Monday Poster Session
Category: GI Bleeding
P3089 - Fatal Gastrointestinal Bleeding in a Case of Duodenal Squamous Cell Carcinoma and Subsequent Duodenorenal Fistula
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Amel Tabet Aoul, MD, PhD
HCA Healthcare Citrus Hospital
Hernando, FL
Presenting Author(s)
Amel Tabet Aoul, MD, PhD1, Nathaniel Leavitt, DO2, Ryan Cromwell, MD2, Melvin Joy, MD2, He Chen, MD2, Lakshmipathi Reddi, MD2, Joseph Maslak, MD2
1HCA Healthcare Citrus Hospital, Hernando, FL; 2HCA Healthcare Citrus Hospital, Inverness, FL
Introduction: Duodenorenal fistulas (DRF) are rare pathologies, mostly affecting the retroperitoneal aspect of the duodenum and emanating from chronic inflammation of the kidney. However, malignant etiologies have also been reported. On the other hand, primary or metastatic squamous cell carcinoma (SCC) of the small intestine (SI) are extremely rare, thus encountering a case of SI-SCC induced DRF is even more unprecedented.
Case Description/
Methods: A 62-year-old male with history of right ureterolithiasis and chronic hydronephrosis but no history of gastrointestinal issues, presented to emergency department with complaints of hematochezia for a month. On arrival, his hemoglobin (Hb) level was 5.1g/dL with a positive fecal occult blood test. The patient refused blood products due to religious beliefs and thus received isotonic fluids, intravenous pantoprazole, 40,000 units of epoetin alfa, 500 mg of iron dextran, cyanocobalamin, and folic acid. Gastroenterology was consulted and an esophagogastroduodenoscopy (EGD) was performed revealing a large duodenal cratered ulceration with rolled margins in the second portion of the duodenum not involving the ampulla of Vater, with deep fistulous tract distal to the superior duodenal angle (Figure 1). Computed tomography (CT) of the abdomen and pelvis with oral contrast showed a DRF with marked dilation of right renal pelvis and several air densities (Figure 2), an enterocaval fistula with a slow caval bleed was also suspected. Biopsy of the DRF demonstrated keratinized SCC. General surgery was consulted. Transfer to a facility with a higher level of care took place, however with low Hb level, blood transfusion restriction and the extensive nature of the intervention required, the surgery was contraindicated and palliative radiation was recommended. However, comfort measures only were elected by the patient's surrogate and patient expired shortly thereafter due to cardiac arrest.
Discussion: This is a unique SI pathology that led to the patient’s demise due to substantial gastrointestinal (GI) blood loss. The very few cases of DRF described in the literature manifested with urological symptoms, contrasted with GI bleeding and severe anemia observed our case. Management was mostly surgical but palliative treatments were sometimes considered for patients deemed poor surgical candidates as was the case for our patient. Thus, we hope this case adds to the scant documentation on this extremely uncommon form of SI cancer and the potential complications it may produce.
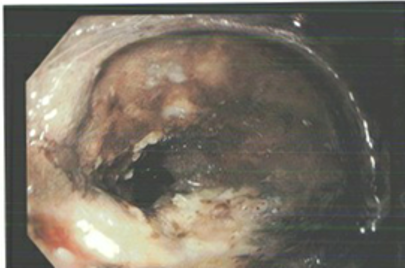
Figure: Figure 1: EGD image revealing a large duodenal ulcer with dark deep fistulous tract distal to the superior duodenal angle in the proximal second portion of the duodenum.
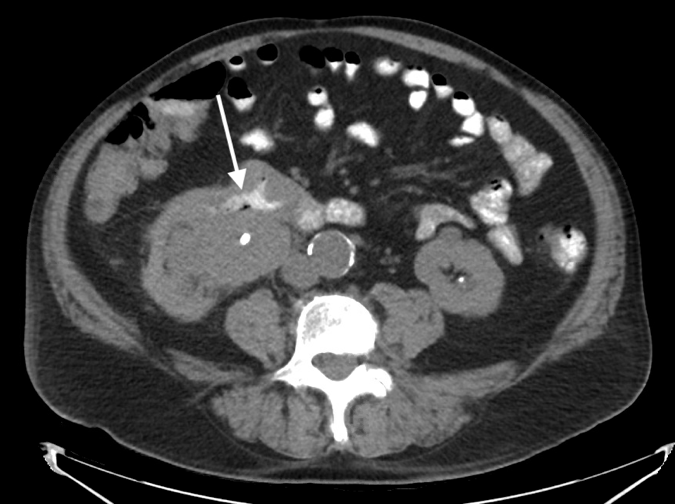
Figure: Figure 2: Computed tomography of the abdomen and pelvis with oral contrast demonstrating a fistulous connection with passage of intravenous contrast between the duodenum and the right renal pelvis (indicated by white arrow).
Disclosures:
Amel Tabet Aoul indicated no relevant financial relationships.
Nathaniel Leavitt indicated no relevant financial relationships.
Ryan Cromwell indicated no relevant financial relationships.
Melvin Joy indicated no relevant financial relationships.
He Chen indicated no relevant financial relationships.
Lakshmipathi Reddi indicated no relevant financial relationships.
Joseph Maslak indicated no relevant financial relationships.
Amel Tabet Aoul, MD, PhD1, Nathaniel Leavitt, DO2, Ryan Cromwell, MD2, Melvin Joy, MD2, He Chen, MD2, Lakshmipathi Reddi, MD2, Joseph Maslak, MD2. P3089 - Fatal Gastrointestinal Bleeding in a Case of Duodenal Squamous Cell Carcinoma and Subsequent Duodenorenal Fistula, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1HCA Healthcare Citrus Hospital, Hernando, FL; 2HCA Healthcare Citrus Hospital, Inverness, FL
Introduction: Duodenorenal fistulas (DRF) are rare pathologies, mostly affecting the retroperitoneal aspect of the duodenum and emanating from chronic inflammation of the kidney. However, malignant etiologies have also been reported. On the other hand, primary or metastatic squamous cell carcinoma (SCC) of the small intestine (SI) are extremely rare, thus encountering a case of SI-SCC induced DRF is even more unprecedented.
Case Description/
Methods: A 62-year-old male with history of right ureterolithiasis and chronic hydronephrosis but no history of gastrointestinal issues, presented to emergency department with complaints of hematochezia for a month. On arrival, his hemoglobin (Hb) level was 5.1g/dL with a positive fecal occult blood test. The patient refused blood products due to religious beliefs and thus received isotonic fluids, intravenous pantoprazole, 40,000 units of epoetin alfa, 500 mg of iron dextran, cyanocobalamin, and folic acid. Gastroenterology was consulted and an esophagogastroduodenoscopy (EGD) was performed revealing a large duodenal cratered ulceration with rolled margins in the second portion of the duodenum not involving the ampulla of Vater, with deep fistulous tract distal to the superior duodenal angle (Figure 1). Computed tomography (CT) of the abdomen and pelvis with oral contrast showed a DRF with marked dilation of right renal pelvis and several air densities (Figure 2), an enterocaval fistula with a slow caval bleed was also suspected. Biopsy of the DRF demonstrated keratinized SCC. General surgery was consulted. Transfer to a facility with a higher level of care took place, however with low Hb level, blood transfusion restriction and the extensive nature of the intervention required, the surgery was contraindicated and palliative radiation was recommended. However, comfort measures only were elected by the patient's surrogate and patient expired shortly thereafter due to cardiac arrest.
Discussion: This is a unique SI pathology that led to the patient’s demise due to substantial gastrointestinal (GI) blood loss. The very few cases of DRF described in the literature manifested with urological symptoms, contrasted with GI bleeding and severe anemia observed our case. Management was mostly surgical but palliative treatments were sometimes considered for patients deemed poor surgical candidates as was the case for our patient. Thus, we hope this case adds to the scant documentation on this extremely uncommon form of SI cancer and the potential complications it may produce.
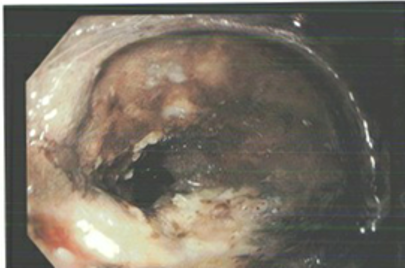
Figure: Figure 1: EGD image revealing a large duodenal ulcer with dark deep fistulous tract distal to the superior duodenal angle in the proximal second portion of the duodenum.
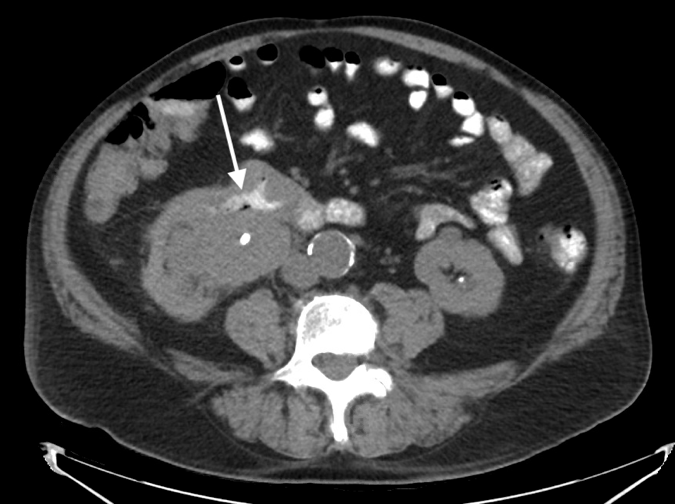
Figure: Figure 2: Computed tomography of the abdomen and pelvis with oral contrast demonstrating a fistulous connection with passage of intravenous contrast between the duodenum and the right renal pelvis (indicated by white arrow).
Disclosures:
Amel Tabet Aoul indicated no relevant financial relationships.
Nathaniel Leavitt indicated no relevant financial relationships.
Ryan Cromwell indicated no relevant financial relationships.
Melvin Joy indicated no relevant financial relationships.
He Chen indicated no relevant financial relationships.
Lakshmipathi Reddi indicated no relevant financial relationships.
Joseph Maslak indicated no relevant financial relationships.
Amel Tabet Aoul, MD, PhD1, Nathaniel Leavitt, DO2, Ryan Cromwell, MD2, Melvin Joy, MD2, He Chen, MD2, Lakshmipathi Reddi, MD2, Joseph Maslak, MD2. P3089 - Fatal Gastrointestinal Bleeding in a Case of Duodenal Squamous Cell Carcinoma and Subsequent Duodenorenal Fistula, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
