Monday Poster Session
Category: GI Bleeding
P3084 - Hematochezia as the Initial Presentation of Amyloidosis: A Rare Presenting Symptom
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Patt Panuncillon, DO
Ochsner Health Clinic Foundation, TX
Presenting Author(s)
Patt Panuncillon, DO1, Ricardo David Espinosa, MD2, Joanna Yuen, DO, MA2, Ian Tobal, DO2, Ashley Scholtens, MD2, Koshy George, MD2
1Ochsner Health Clinic Foundation, Pearland, TX; 2Ochsner Health Clinic Foundation, New Orleans, LA
Introduction: Amyloidosis is a rare phenomenon and can be challenging to diagnose. It can manifest itself in several ways due to the deposition of different precursor proteins in various organs and is usually seen in conditions that produce monoclonal immunoglobulins or persistent uncontrolled inflammatory disease. Amyloidosis of the colon is particularly rare and if not treated could lead to hematochezia and potential hemodynamic collapse.
Case Description/
Methods: 52-year-old male with atrial fibrillation on apixaban, nonischemic cardiomyopathy, and spindle cell neoplasm presented to the ED with complaints of hematochezia and melena. Initial labs showed Hgb of 6.8 g/dL and was transfused 1 unit of pRBC. Colonoscopy with biopsy performed and showed a 6 mm polyp in the cecum, multiple ulcers in the ascending and transverse colon, as well as friability with contact bleeding from descending to ascending colon. Patient was then subsequently discharged with referrals to Gastroenterology and Hematology as well as pantoprazole. During follow up visits, colon ulcer biopsies returned positive for amyloid by Congo Red staining. Furthermore, bone marrow biopsy showed 45% plasma cells and PET scan showed widespread uptakes, strengthening the diagnosis. Patient was started on induction therapy with Dara-CyBorD and IV iron infusion. Subsequently, the patient has had decreased bloody stools but reports abdominal cramping, loose bowel movements, and fatigue. Most recently, patient is being closely followed by Hematology for treatment and symptomatic relief.
Discussion: Amyloidosis is rare and can lead to ulcer in the colon and subsequent hematochezia. On endoscopy, it typically presents with ulcers, submucosal petechial hematomas, and polypoid lesions. Amyloidosis is challenging to diagnose because of different precursor proteins leading to diverse clinical manifestations making it difficult to find a consistent pattern. In this case, the diagnosis was confirmed by colon biopsy Congo Red staining and supported by bone marrow biopsy and PET scan. This case shows the importance of recognizing hematochezia as a presenting symptom of Amyloidosis and emphasizes the importance of keeping Amyloidosis on the differential when encountered with a GI bleed. Management of Colonic Amyloidosis is focused mainly on symptomatic relief, addressing gastrointestinal bleeding through endoscopic intervention, and implementing targeted treatment based on specific amyloidosis type preventing further complications.
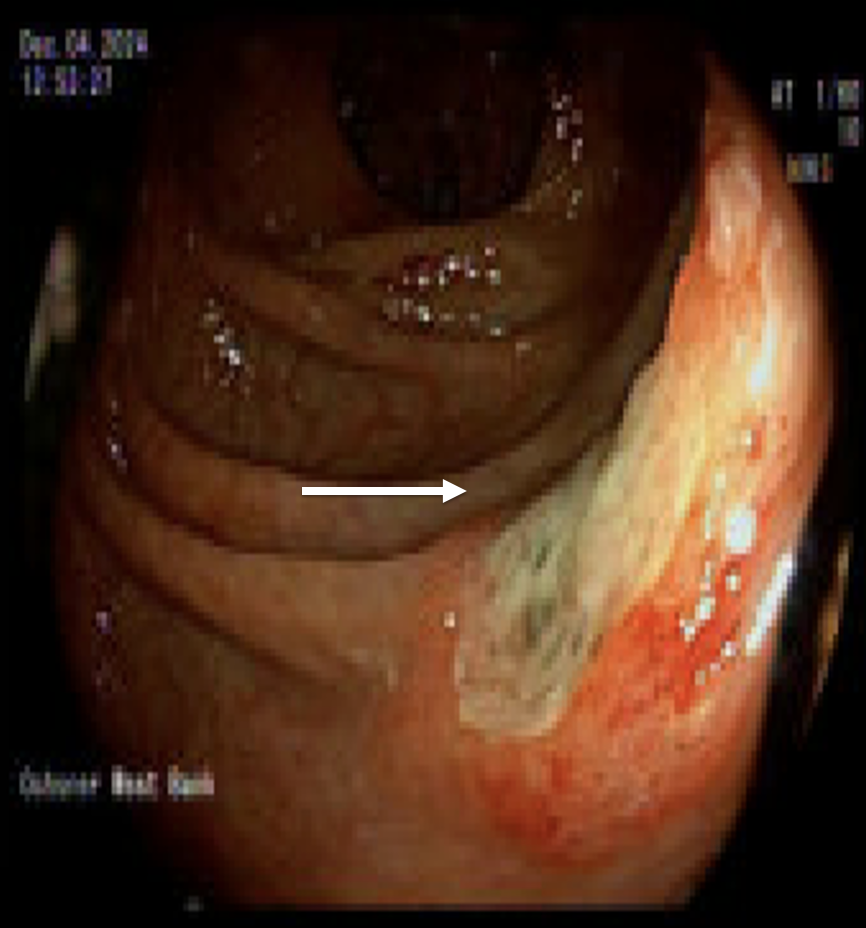
Figure: Figure 1: Ulcer in ascending colon
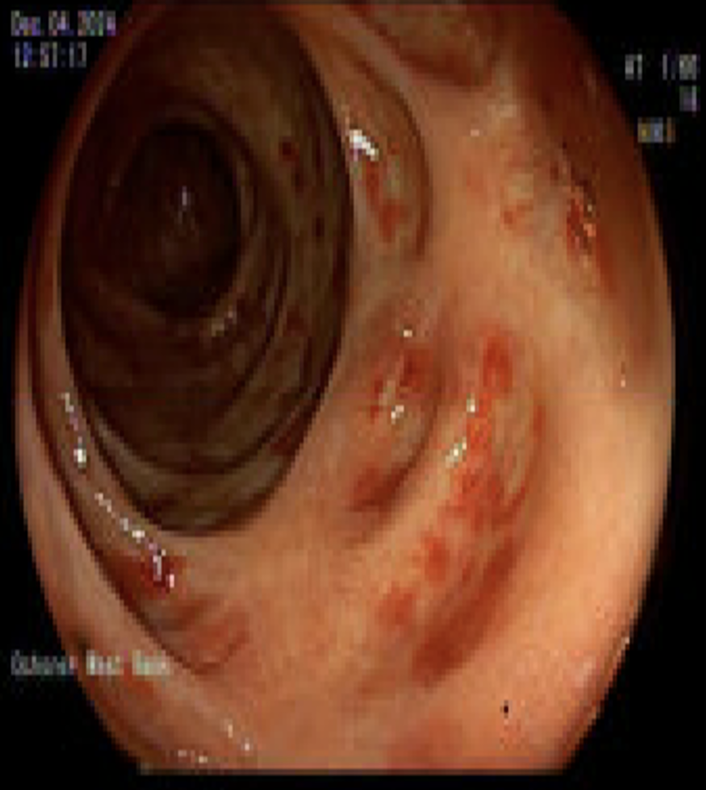
Figure: Figure 2: Friable mucosa in transverse colon
Disclosures:
Patt Panuncillon indicated no relevant financial relationships.
Ricardo David Espinosa indicated no relevant financial relationships.
Joanna Yuen indicated no relevant financial relationships.
Ian Tobal indicated no relevant financial relationships.
Ashley Scholtens indicated no relevant financial relationships.
Koshy George indicated no relevant financial relationships.
Patt Panuncillon, DO1, Ricardo David Espinosa, MD2, Joanna Yuen, DO, MA2, Ian Tobal, DO2, Ashley Scholtens, MD2, Koshy George, MD2. P3084 - Hematochezia as the Initial Presentation of Amyloidosis: A Rare Presenting Symptom, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Ochsner Health Clinic Foundation, Pearland, TX; 2Ochsner Health Clinic Foundation, New Orleans, LA
Introduction: Amyloidosis is a rare phenomenon and can be challenging to diagnose. It can manifest itself in several ways due to the deposition of different precursor proteins in various organs and is usually seen in conditions that produce monoclonal immunoglobulins or persistent uncontrolled inflammatory disease. Amyloidosis of the colon is particularly rare and if not treated could lead to hematochezia and potential hemodynamic collapse.
Case Description/
Methods: 52-year-old male with atrial fibrillation on apixaban, nonischemic cardiomyopathy, and spindle cell neoplasm presented to the ED with complaints of hematochezia and melena. Initial labs showed Hgb of 6.8 g/dL and was transfused 1 unit of pRBC. Colonoscopy with biopsy performed and showed a 6 mm polyp in the cecum, multiple ulcers in the ascending and transverse colon, as well as friability with contact bleeding from descending to ascending colon. Patient was then subsequently discharged with referrals to Gastroenterology and Hematology as well as pantoprazole. During follow up visits, colon ulcer biopsies returned positive for amyloid by Congo Red staining. Furthermore, bone marrow biopsy showed 45% plasma cells and PET scan showed widespread uptakes, strengthening the diagnosis. Patient was started on induction therapy with Dara-CyBorD and IV iron infusion. Subsequently, the patient has had decreased bloody stools but reports abdominal cramping, loose bowel movements, and fatigue. Most recently, patient is being closely followed by Hematology for treatment and symptomatic relief.
Discussion: Amyloidosis is rare and can lead to ulcer in the colon and subsequent hematochezia. On endoscopy, it typically presents with ulcers, submucosal petechial hematomas, and polypoid lesions. Amyloidosis is challenging to diagnose because of different precursor proteins leading to diverse clinical manifestations making it difficult to find a consistent pattern. In this case, the diagnosis was confirmed by colon biopsy Congo Red staining and supported by bone marrow biopsy and PET scan. This case shows the importance of recognizing hematochezia as a presenting symptom of Amyloidosis and emphasizes the importance of keeping Amyloidosis on the differential when encountered with a GI bleed. Management of Colonic Amyloidosis is focused mainly on symptomatic relief, addressing gastrointestinal bleeding through endoscopic intervention, and implementing targeted treatment based on specific amyloidosis type preventing further complications.
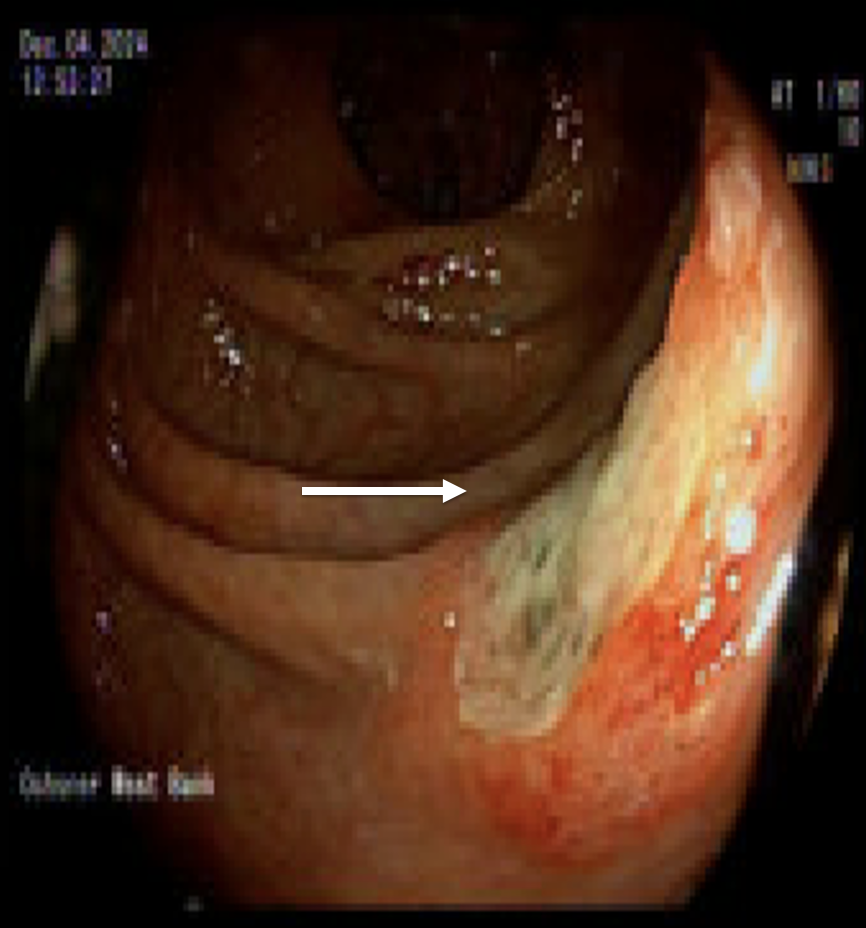
Figure: Figure 1: Ulcer in ascending colon
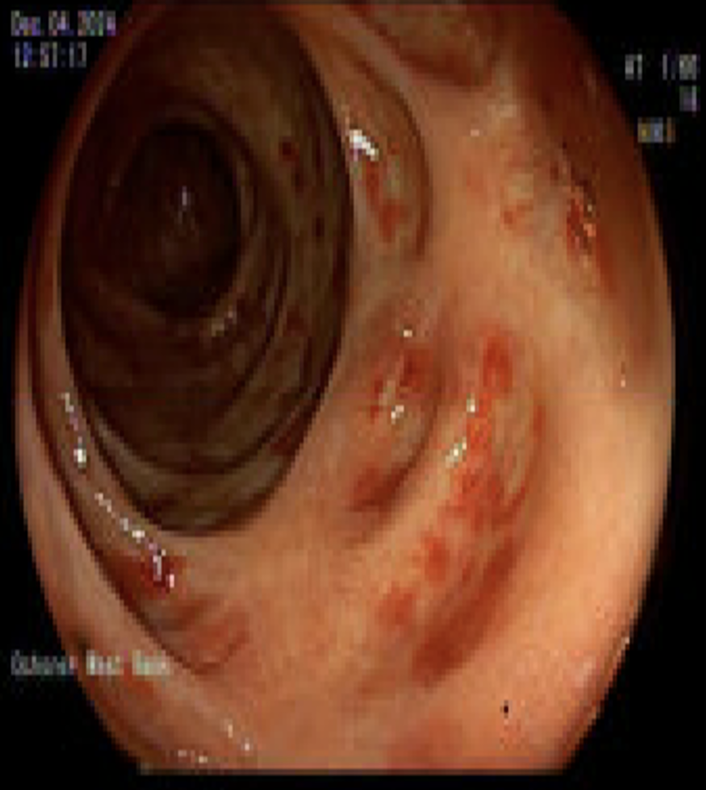
Figure: Figure 2: Friable mucosa in transverse colon
Disclosures:
Patt Panuncillon indicated no relevant financial relationships.
Ricardo David Espinosa indicated no relevant financial relationships.
Joanna Yuen indicated no relevant financial relationships.
Ian Tobal indicated no relevant financial relationships.
Ashley Scholtens indicated no relevant financial relationships.
Koshy George indicated no relevant financial relationships.
Patt Panuncillon, DO1, Ricardo David Espinosa, MD2, Joanna Yuen, DO, MA2, Ian Tobal, DO2, Ashley Scholtens, MD2, Koshy George, MD2. P3084 - Hematochezia as the Initial Presentation of Amyloidosis: A Rare Presenting Symptom, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
