Monday Poster Session
Category: GI Bleeding
P3094 - The Ulcer That Wasn't: Gastric Amyloidosis Masquerading as Refractory Upper Gastrointestinal Bleeding
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Vatsal Khanna, MD
Henry Ford Health
Southfield, MI
Presenting Author(s)
Award: ACG Presidential Poster Award
Vatsal Khanna, MD1, James Aldridge, MD2, Mark DeVore, MD1, Serge Sorser, MD1
1Henry Ford Health, Southfield, MI; 2Corewell Health, Redford, MI
Introduction: Gastric involvement in systemic amyloidosis is a rare and often underdiagnosed cause of upper gastrointestinal (GI) bleeding. Clinical manifestations are nonspecific and may include early satiety, weight loss, or recurrent bleeding, often mimicking peptic ulcer disease or malignancy. Endoscopic findings are frequently subtle, and biopsies are sometimes deferred during active bleeding. We present a case of gastric amyloidosis identified after nearly a year of recurrent GI bleeding and repeated non-diagnostic endoscopies.
Case Description/
Methods: An 84-year-old man with low-grade myelodysplastic syndrome, stage V chronic kidney disease, coronary artery disease, and type 2 diabetes presented to our hospital with progressive weakness, orthostatic dizziness, and melena. He was on low-dose aspirin, denied NSAID use, and was not taking anticoagulants.
Over the past year, he had multiple hospitalizations for recurrent upper GI bleeding. Prior EGDs revealed large ulcers in the gastric fundus and antrum with adherent clots, treated with over-the-scope clips and epinephrine injection. Biopsies were deferred due to active bleeding and poor visualization.
On this admission, he was hemodynamically stable with melena on exam and a hemoglobin of 9.7 g/dL. IV pantoprazole was initiated. Given his recurrent bleeding with no clear etiology on prior evaluations, serum, and urine protein electrophoresis with immunofixation were performed to assess for possible plasma cell dyscrasia. Free light chain assay showed elevated kappa and lambda levels, with a kappa-to-lambda ratio of 2.43—within the renal-adjusted range.
Repeat EGD revealed a 1 cm ulcerated mass in the gastric fundus with granulation tissue and a previously placed clip. No active bleeding was noted (Figure 1). Biopsies showed chronic gastritis and ulceration. Congo red staining confirmed submucosal amyloid deposits with apple-green birefringence, diagnostic of gastric amyloidosis. The patient was discharged on oral pantoprazole twice daily with outpatient hematology-oncology follow-up for suspected AL amyloidosis.
Discussion: This case highlights the diagnostic challenge of gastric amyloidosis, particularly when biopsies are delayed due to acute bleeding. In patients with chronic kidney disease, free light chain ratios may be misleading. Deep biopsies with Congo red staining remain essential for diagnosis. Early recognition can prevent delays in initiating systemic therapy for AL amyloidosis.
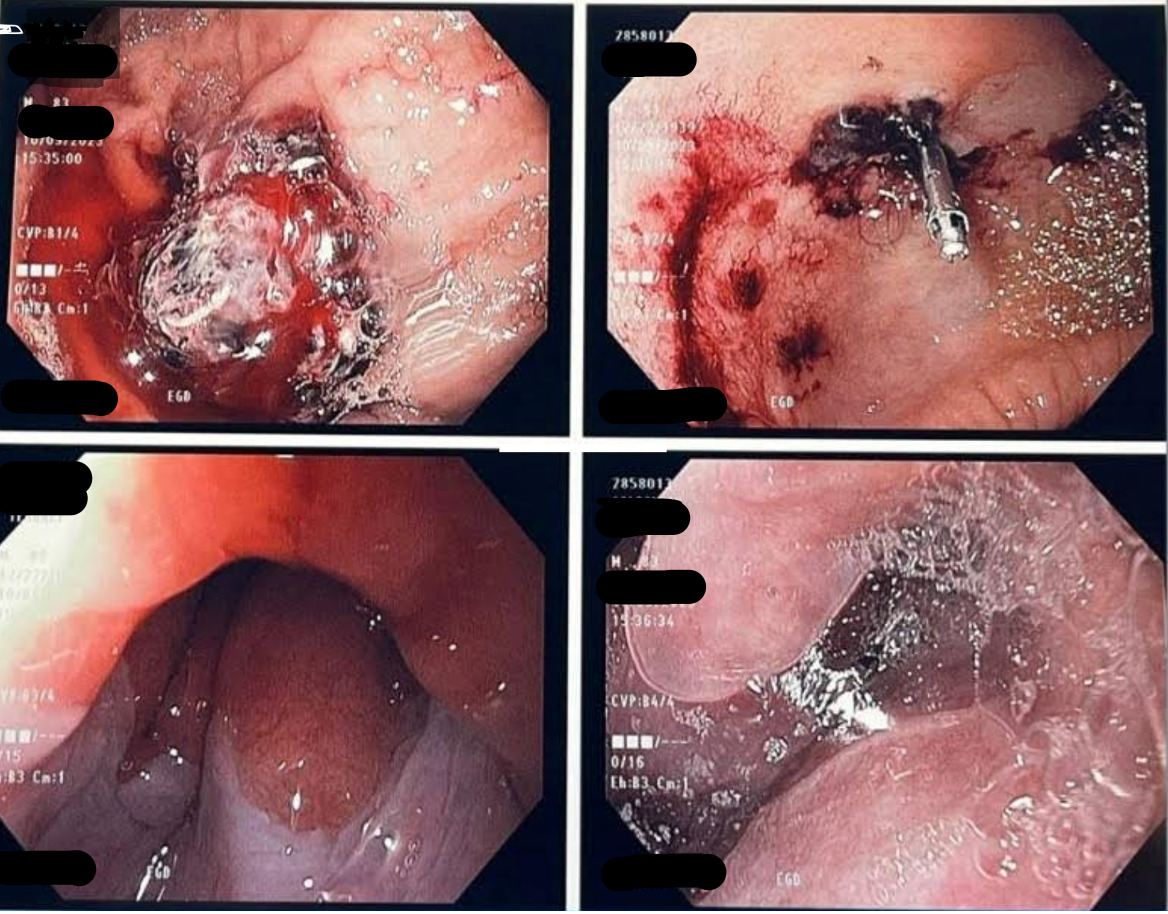
Figure: Figure 1: Repeat EGD revealed a 1 cm ulcerated mass in the gastric fundus with granulation tissue and a previously placed clip.
Disclosures:
Vatsal Khanna indicated no relevant financial relationships.
James Aldridge indicated no relevant financial relationships.
Mark DeVore indicated no relevant financial relationships.
Serge Sorser indicated no relevant financial relationships.
Vatsal Khanna, MD1, James Aldridge, MD2, Mark DeVore, MD1, Serge Sorser, MD1. P3094 - The Ulcer That Wasn't: Gastric Amyloidosis Masquerading as Refractory Upper Gastrointestinal Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Vatsal Khanna, MD1, James Aldridge, MD2, Mark DeVore, MD1, Serge Sorser, MD1
1Henry Ford Health, Southfield, MI; 2Corewell Health, Redford, MI
Introduction: Gastric involvement in systemic amyloidosis is a rare and often underdiagnosed cause of upper gastrointestinal (GI) bleeding. Clinical manifestations are nonspecific and may include early satiety, weight loss, or recurrent bleeding, often mimicking peptic ulcer disease or malignancy. Endoscopic findings are frequently subtle, and biopsies are sometimes deferred during active bleeding. We present a case of gastric amyloidosis identified after nearly a year of recurrent GI bleeding and repeated non-diagnostic endoscopies.
Case Description/
Methods: An 84-year-old man with low-grade myelodysplastic syndrome, stage V chronic kidney disease, coronary artery disease, and type 2 diabetes presented to our hospital with progressive weakness, orthostatic dizziness, and melena. He was on low-dose aspirin, denied NSAID use, and was not taking anticoagulants.
Over the past year, he had multiple hospitalizations for recurrent upper GI bleeding. Prior EGDs revealed large ulcers in the gastric fundus and antrum with adherent clots, treated with over-the-scope clips and epinephrine injection. Biopsies were deferred due to active bleeding and poor visualization.
On this admission, he was hemodynamically stable with melena on exam and a hemoglobin of 9.7 g/dL. IV pantoprazole was initiated. Given his recurrent bleeding with no clear etiology on prior evaluations, serum, and urine protein electrophoresis with immunofixation were performed to assess for possible plasma cell dyscrasia. Free light chain assay showed elevated kappa and lambda levels, with a kappa-to-lambda ratio of 2.43—within the renal-adjusted range.
Repeat EGD revealed a 1 cm ulcerated mass in the gastric fundus with granulation tissue and a previously placed clip. No active bleeding was noted (Figure 1). Biopsies showed chronic gastritis and ulceration. Congo red staining confirmed submucosal amyloid deposits with apple-green birefringence, diagnostic of gastric amyloidosis. The patient was discharged on oral pantoprazole twice daily with outpatient hematology-oncology follow-up for suspected AL amyloidosis.
Discussion: This case highlights the diagnostic challenge of gastric amyloidosis, particularly when biopsies are delayed due to acute bleeding. In patients with chronic kidney disease, free light chain ratios may be misleading. Deep biopsies with Congo red staining remain essential for diagnosis. Early recognition can prevent delays in initiating systemic therapy for AL amyloidosis.
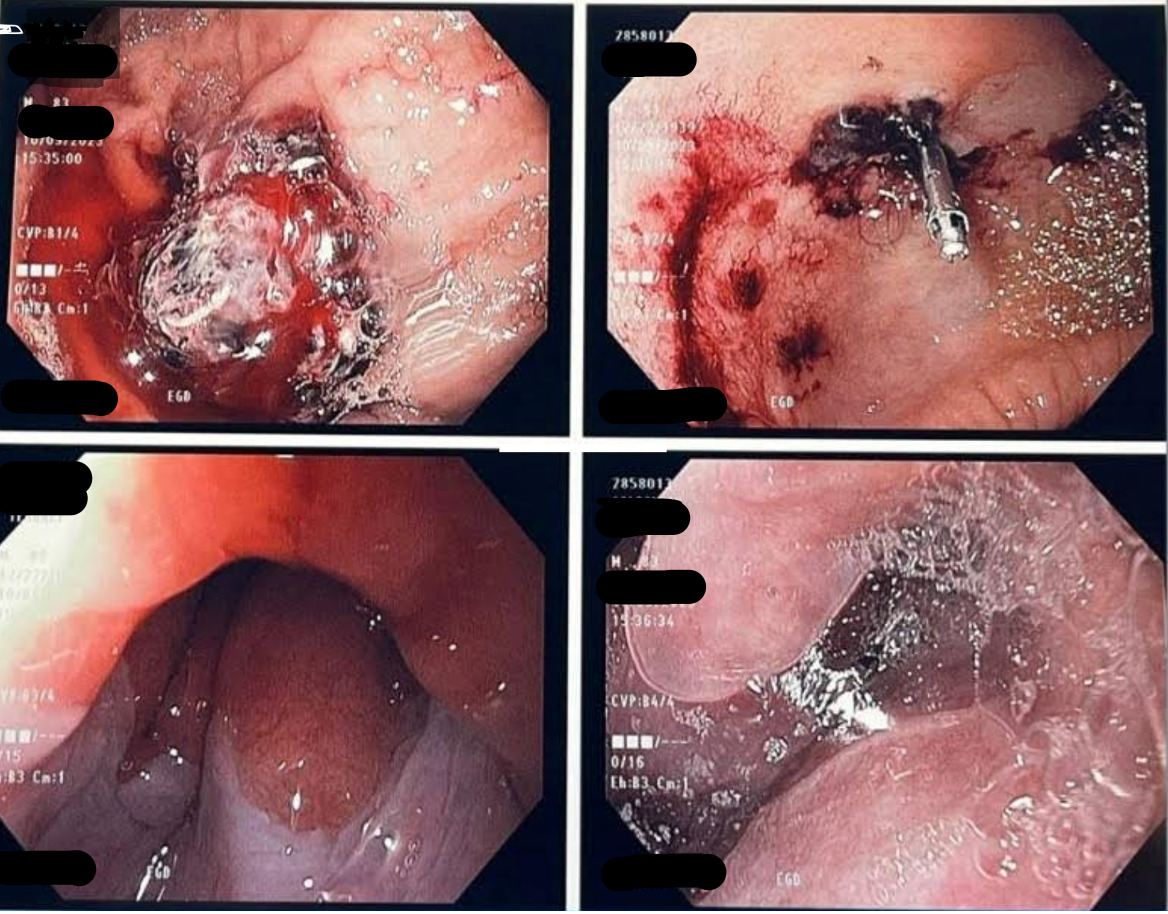
Figure: Figure 1: Repeat EGD revealed a 1 cm ulcerated mass in the gastric fundus with granulation tissue and a previously placed clip.
Disclosures:
Vatsal Khanna indicated no relevant financial relationships.
James Aldridge indicated no relevant financial relationships.
Mark DeVore indicated no relevant financial relationships.
Serge Sorser indicated no relevant financial relationships.
Vatsal Khanna, MD1, James Aldridge, MD2, Mark DeVore, MD1, Serge Sorser, MD1. P3094 - The Ulcer That Wasn't: Gastric Amyloidosis Masquerading as Refractory Upper Gastrointestinal Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.


