Monday Poster Session
Category: GI Bleeding
P3067 - Trends in Gastrointestinal Bleeding-Related Mortality Among Adults With Chronic Kidney Disease in the United States, 1999-2020
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Anmol Mohan, MD
Carle Foundation hospital
Urbana, Pakistan
Presenting Author(s)
Anmol Mohan, MD1, Jazza Aamir, MD2, Abdullah Sultany, MD3
1Carle Foundation hospital, Urbana, IL; 2Dow University of Health Sciences, Department of Medicine, Karachi, Sindh, Pakistan; 3Guthrie Robert Packer Hospital, Department of Internal Medicine, Sayre, PA
Introduction: Gastrointestinal (GI) bleeding is a critical complication for chronic kidney disease (CKD) patients, raising mortality risks due to physiological changes and comorbidities. This study analyzes GI bleeding-related mortality trends among CKD patients in the United States (US) from 1999 to 2020.
Methods: Data from the Centers for Disease Control and Prevention Wide‐ranging Online Data for Epidemiologic Research (CDC WONDER) on US CKD patients aged ≥ 25 years, with CKD and GI bleeding listed as underlying or contributing causes of death, were analyzed for GI bleeding-related mortality. Age‐adjusted mortality rates (AAMRs) per 100,000 were calculated, and Joinpoint regression assessed trends. Annual percentage change (APC), and average annual percentage change (AAPC) stratified by year, gender, race, and geographic region.
Results: A total of 41,697 GI bleeding–related deaths occurred among CKD patients. AAMR increased from 1.1 per 100,000 in 1999 to 3.0 in 2020 (AAPC 4.2 %; 95 % CI: 2.9–5.4 %). From 1999 to 2009, AAMR declined to 0.8 (APC –2.9 %; 95 % CI: –8.2–0.0 %), surged to 2.0 by 2012 (APC 31.4 %; 95 % CI: 12.5–41.9 %), then rose gradually to 3.0 by 2020 (APC 4.4 %; 95 % CI: –2.2–7.1 %). Males had higher AAMR (2.1; AAPC 3.9 %; 95 % CI: 2.6–5.0 %) than females (1.3; AAPC 4.3 %; 95 % CI: 2.9–5.4 %). By race, non‐Hispanic Black patients had the highest AAMR (3.4; AAPC 2.7 %; 95 % CI: 1.3–4.2 %), with declines from 1999–2008, a sharp rise through 2011, and a moderate increase thereafter. Non‐Hispanic Asian/Pacific Islander patients had AAMR 1.8 (AAPC 3.8 %; 95 % CI: 2.1–7.0 %), Hispanic patients 1.8 (AAPC 3.3 %; 95 % CI: 1.7–4.8 %), and non‐Hispanic White patients 1.4 (AAPC 4.5 %; 95 % CI: 3.4–5.6 %). Non‐metropolitan areas recorded AAMR 1.8 (AAPC 4.1 %; 95 % CI: 2.8–5.4 %) compared to metropolitan areas 1.6 (AAPC 4.1 %; 95 % CI: 2.8–5.7 %). Regionally, the Midwest had AAMR 1.7 (AAPC 4.1 %; 95 % CI: 2.9–5.3 %), the West 1.6 (AAPC 4.8 %; 95 % CI: 3.2–6.2 %), the South 1.6 (AAPC 4.0 %; 95 % CI: 2.4–5.4 %), and the Northeast 1.5 (AAPC 3.6 %; 95 % CI: 1.9–5.1 %). States in the top 90th percentile of AAMR included South Carolina, District of Columbia, and Rhode Island (2.6); South Dakota (2.4); and Washington and North Dakota (2.3).
Discussion: GI bleeding-related mortality among CKD patients in the U.S. has markedly increased over the past two decades. Demographic and geographic disparities underscore the need for targeted public health efforts to improve outcomes for at-risk CKD patients.
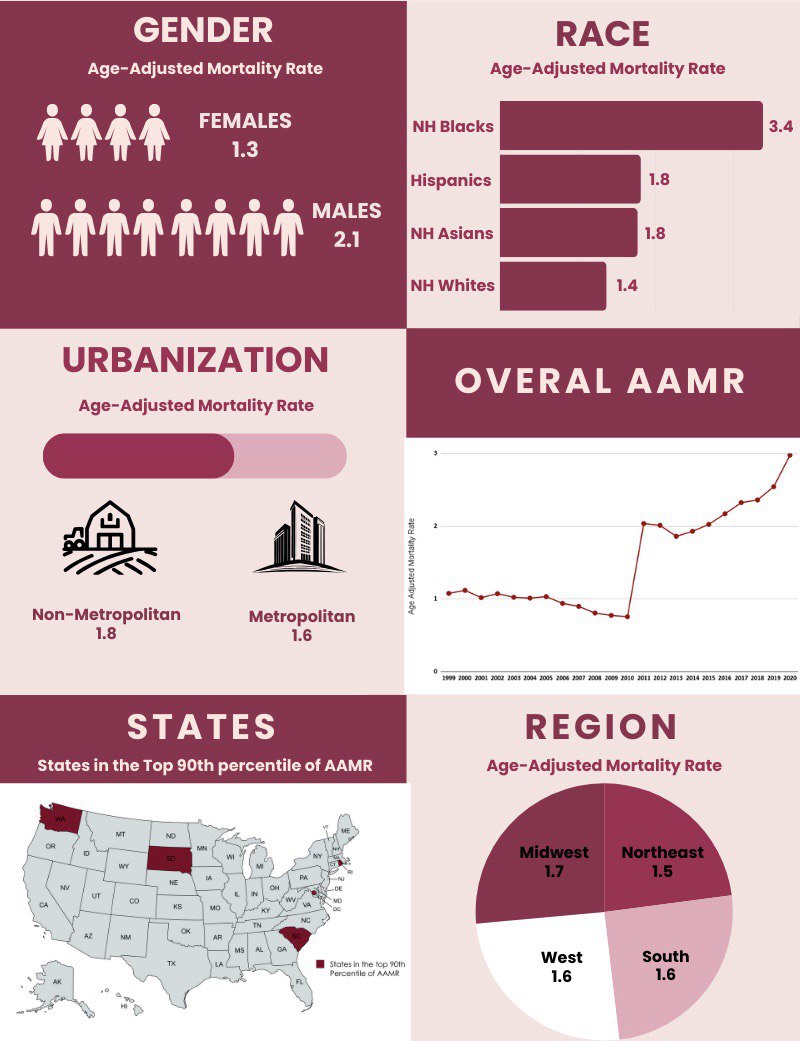
Figure: Figure 1. Trends in GI Bleeding-Related Mortality Among Patients With Chronic Kidney Disease in the U.S, 1999–2020.
Disclosures:
Anmol Mohan indicated no relevant financial relationships.
Jazza Aamir indicated no relevant financial relationships.
Abdullah Sultany indicated no relevant financial relationships.
Anmol Mohan, MD1, Jazza Aamir, MD2, Abdullah Sultany, MD3. P3067 - Trends in Gastrointestinal Bleeding-Related Mortality Among Adults With Chronic Kidney Disease in the United States, 1999-2020, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Carle Foundation hospital, Urbana, IL; 2Dow University of Health Sciences, Department of Medicine, Karachi, Sindh, Pakistan; 3Guthrie Robert Packer Hospital, Department of Internal Medicine, Sayre, PA
Introduction: Gastrointestinal (GI) bleeding is a critical complication for chronic kidney disease (CKD) patients, raising mortality risks due to physiological changes and comorbidities. This study analyzes GI bleeding-related mortality trends among CKD patients in the United States (US) from 1999 to 2020.
Methods: Data from the Centers for Disease Control and Prevention Wide‐ranging Online Data for Epidemiologic Research (CDC WONDER) on US CKD patients aged ≥ 25 years, with CKD and GI bleeding listed as underlying or contributing causes of death, were analyzed for GI bleeding-related mortality. Age‐adjusted mortality rates (AAMRs) per 100,000 were calculated, and Joinpoint regression assessed trends. Annual percentage change (APC), and average annual percentage change (AAPC) stratified by year, gender, race, and geographic region.
Results: A total of 41,697 GI bleeding–related deaths occurred among CKD patients. AAMR increased from 1.1 per 100,000 in 1999 to 3.0 in 2020 (AAPC 4.2 %; 95 % CI: 2.9–5.4 %). From 1999 to 2009, AAMR declined to 0.8 (APC –2.9 %; 95 % CI: –8.2–0.0 %), surged to 2.0 by 2012 (APC 31.4 %; 95 % CI: 12.5–41.9 %), then rose gradually to 3.0 by 2020 (APC 4.4 %; 95 % CI: –2.2–7.1 %). Males had higher AAMR (2.1; AAPC 3.9 %; 95 % CI: 2.6–5.0 %) than females (1.3; AAPC 4.3 %; 95 % CI: 2.9–5.4 %). By race, non‐Hispanic Black patients had the highest AAMR (3.4; AAPC 2.7 %; 95 % CI: 1.3–4.2 %), with declines from 1999–2008, a sharp rise through 2011, and a moderate increase thereafter. Non‐Hispanic Asian/Pacific Islander patients had AAMR 1.8 (AAPC 3.8 %; 95 % CI: 2.1–7.0 %), Hispanic patients 1.8 (AAPC 3.3 %; 95 % CI: 1.7–4.8 %), and non‐Hispanic White patients 1.4 (AAPC 4.5 %; 95 % CI: 3.4–5.6 %). Non‐metropolitan areas recorded AAMR 1.8 (AAPC 4.1 %; 95 % CI: 2.8–5.4 %) compared to metropolitan areas 1.6 (AAPC 4.1 %; 95 % CI: 2.8–5.7 %). Regionally, the Midwest had AAMR 1.7 (AAPC 4.1 %; 95 % CI: 2.9–5.3 %), the West 1.6 (AAPC 4.8 %; 95 % CI: 3.2–6.2 %), the South 1.6 (AAPC 4.0 %; 95 % CI: 2.4–5.4 %), and the Northeast 1.5 (AAPC 3.6 %; 95 % CI: 1.9–5.1 %). States in the top 90th percentile of AAMR included South Carolina, District of Columbia, and Rhode Island (2.6); South Dakota (2.4); and Washington and North Dakota (2.3).
Discussion: GI bleeding-related mortality among CKD patients in the U.S. has markedly increased over the past two decades. Demographic and geographic disparities underscore the need for targeted public health efforts to improve outcomes for at-risk CKD patients.
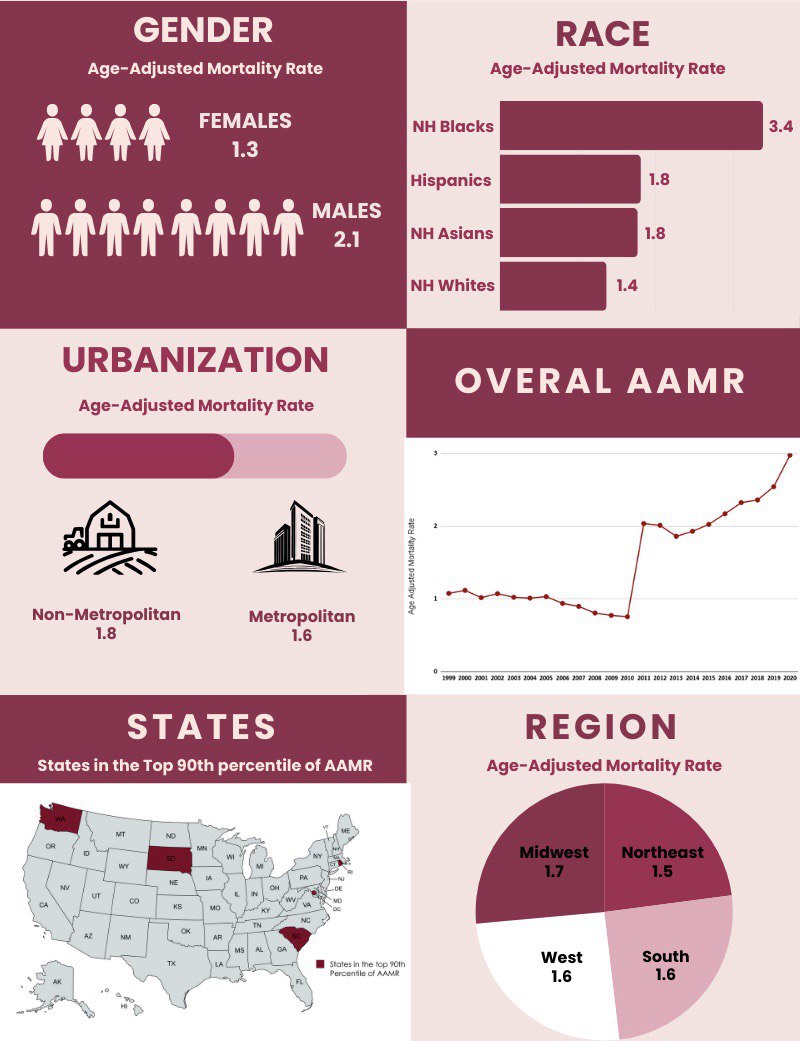
Figure: Figure 1. Trends in GI Bleeding-Related Mortality Among Patients With Chronic Kidney Disease in the U.S, 1999–2020.
Disclosures:
Anmol Mohan indicated no relevant financial relationships.
Jazza Aamir indicated no relevant financial relationships.
Abdullah Sultany indicated no relevant financial relationships.
Anmol Mohan, MD1, Jazza Aamir, MD2, Abdullah Sultany, MD3. P3067 - Trends in Gastrointestinal Bleeding-Related Mortality Among Adults With Chronic Kidney Disease in the United States, 1999-2020, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

