Monday Poster Session
Category: GI Bleeding
P3085 - Recurrent GI Bleeds in the Setting of Heyde Syndrome: The Importance of Early Diagnosis and Management
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- SW
Syed Waseem
Temple University
Philadelphia, PA
Presenting Author(s)
Syed Waseem, , Shivani Kumar, MD, Claire Raab, MD
Temple University, Philadelphia, PA
Introduction: Heyde syndrome (HS) is characterized by the triad of severe aortic stenosis, acquired type 2 von Willebrand Factor (vWF) deficiency, and gastrointestinal (GI) bleeding. Aortic valve (AV) replacement leads to cessation of GI bleeding in 95% of reported cases thus highlighting the need for early diagnosis to prevent life-threatening complications.
Case Description/
Methods: A 74-year-old woman presented to the ED after 3 days of melena, worsening shortness of breath, and severe angina. Her medical history included aortic stenosis (AS), hypertension, hyperlipidemia, and iron deficiency anemia with no NSAID use. Initial exam revealed a loud murmur at the left sternal border and bilateral lower extremity 2+ pitting edema. Admission labs revealed a Hgb of 5.3, Hct of 18.4, and a WBC of 6.6. ECG was unremarkable for acute ischemic changes. She was admitted for management of presumed GI bleed and received 2 units of packed red blood cells.
The patient presented three times in the previous seven months with similar complaints of melena, chest pain and severe Hgb drop, with no obvious source despite extensive evaluations. Six months prior to admission, she was found to have cecal angioectasias without obvious bleeding. She was admitted one week prior to admission, but no bleeding source was identified.
A push enteroscopy revealed four angioectasias in the duodenum and jejunum, treated with argon plasma coagulation (APC). Echocardiogram was ordered and revealed an AV peak velocity of 4.40 m/s, an AV mean gradient of 51.88 mmHg, and an AV area of 0.84 cm2, thereby classifying her aortic stenosis as severe. vWF labs showed a subtle relative decrease of the high molecular weight vWF multimers, indicating an acquired vWF deficiency. With the triad of HS met, the patient was referred for a transcatheter aortic valve replacement (TAVR) and now remains stable.
Discussion: HS has a 1-3% incidence rate in patients with AS; however, it may not be considered in patients with recurrent GI bleeds and AS. Delays in diagnosis have been shown to increase mortality risk and hospital admissions. Treatment of bleeding with APC in HS has been associated with a higher recurrent rate of bleeding, while timely AV replacement has been shown to rapidly lead to GI bleeding cessation. This patient's varied findings on GI interventions and subtle reduction in the vWF multimer assay underscore the difficulty of diagnosing HS. Increasing awareness of HS will enable earlier diagnosis and prevent severe complications.
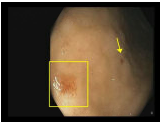
Figure: An angioectasia visualized in the duodenal bulb on push enteroscopy.
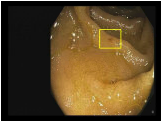
Figure: An angioectasia visualized in the jejunum on push enteroscopy.
Disclosures:
Syed Waseem indicated no relevant financial relationships.
Shivani Kumar indicated no relevant financial relationships.
Claire Raab indicated no relevant financial relationships.
Syed Waseem, , Shivani Kumar, MD, Claire Raab, MD. P3085 - Recurrent GI Bleeds in the Setting of Heyde Syndrome: The Importance of Early Diagnosis and Management, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Temple University, Philadelphia, PA
Introduction: Heyde syndrome (HS) is characterized by the triad of severe aortic stenosis, acquired type 2 von Willebrand Factor (vWF) deficiency, and gastrointestinal (GI) bleeding. Aortic valve (AV) replacement leads to cessation of GI bleeding in 95% of reported cases thus highlighting the need for early diagnosis to prevent life-threatening complications.
Case Description/
Methods: A 74-year-old woman presented to the ED after 3 days of melena, worsening shortness of breath, and severe angina. Her medical history included aortic stenosis (AS), hypertension, hyperlipidemia, and iron deficiency anemia with no NSAID use. Initial exam revealed a loud murmur at the left sternal border and bilateral lower extremity 2+ pitting edema. Admission labs revealed a Hgb of 5.3, Hct of 18.4, and a WBC of 6.6. ECG was unremarkable for acute ischemic changes. She was admitted for management of presumed GI bleed and received 2 units of packed red blood cells.
The patient presented three times in the previous seven months with similar complaints of melena, chest pain and severe Hgb drop, with no obvious source despite extensive evaluations. Six months prior to admission, she was found to have cecal angioectasias without obvious bleeding. She was admitted one week prior to admission, but no bleeding source was identified.
A push enteroscopy revealed four angioectasias in the duodenum and jejunum, treated with argon plasma coagulation (APC). Echocardiogram was ordered and revealed an AV peak velocity of 4.40 m/s, an AV mean gradient of 51.88 mmHg, and an AV area of 0.84 cm2, thereby classifying her aortic stenosis as severe. vWF labs showed a subtle relative decrease of the high molecular weight vWF multimers, indicating an acquired vWF deficiency. With the triad of HS met, the patient was referred for a transcatheter aortic valve replacement (TAVR) and now remains stable.
Discussion: HS has a 1-3% incidence rate in patients with AS; however, it may not be considered in patients with recurrent GI bleeds and AS. Delays in diagnosis have been shown to increase mortality risk and hospital admissions. Treatment of bleeding with APC in HS has been associated with a higher recurrent rate of bleeding, while timely AV replacement has been shown to rapidly lead to GI bleeding cessation. This patient's varied findings on GI interventions and subtle reduction in the vWF multimer assay underscore the difficulty of diagnosing HS. Increasing awareness of HS will enable earlier diagnosis and prevent severe complications.
Figure: An angioectasia visualized in the duodenal bulb on push enteroscopy.
Figure: An angioectasia visualized in the jejunum on push enteroscopy.
Disclosures:
Syed Waseem indicated no relevant financial relationships.
Shivani Kumar indicated no relevant financial relationships.
Claire Raab indicated no relevant financial relationships.
Syed Waseem, , Shivani Kumar, MD, Claire Raab, MD. P3085 - Recurrent GI Bleeds in the Setting of Heyde Syndrome: The Importance of Early Diagnosis and Management, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
