Monday Poster Session
Category: GI Bleeding
P3087 - Infiltrating Presacral Neuroendocrine Tumor: An Atypical Cause of Lower Gastrointestinal Bleeding
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Laura Krause, DO
Eisenhower Army Medical Center
Augusta, GA
Presenting Author(s)
Laura Krause, DO, Ross Humes, MD
Eisenhower Army Medical Center, Augusta, GA
Introduction: Neuroendocrine tumors (NETs) are rare malignancies with an incidence of 8.19 per 100,000 people. Typical patterns demonstrate NETs tend to be asymptomatic until advanced stages and frequently identified within the GI system. The presacrum is an exceedingly rare location for primary and metastatic NETs, that, when symptomatic, present with pelvic pain or fullness. We describe the case of an 82 year old African American male with a metastatic presacral NET presenting with lower GI bleeding.
Case Description/
Methods: The patient had a history of a 10mm, well-differentiated, G2 rectal NET with Ki67 index less than 5% located 8cm from the anal verge, which was treated with complete endoscopic resection 15 years prior to presentation. There was one recurrence of local disease, also treated with complete endoscopic resection 10 years prior. Metastases to bone and liver were identified on imaging 4 years prior, and the presacrum 2 years prior. The metastatic disease was treated with systemic chemotherapy, but this was stopped 4 months prior to current presentation. On admission, hemoglobin was 11.0 g/dL which decreased to 6.4 g/dL the following day. He was given 3 units of packed red blood cells. Colonoscopy identified a large clot adherent to pale, dusky, necrotic appearing rectal mucosa. There were 3 fistulous tracts identified. The mucosa proximal to 8cm from the anal verge appeared normal. CT angiography of the abdomen and pelvis demonstrated a large presacral, contrast-enhancing tumor filling the majority of the pelvis with cystic and necrotic changes. The tumor was contiguous with the rectum, without differentiation between the structures and with connecting fistulous tracts. There was no evidence of mass within the rectum on colonoscopy or imaging.
Discussion: The prognosis of NETs can be difficult to predict. The majority of rectal NETs are less than 1cm and do not invade deeper than the submucosa, making them amenable to endoscopic resection. The risk of metastatic disease is low at 5% for lesions less than 1cm. In this case, the patient had complete endoscopic resection with negative margins, but intermediate grading based on Ki67 index. On review of the literature, we have not identified any reported cases of metastatic presacral lesions eroding into the rectum or presenting with lower GI bleeding. Interestingly, it appears that the location of erosion from the presacral tumor is he same location as the index tumor. This case highlights a rare presentation of a rare disease.
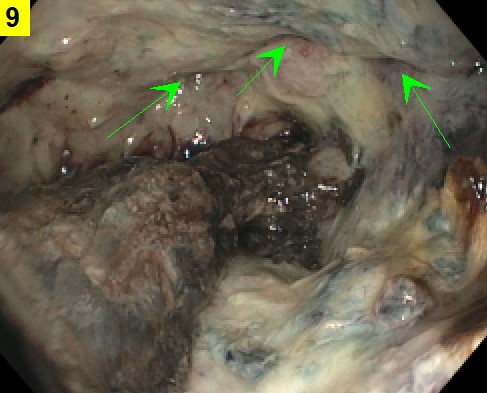
Figure: Colonoscopy, at 8cm proximal from rectum. Diffusely necrotic rectal mucosa with multiple fistulas (green arrows). The area of prior cauterization has an adherent clot. There is no evidence of mass within the rectum.

Figure: Computed tomography angiogram of abdomen/pelvis, sagittal view. Large contrast-enhancing presacral tumor with internal cystic/necrotic changes that is growing into and indistinguishable from rectum. There is a channel-like area consistent with fistula formation. The tumor is exerting mass effect on other pelvic organs.
Disclosures:
Laura Krause indicated no relevant financial relationships.
Ross Humes indicated no relevant financial relationships.
Laura Krause, DO, Ross Humes, MD. P3087 - Infiltrating Presacral Neuroendocrine Tumor: An Atypical Cause of Lower Gastrointestinal Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Eisenhower Army Medical Center, Augusta, GA
Introduction: Neuroendocrine tumors (NETs) are rare malignancies with an incidence of 8.19 per 100,000 people. Typical patterns demonstrate NETs tend to be asymptomatic until advanced stages and frequently identified within the GI system. The presacrum is an exceedingly rare location for primary and metastatic NETs, that, when symptomatic, present with pelvic pain or fullness. We describe the case of an 82 year old African American male with a metastatic presacral NET presenting with lower GI bleeding.
Case Description/
Methods: The patient had a history of a 10mm, well-differentiated, G2 rectal NET with Ki67 index less than 5% located 8cm from the anal verge, which was treated with complete endoscopic resection 15 years prior to presentation. There was one recurrence of local disease, also treated with complete endoscopic resection 10 years prior. Metastases to bone and liver were identified on imaging 4 years prior, and the presacrum 2 years prior. The metastatic disease was treated with systemic chemotherapy, but this was stopped 4 months prior to current presentation. On admission, hemoglobin was 11.0 g/dL which decreased to 6.4 g/dL the following day. He was given 3 units of packed red blood cells. Colonoscopy identified a large clot adherent to pale, dusky, necrotic appearing rectal mucosa. There were 3 fistulous tracts identified. The mucosa proximal to 8cm from the anal verge appeared normal. CT angiography of the abdomen and pelvis demonstrated a large presacral, contrast-enhancing tumor filling the majority of the pelvis with cystic and necrotic changes. The tumor was contiguous with the rectum, without differentiation between the structures and with connecting fistulous tracts. There was no evidence of mass within the rectum on colonoscopy or imaging.
Discussion: The prognosis of NETs can be difficult to predict. The majority of rectal NETs are less than 1cm and do not invade deeper than the submucosa, making them amenable to endoscopic resection. The risk of metastatic disease is low at 5% for lesions less than 1cm. In this case, the patient had complete endoscopic resection with negative margins, but intermediate grading based on Ki67 index. On review of the literature, we have not identified any reported cases of metastatic presacral lesions eroding into the rectum or presenting with lower GI bleeding. Interestingly, it appears that the location of erosion from the presacral tumor is he same location as the index tumor. This case highlights a rare presentation of a rare disease.
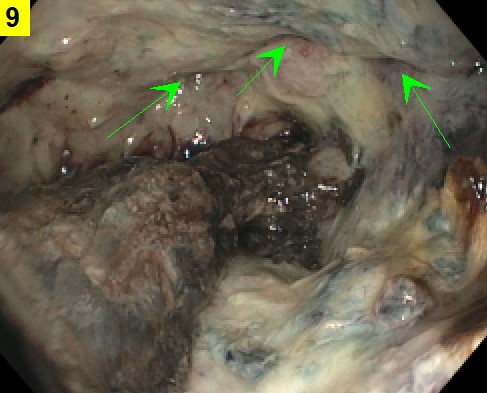
Figure: Colonoscopy, at 8cm proximal from rectum. Diffusely necrotic rectal mucosa with multiple fistulas (green arrows). The area of prior cauterization has an adherent clot. There is no evidence of mass within the rectum.

Figure: Computed tomography angiogram of abdomen/pelvis, sagittal view. Large contrast-enhancing presacral tumor with internal cystic/necrotic changes that is growing into and indistinguishable from rectum. There is a channel-like area consistent with fistula formation. The tumor is exerting mass effect on other pelvic organs.
Disclosures:
Laura Krause indicated no relevant financial relationships.
Ross Humes indicated no relevant financial relationships.
Laura Krause, DO, Ross Humes, MD. P3087 - Infiltrating Presacral Neuroendocrine Tumor: An Atypical Cause of Lower Gastrointestinal Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

