Monday Poster Session
Category: GI Bleeding
P3069 - Clinical Outcomes of Gastrointestinal Bleeding in DOAC and Warfarin-Related Hospitalizations: A Population-Based Cohort Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- SK
Sachi Khemka, MBA, BS
Texas Tech University Health Sciences Center
Amarillo, TX
Presenting Author(s)
Merry Mathew, BS1, Sachi Khemka, MBA, BS2, Anjul Verma, MD3, Avneet Kaur, MBBS4, John Garza, PhD5
1Texas Tech University Health Sciences Center School of Medicine, Odessa, TX; 2Texas Tech University Health Sciences Center, Amarillo, TX; 3Texas Tech University Health Sciences Center, Odessa, TX; 4SUNY Upstate Medical University, Syracuse, NY; 5Texas Tech University Health Sciences Center - Permian Basin, Odessa, TX
Introduction: Gastrointestinal (GI) bleeding is a frequent and serious adverse event associated with anticoagulant therapy. Although direct oral anticoagulants (DOACs) offer advantages such as fixed dosing and reduced monitoring needs, concerns remain regarding their bleeding risk, particularly in the gastrointestinal tract. Our study evaluates the relative risk of GI bleeding among hospitalized patients experiencing adverse effects from DOACs compared to warfarin, aiming to inform safer practices.
Methods: We conducted a population-based cohort study using de-identified and publicly available of adults hospitalized in Texas to acute care hospitals (2016–2023) with a diagnosis of initial encounter for adverse effect of DOAC or Warfarin identified using ICD-10 codes T45.515A and T45.516A The primary outcome was a diagnosis of gastrointestinal tract bleeding using codes selected from Clinical Classification Software Refined category DIG021: Gastrointestinal Hemorrhage. Overlap propensity score weighting was applied to adjust for confounders. Results were reported as adjusted risk ratios (aRR) with 95% confidence intervals. Subgroup analyses were performed by age, sex, race/ethnicity, insurance type, and Deyo comorbidity index.
Results: A total of 56,092 hospitalizations from 388 hospitals were analyzed, including 5,401 (9.6%) with adverse effects attributed to warfarin. Compared to DOAC-related hospitalizations, patients in the warfarin group were younger (35.9% vs. 71.9% aged ≥65 years, p < 0.0001), had a lower comorbidity burden (mean Deyo index 2.22 ± 2.11 vs. 2.53 ± 2.21, p < 0.0001), and shorter hospital stays (5.14 ± 5.04 vs. 6.80 ± 6.97 days, p < 0.0001). Gastrointestinal bleeding occurred less frequently in the warfarin group (2.7% vs. 21.1%), and this association persisted after adjustment (aRR 0.22; 95% CI: 0.18–0.26). Hospital mortality was higher with DOACs group (4.7% vs. 1.2%). Subgroup analyses yielded consistent findings across all strata.
Discussion: In this large population-based cohort, warfarin use was associated with a significantly lower adjusted risk of gastrointestinal bleeding compared to DOACs. These findings highlight important safety considerations in anticoagulant selection and support the need for risk stratification in clinical decision-making.
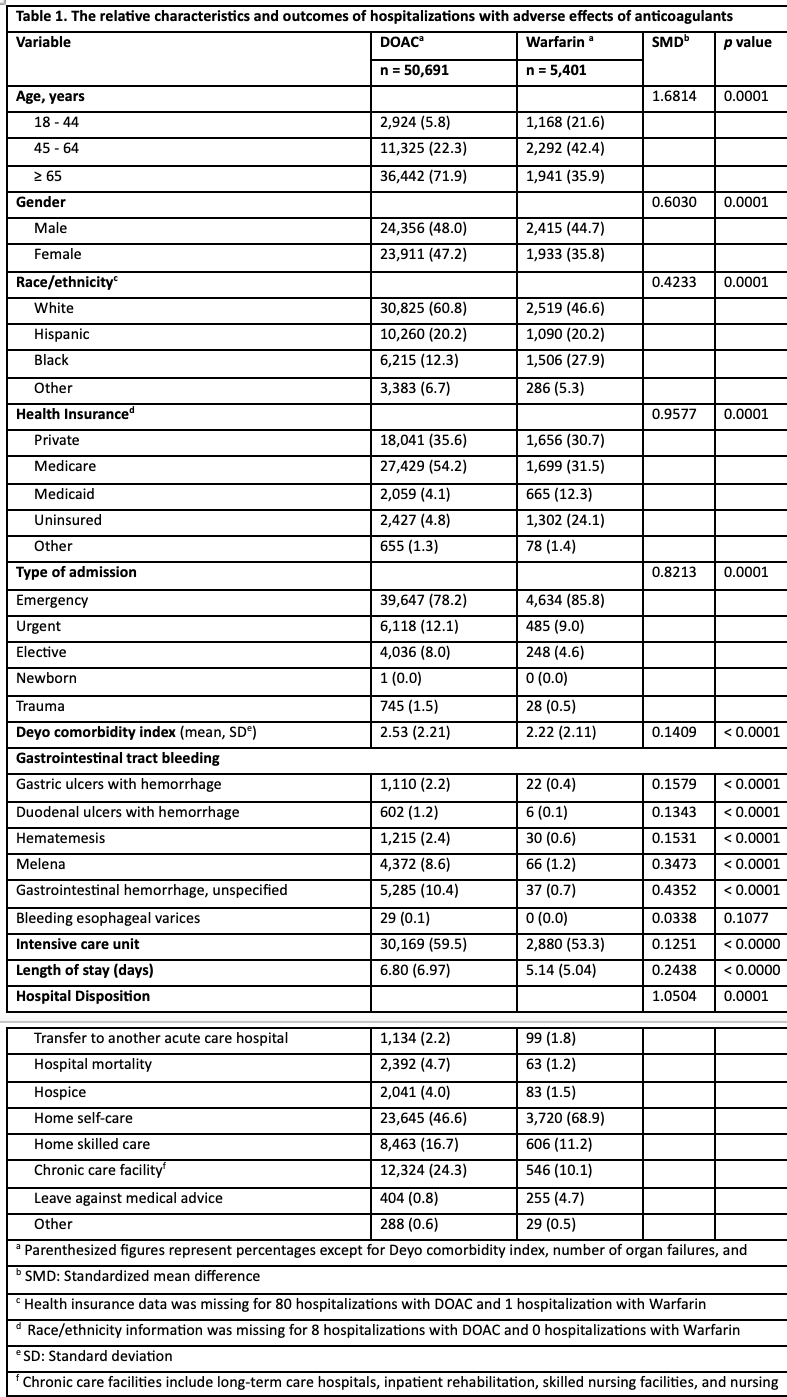
Figure: Forest Plot
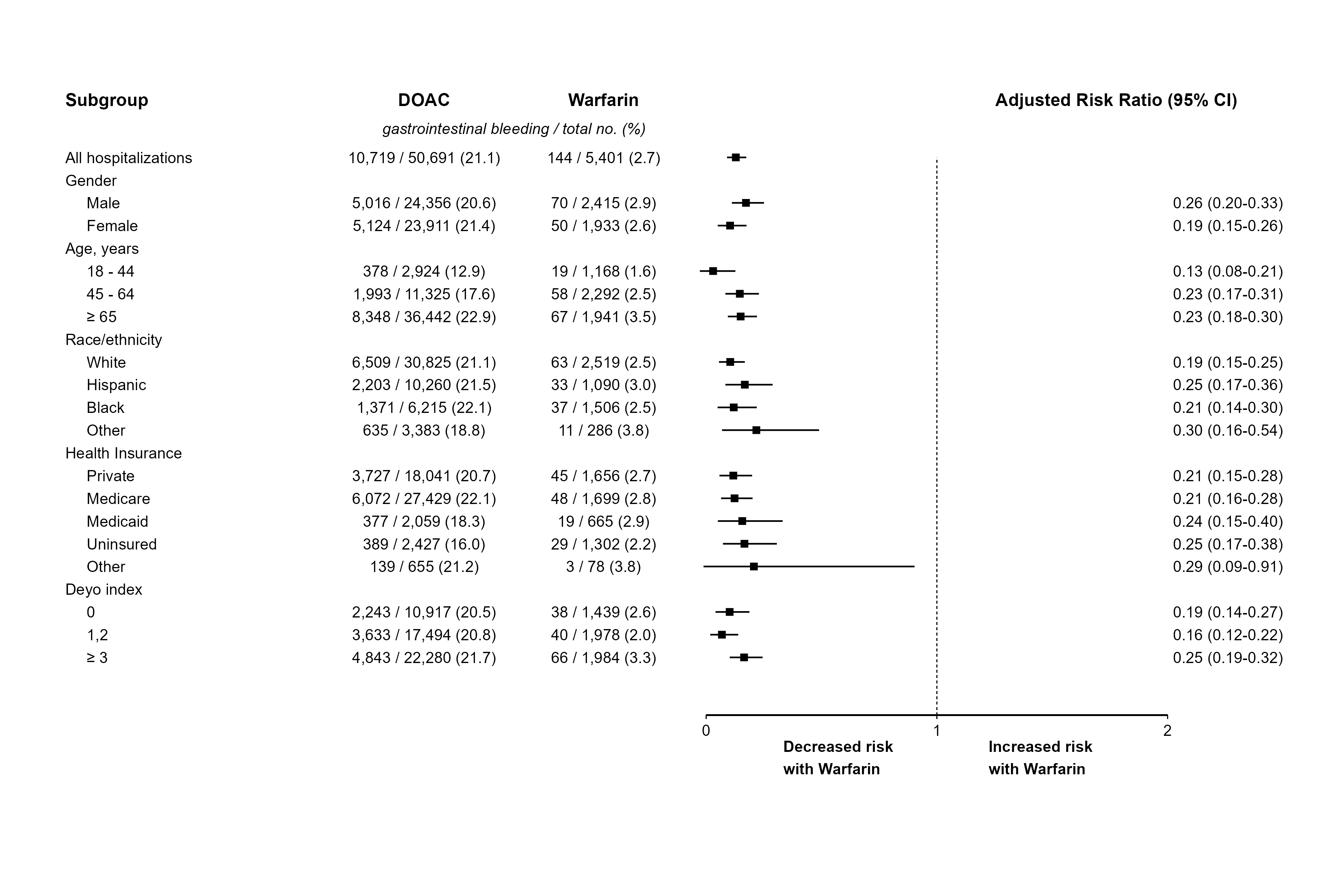
Figure: The relative characteristics and outcomes of hospitalizations with adverse effects of anticoagulants
Disclosures:
Merry Mathew indicated no relevant financial relationships.
Sachi Khemka indicated no relevant financial relationships.
Anjul Verma indicated no relevant financial relationships.
Avneet Kaur indicated no relevant financial relationships.
John Garza indicated no relevant financial relationships.
Merry Mathew, BS1, Sachi Khemka, MBA, BS2, Anjul Verma, MD3, Avneet Kaur, MBBS4, John Garza, PhD5. P3069 - Clinical Outcomes of Gastrointestinal Bleeding in DOAC and Warfarin-Related Hospitalizations: A Population-Based Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Texas Tech University Health Sciences Center School of Medicine, Odessa, TX; 2Texas Tech University Health Sciences Center, Amarillo, TX; 3Texas Tech University Health Sciences Center, Odessa, TX; 4SUNY Upstate Medical University, Syracuse, NY; 5Texas Tech University Health Sciences Center - Permian Basin, Odessa, TX
Introduction: Gastrointestinal (GI) bleeding is a frequent and serious adverse event associated with anticoagulant therapy. Although direct oral anticoagulants (DOACs) offer advantages such as fixed dosing and reduced monitoring needs, concerns remain regarding their bleeding risk, particularly in the gastrointestinal tract. Our study evaluates the relative risk of GI bleeding among hospitalized patients experiencing adverse effects from DOACs compared to warfarin, aiming to inform safer practices.
Methods: We conducted a population-based cohort study using de-identified and publicly available of adults hospitalized in Texas to acute care hospitals (2016–2023) with a diagnosis of initial encounter for adverse effect of DOAC or Warfarin identified using ICD-10 codes T45.515A and T45.516A The primary outcome was a diagnosis of gastrointestinal tract bleeding using codes selected from Clinical Classification Software Refined category DIG021: Gastrointestinal Hemorrhage. Overlap propensity score weighting was applied to adjust for confounders. Results were reported as adjusted risk ratios (aRR) with 95% confidence intervals. Subgroup analyses were performed by age, sex, race/ethnicity, insurance type, and Deyo comorbidity index.
Results: A total of 56,092 hospitalizations from 388 hospitals were analyzed, including 5,401 (9.6%) with adverse effects attributed to warfarin. Compared to DOAC-related hospitalizations, patients in the warfarin group were younger (35.9% vs. 71.9% aged ≥65 years, p < 0.0001), had a lower comorbidity burden (mean Deyo index 2.22 ± 2.11 vs. 2.53 ± 2.21, p < 0.0001), and shorter hospital stays (5.14 ± 5.04 vs. 6.80 ± 6.97 days, p < 0.0001). Gastrointestinal bleeding occurred less frequently in the warfarin group (2.7% vs. 21.1%), and this association persisted after adjustment (aRR 0.22; 95% CI: 0.18–0.26). Hospital mortality was higher with DOACs group (4.7% vs. 1.2%). Subgroup analyses yielded consistent findings across all strata.
Discussion: In this large population-based cohort, warfarin use was associated with a significantly lower adjusted risk of gastrointestinal bleeding compared to DOACs. These findings highlight important safety considerations in anticoagulant selection and support the need for risk stratification in clinical decision-making.
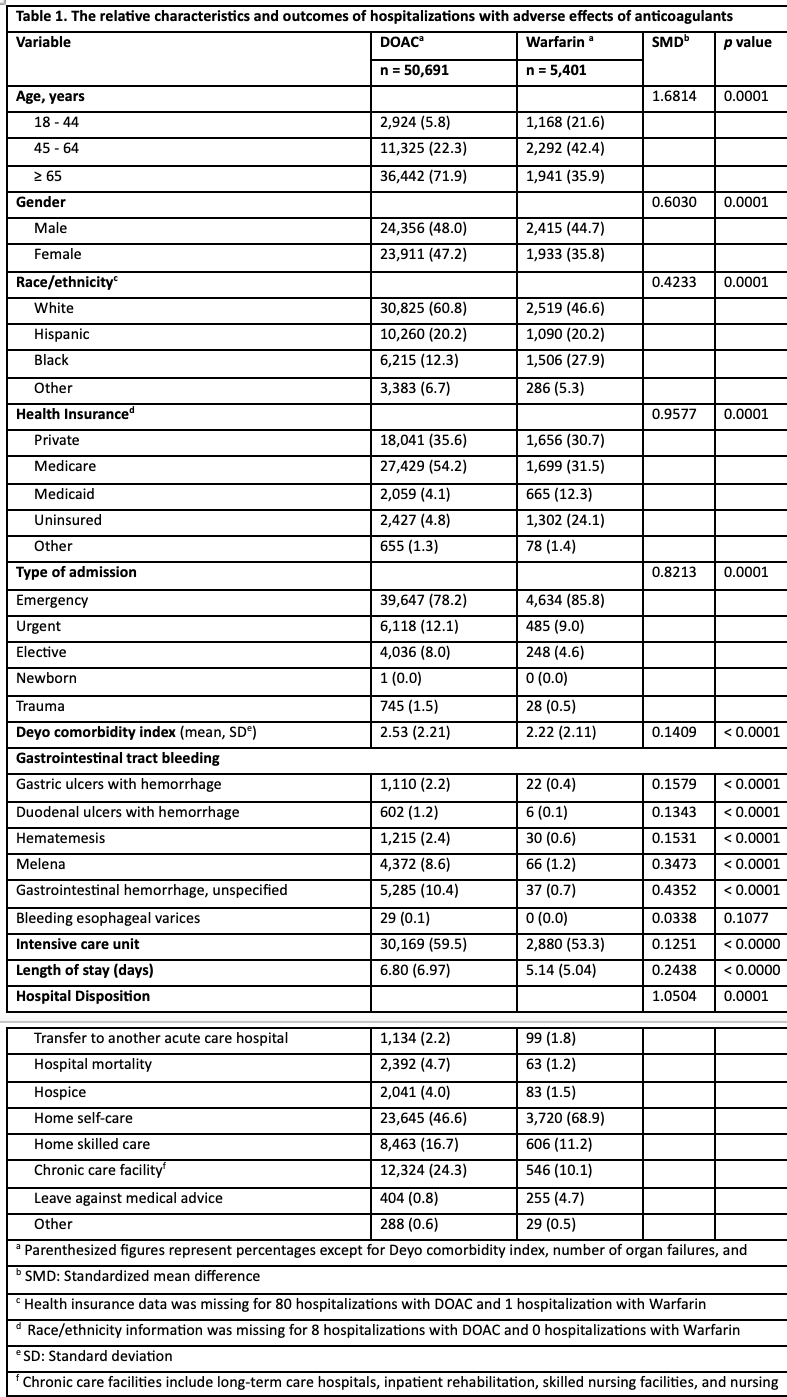
Figure: Forest Plot
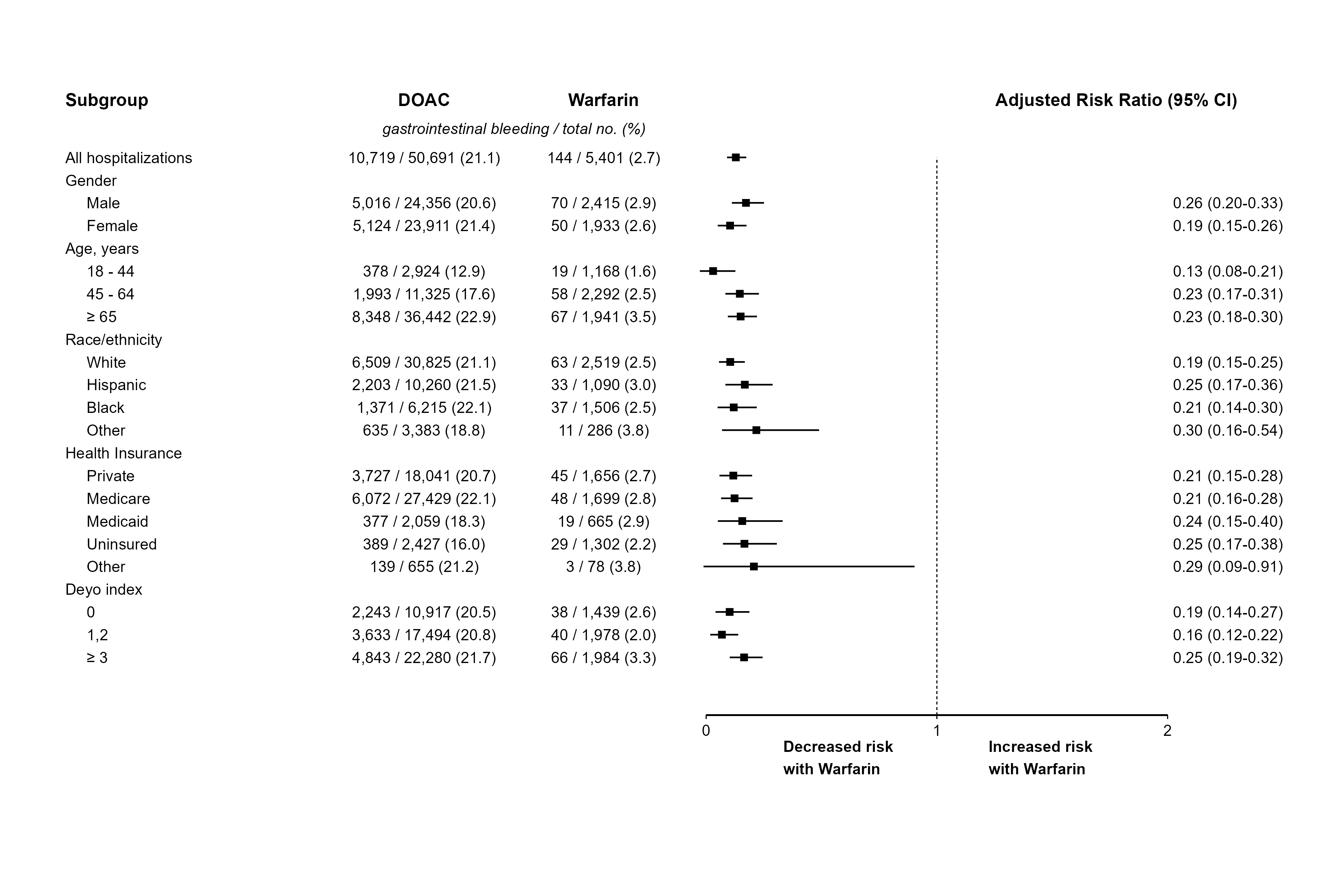
Figure: The relative characteristics and outcomes of hospitalizations with adverse effects of anticoagulants
Disclosures:
Merry Mathew indicated no relevant financial relationships.
Sachi Khemka indicated no relevant financial relationships.
Anjul Verma indicated no relevant financial relationships.
Avneet Kaur indicated no relevant financial relationships.
John Garza indicated no relevant financial relationships.
Merry Mathew, BS1, Sachi Khemka, MBA, BS2, Anjul Verma, MD3, Avneet Kaur, MBBS4, John Garza, PhD5. P3069 - Clinical Outcomes of Gastrointestinal Bleeding in DOAC and Warfarin-Related Hospitalizations: A Population-Based Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
