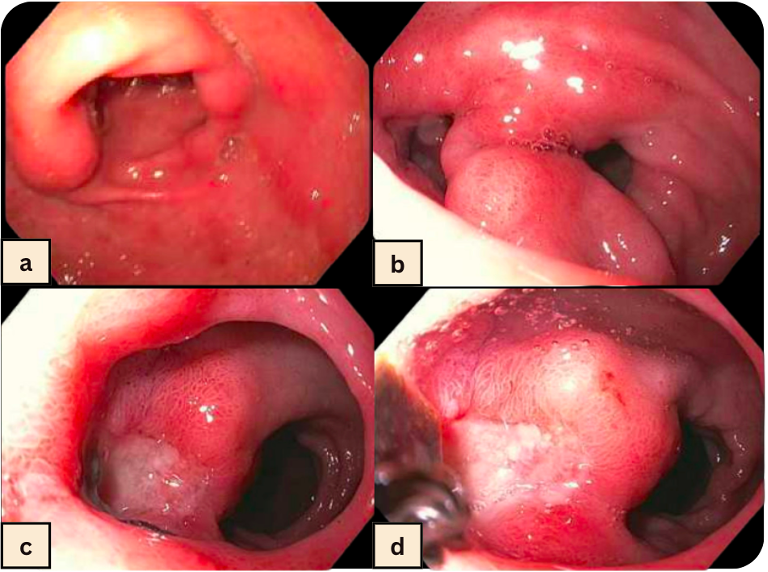
Figure: Figure 1. a. Patent, single-channel pylorus (March 2021); b. Pre-pyloric view with a double pylorus (March 2025), characterized by two distinct channels connecting the gastric antrum to the duodenal bulb; c,d. Cratered duodenal ulcer with no visible vessel or adherent clot.
Disclosures:
Sinclair Strange indicated no relevant financial relationships.
Sadie De Silva indicated no relevant financial relationships.
Muhannad Kurtom indicated no relevant financial relationships.
Dustin Kilpatrick indicated no relevant financial relationships.
Sinclair Strange, DO, Sadie De Silva, MD, Muhannad Kurtom, DO, Dustin Kilpatrick, DO. P3112 - An Acquired Double Pylorus Sign: A Rare Consequence of Recurrent Peptic Ulcer Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
UNC Health Blue Ridge, Morganton, NC
Introduction: Double pylorus is a rare gastrointestinal finding characterized by the presence of two distinct channels connecting the gastric antrum to the duodenal bulb. It may arise as either a congenital anomaly or as an acquired complication of peptic ulcer disease which has an estimated prevalence of 0.001–0.4%. We present a case of double pylorus identified during endoscopic evaluation, explore its potential etiologies, and review relevant management strategies and clinical implications.
Case Description/
Methods: A 67-year-old male with a history of decompensated alcoholic cirrhosis, prior perforated gastric ulcer requiring Graham patch repair, and chronic NSAID use for pain management presented with melena. On arrival, he was hypotensive and tachycardic. Laboratory evaluation revealed a hemoglobin level of 10.7 g/dL (reference range: 13.5–17.5 g/dL), decreased from his baseline of 12.1 g/dL. He was emergently transfused with two units of packed red blood cells, started on an octreotide infusion, and received intravenous pantoprazole. Esophagogastroduodenoscopy (EGD) demonstrated non-bleeding type 2 gastroesophageal varices, portal hypertensive gastropathy, a cratered duodenal ulcer without active bleeding, and a double pylorus (Figure 1b). We suspected that the double pylorus was acquired in setting of previous perforated gastric ulcer as was not seen on a prior EGD performed several years earlier (Figure 1a). At discharge, the patient was advised to discontinue NSAIDs, transitioned to oral pantoprazole and scheduled for outpatient gastroenterology follow-up, including a repeat EGD in six weeks.
Discussion: Penetrating gastroduodenal ulcers can form a fistulous tract between the stomach and duodenum, resulting in an acquired double pylorus. This condition is often discovered incidentally during endoscopy, as was the case with our patient. Management typically involves discontinuation of NSAIDs, initiation of proton pump inhibitor (PPI) therapy, and eradication of Helicobacter pylori, if present. While repeat endoscopy may be considered to assess healing and evaluate for fistula closure, the tract often persists as a stable anatomic variant. This case underscores the importance of recognizing double pylorus as a potential complication of peptic ulcer disease, particularly in the context of chronic NSAID use. Early identification and targeted management of the underlying etiology are essential to minimizing further gastrointestinal morbidity.
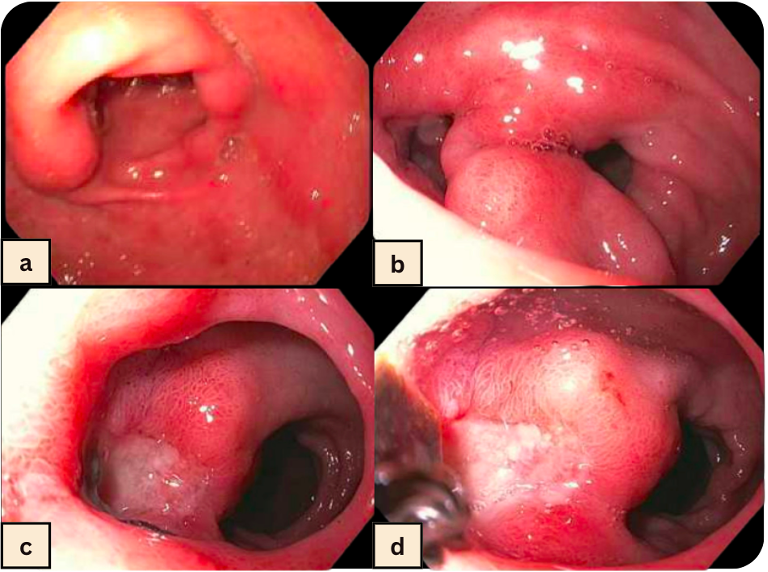
Figure: Figure 1. a. Patent, single-channel pylorus (March 2021); b. Pre-pyloric view with a double pylorus (March 2025), characterized by two distinct channels connecting the gastric antrum to the duodenal bulb; c,d. Cratered duodenal ulcer with no visible vessel or adherent clot.
Disclosures:
Sinclair Strange indicated no relevant financial relationships.
Sadie De Silva indicated no relevant financial relationships.
Muhannad Kurtom indicated no relevant financial relationships.
Dustin Kilpatrick indicated no relevant financial relationships.
Sinclair Strange, DO, Sadie De Silva, MD, Muhannad Kurtom, DO, Dustin Kilpatrick, DO. P3112 - An Acquired Double Pylorus Sign: A Rare Consequence of Recurrent Peptic Ulcer Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
