Monday Poster Session
Category: GI Bleeding
P3110 - Recurrent Hemorrhagic Shock From Massive Lower GI Bleed Following Transanal Hemorrrhoidal Dearterialization Surgery
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- YR
Yasir Rajwana, MD
Marshall University Joan C. Edwards School of Medicine
Huntington, WV
Presenting Author(s)
Yasir Rajwana, MD1, Ejaz Sara, MBBS2, Rahoma Saad, MD3, Ahmed Sherif, MD1, Wesam Frandah, MD1
1Marshall University Joan C. Edwards School of Medicine, Huntington, WV; 2Fatima Memorial Medical College, Barboursville, WV; 3Marshall University - - Huntington, WV, Huntington, WV
Introduction: Massive lower GI bleed has a broad differential but rarely presents with recurrent hemorrhagic shock as a complication of recent Transanal Hemorrhoidal Dearterialization surgery.
Case Description/
Methods: 49-year-old F with history of hidradenitis suppurativa, obesity, remote DVT, single Prothrombin G20210 mutation(not on anticoagulation) presented 10 days after Transanal Hemorrhoidal Dearterialization and Mucopexy for external hemorrhoids, with hematochezia and associated syncope with initial Hgb of 11.9 with subsequent drop to 7.9. Vitals showed BP of 100/61, HR of 105. CTA showed no active bleeding. She underwent EGD and colonoscopy after Bowel prep. The EGD was unremarkable, colonoscopy showed diverticulosis and sutures in the rectum from recent surgery but no active bleeding was seen. She was discharged 24 hours later suspecting a self limiting diverticular bleed.
She presented 2 days later with hypotension, recurrent hematochezia and Hgb drop to 6.5 g/dl (7.9 on discharge). A Meckel's scan was performed which was negative.Repeat colonoscopy next day showed similar findings to prior and no active bleeding. The area of hemorrhoid surgery was inspected and did not show any high risk lesions except for small areas of mucosal healing associated with sutures. The plan was to perform capsule endoscopy for small bowel evaluation if bleeding recurred but she remained stable and discharged 48 hours later.
Patient again presented 4 days later with hematochezia and presyncope. Repeat CTA showed active bleeding in the rectum, IR team performed angiography for embolization but the active bleeding had stopped. A plan was made to perform flexible sigmoidoscopy and rectal EUS to evaluate for a post surgical pseudoaneurysm and perform definitive hemostasis. The EUS showed increased vascularity in the areas of sutures and mucopexy in the rectum but no pseudoaneurysm was identified. The sutures were removed with endoscissors and hemostatic clips were placed to prevent rebleeding.
The patient was observed for 4 days after the procedure and had no recurrent bleeding. She was seen in clinic subsequently few days later and was doing well without any further bleeding episodes.
Discussion: Transanal Hemorrhoidal Dearterialization is commonly performed for external hemorrhoids. Lower GI bleed following this surgery should be considered as a differential in this population. Use of EUS for evaluation and hemostatic metal clips if no clear lesion is identified can be helpful as proved to be the case in our patient.
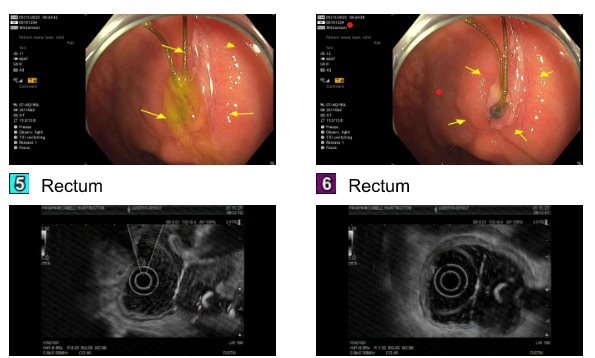
Figure: THD and Mucopexy site with sutures
EUS of the surgery site
Disclosures:
Yasir Rajwana indicated no relevant financial relationships.
Ejaz Sara indicated no relevant financial relationships.
Rahoma Saad indicated no relevant financial relationships.
Ahmed Sherif indicated no relevant financial relationships.
Wesam Frandah: Boston Scientific – Advisor or Review Panel Member, Consultant. Merritt – Consultant. Olympus corporation of America – Consultant.
Yasir Rajwana, MD1, Ejaz Sara, MBBS2, Rahoma Saad, MD3, Ahmed Sherif, MD1, Wesam Frandah, MD1. P3110 - Recurrent Hemorrhagic Shock From Massive Lower GI Bleed Following Transanal Hemorrrhoidal Dearterialization Surgery, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Marshall University Joan C. Edwards School of Medicine, Huntington, WV; 2Fatima Memorial Medical College, Barboursville, WV; 3Marshall University - - Huntington, WV, Huntington, WV
Introduction: Massive lower GI bleed has a broad differential but rarely presents with recurrent hemorrhagic shock as a complication of recent Transanal Hemorrhoidal Dearterialization surgery.
Case Description/
Methods: 49-year-old F with history of hidradenitis suppurativa, obesity, remote DVT, single Prothrombin G20210 mutation(not on anticoagulation) presented 10 days after Transanal Hemorrhoidal Dearterialization and Mucopexy for external hemorrhoids, with hematochezia and associated syncope with initial Hgb of 11.9 with subsequent drop to 7.9. Vitals showed BP of 100/61, HR of 105. CTA showed no active bleeding. She underwent EGD and colonoscopy after Bowel prep. The EGD was unremarkable, colonoscopy showed diverticulosis and sutures in the rectum from recent surgery but no active bleeding was seen. She was discharged 24 hours later suspecting a self limiting diverticular bleed.
She presented 2 days later with hypotension, recurrent hematochezia and Hgb drop to 6.5 g/dl (7.9 on discharge). A Meckel's scan was performed which was negative.Repeat colonoscopy next day showed similar findings to prior and no active bleeding. The area of hemorrhoid surgery was inspected and did not show any high risk lesions except for small areas of mucosal healing associated with sutures. The plan was to perform capsule endoscopy for small bowel evaluation if bleeding recurred but she remained stable and discharged 48 hours later.
Patient again presented 4 days later with hematochezia and presyncope. Repeat CTA showed active bleeding in the rectum, IR team performed angiography for embolization but the active bleeding had stopped. A plan was made to perform flexible sigmoidoscopy and rectal EUS to evaluate for a post surgical pseudoaneurysm and perform definitive hemostasis. The EUS showed increased vascularity in the areas of sutures and mucopexy in the rectum but no pseudoaneurysm was identified. The sutures were removed with endoscissors and hemostatic clips were placed to prevent rebleeding.
The patient was observed for 4 days after the procedure and had no recurrent bleeding. She was seen in clinic subsequently few days later and was doing well without any further bleeding episodes.
Discussion: Transanal Hemorrhoidal Dearterialization is commonly performed for external hemorrhoids. Lower GI bleed following this surgery should be considered as a differential in this population. Use of EUS for evaluation and hemostatic metal clips if no clear lesion is identified can be helpful as proved to be the case in our patient.
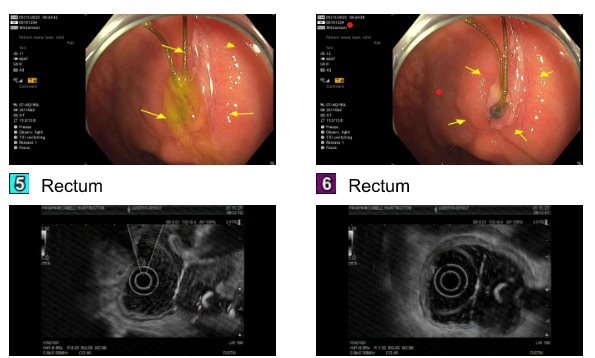
Figure: THD and Mucopexy site with sutures
EUS of the surgery site
Disclosures:
Yasir Rajwana indicated no relevant financial relationships.
Ejaz Sara indicated no relevant financial relationships.
Rahoma Saad indicated no relevant financial relationships.
Ahmed Sherif indicated no relevant financial relationships.
Wesam Frandah: Boston Scientific – Advisor or Review Panel Member, Consultant. Merritt – Consultant. Olympus corporation of America – Consultant.
Yasir Rajwana, MD1, Ejaz Sara, MBBS2, Rahoma Saad, MD3, Ahmed Sherif, MD1, Wesam Frandah, MD1. P3110 - Recurrent Hemorrhagic Shock From Massive Lower GI Bleed Following Transanal Hemorrrhoidal Dearterialization Surgery, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
