Monday Poster Session
Category: GI Bleeding
P3074 - Outcomes of Lower Gastrointestinal Bleeding at Teaching vs Non-Teaching Hospitals: A Nationwide Inpatient Sample Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- JL
James Lee, MD
Stony Brook Medicine
Stony Brook, NY
Presenting Author(s)
James Lee, MD1, Rahul Tripathi, MD1, Alan Abboud, MD1, Matthew Obusan, BS2, Lisa Fisher, MD3, Daniel Jamorabo, MD4
1Stony Brook Medicine, Stony Brook, NY; 2Renaissance School of Medicine, Stony Brook University, Stony Brook, NY; 3Stony Brook University Hospital, Northport, NY; 4Northwell Health, Forest Hills, NY
Introduction: Lower gastrointestinal bleeding (LGIB) is a common and potentially serious cause of hospitalization, often requiring endoscopic or radiologic intervention. Outcomes may vary by hospital type, with teaching hospitals typically managing more complex cases. However, the impact of teaching status on LGIB outcomes remains unclear. Understanding these differences is essential to improving care delivery and reducing outcome disparities.
Methods: We performed a retrospective cohort study using the 2018–2020 Nationwide Inpatient Sample (NIS) to identify adult hospitalizations for LGIB. Hospitals were classified as teaching (urban teaching) or non-teaching (urban non-teaching and rural). Survey-weighted multivariable regression adjusted for demographics, comorbidities, and hospital characteristics. Primary outcomes were in-hospital mortality, length of stay (LOS), and total charges. Secondary outcomes included colonoscopy, early colonoscopy (≤1 day), angiography, embolization, and transfusion.
Results: Among an estimated 501,120 weighted LGIB admissions, 72.3% occurred at teaching hospitals. Compared to non-teaching hospitals, teaching hospitals had more non-White patients, higher comorbidity burden (Charlson index >3), and greater Medicaid enrollment. Overall, in-hospital mortality was 0.94%, and significantly higher at teaching hospitals (0.99%) than non-teaching (0.82%, p=0.013). After adjustment, teaching hospital admission was associated with 25% increased odds of mortality (aOR 1.25, 95% CI: 1.07–1.47, p=0.006), longer LOS (+0.56 days, p< 0.001), and higher total hospital charges (+$6,399, p< 0.001). Teaching hospitals had higher adjusted odds of colonoscopy, angiography, and embolization. Early colonoscopy rates did not differ (Table 2).
Discussion: In this nationally representative analysis of LGIB hospitalizations, admission to teaching hospitals was associated with higher in-hospital mortality, prolonged LOS, and increased healthcare costs, likely due to more frequent use of diagnostic and therapeutic procedures. These differences may reflect the referral of more complex or acutely ill patients to teaching centers. The lack of difference in early colonoscopy rates suggests that factors beyond timing of intervention may contribute to outcome disparities. Further investigation is warranted to better understand the role of hospital-level factors in shaping LGIB outcomes and to identify opportunities for improving care across all hospital settings.
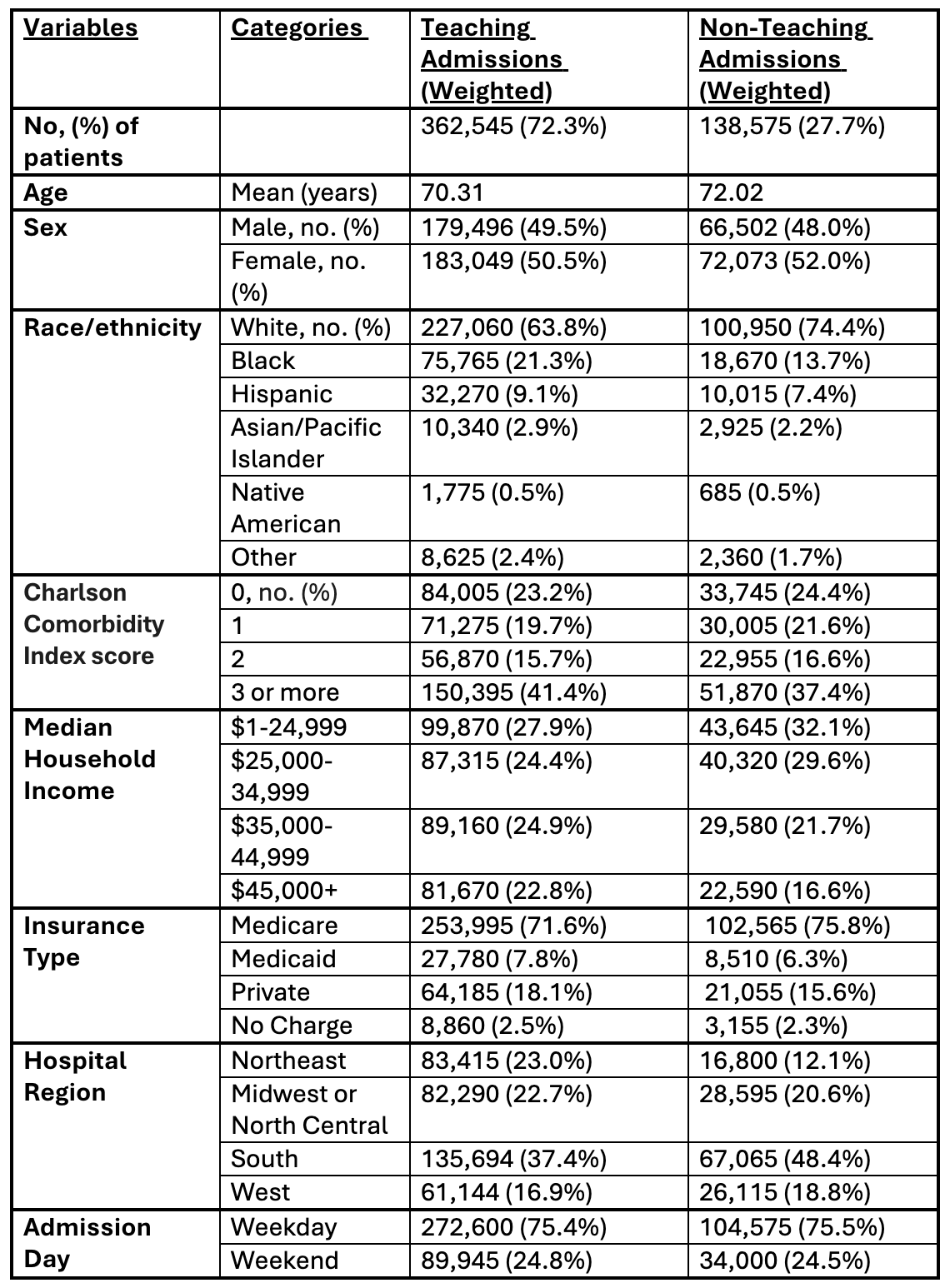
Figure: Table 1. Baseline Characteristics
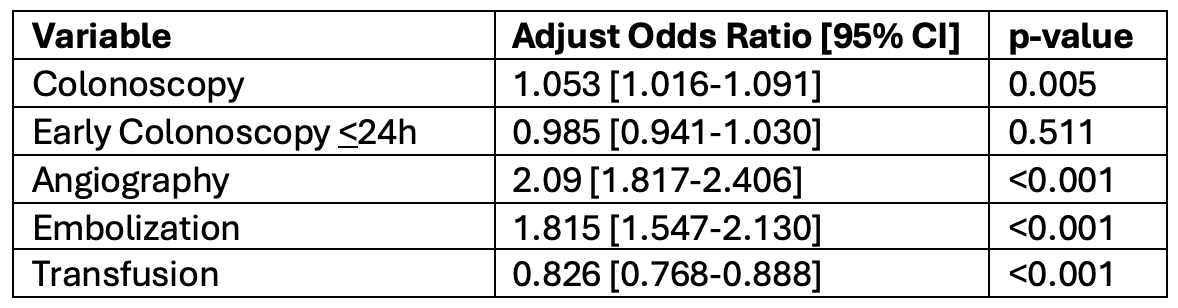
Figure: Table 2. Adjusted Odds of Interventions in LGIB Admissions: Teaching vs. Non-Teaching Hospitals
Disclosures:
James Lee indicated no relevant financial relationships.
Rahul Tripathi indicated no relevant financial relationships.
Alan Abboud indicated no relevant financial relationships.
Matthew Obusan indicated no relevant financial relationships.
Lisa Fisher indicated no relevant financial relationships.
Daniel Jamorabo indicated no relevant financial relationships.
James Lee, MD1, Rahul Tripathi, MD1, Alan Abboud, MD1, Matthew Obusan, BS2, Lisa Fisher, MD3, Daniel Jamorabo, MD4. P3074 - Outcomes of Lower Gastrointestinal Bleeding at Teaching vs Non-Teaching Hospitals: A Nationwide Inpatient Sample Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Stony Brook Medicine, Stony Brook, NY; 2Renaissance School of Medicine, Stony Brook University, Stony Brook, NY; 3Stony Brook University Hospital, Northport, NY; 4Northwell Health, Forest Hills, NY
Introduction: Lower gastrointestinal bleeding (LGIB) is a common and potentially serious cause of hospitalization, often requiring endoscopic or radiologic intervention. Outcomes may vary by hospital type, with teaching hospitals typically managing more complex cases. However, the impact of teaching status on LGIB outcomes remains unclear. Understanding these differences is essential to improving care delivery and reducing outcome disparities.
Methods: We performed a retrospective cohort study using the 2018–2020 Nationwide Inpatient Sample (NIS) to identify adult hospitalizations for LGIB. Hospitals were classified as teaching (urban teaching) or non-teaching (urban non-teaching and rural). Survey-weighted multivariable regression adjusted for demographics, comorbidities, and hospital characteristics. Primary outcomes were in-hospital mortality, length of stay (LOS), and total charges. Secondary outcomes included colonoscopy, early colonoscopy (≤1 day), angiography, embolization, and transfusion.
Results: Among an estimated 501,120 weighted LGIB admissions, 72.3% occurred at teaching hospitals. Compared to non-teaching hospitals, teaching hospitals had more non-White patients, higher comorbidity burden (Charlson index >3), and greater Medicaid enrollment. Overall, in-hospital mortality was 0.94%, and significantly higher at teaching hospitals (0.99%) than non-teaching (0.82%, p=0.013). After adjustment, teaching hospital admission was associated with 25% increased odds of mortality (aOR 1.25, 95% CI: 1.07–1.47, p=0.006), longer LOS (+0.56 days, p< 0.001), and higher total hospital charges (+$6,399, p< 0.001). Teaching hospitals had higher adjusted odds of colonoscopy, angiography, and embolization. Early colonoscopy rates did not differ (Table 2).
Discussion: In this nationally representative analysis of LGIB hospitalizations, admission to teaching hospitals was associated with higher in-hospital mortality, prolonged LOS, and increased healthcare costs, likely due to more frequent use of diagnostic and therapeutic procedures. These differences may reflect the referral of more complex or acutely ill patients to teaching centers. The lack of difference in early colonoscopy rates suggests that factors beyond timing of intervention may contribute to outcome disparities. Further investigation is warranted to better understand the role of hospital-level factors in shaping LGIB outcomes and to identify opportunities for improving care across all hospital settings.
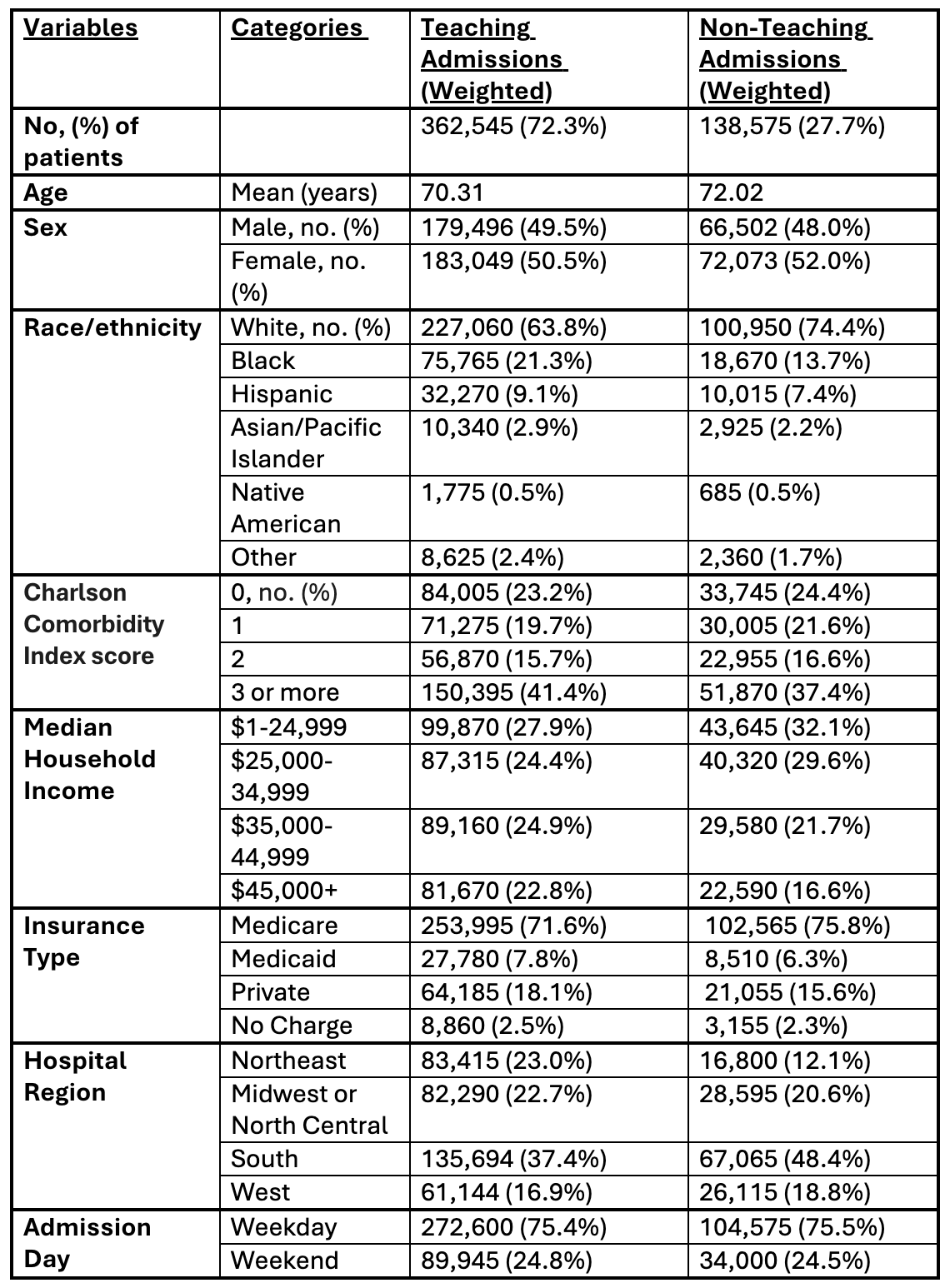
Figure: Table 1. Baseline Characteristics
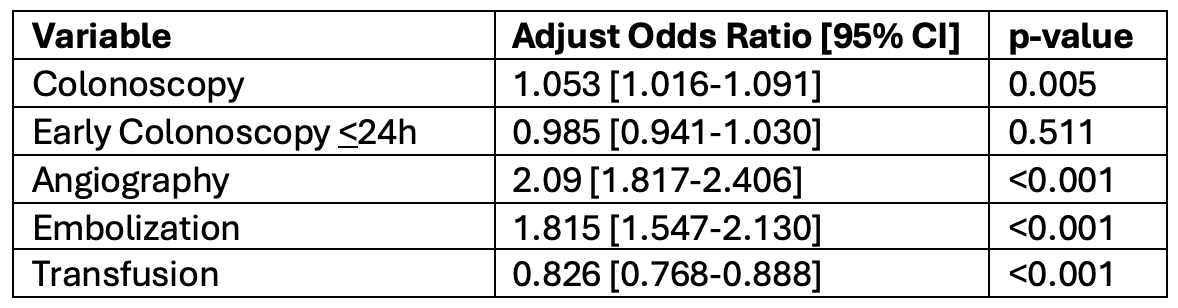
Figure: Table 2. Adjusted Odds of Interventions in LGIB Admissions: Teaching vs. Non-Teaching Hospitals
Disclosures:
James Lee indicated no relevant financial relationships.
Rahul Tripathi indicated no relevant financial relationships.
Alan Abboud indicated no relevant financial relationships.
Matthew Obusan indicated no relevant financial relationships.
Lisa Fisher indicated no relevant financial relationships.
Daniel Jamorabo indicated no relevant financial relationships.
James Lee, MD1, Rahul Tripathi, MD1, Alan Abboud, MD1, Matthew Obusan, BS2, Lisa Fisher, MD3, Daniel Jamorabo, MD4. P3074 - Outcomes of Lower Gastrointestinal Bleeding at Teaching vs Non-Teaching Hospitals: A Nationwide Inpatient Sample Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
