Monday Poster Session
Category: General Endoscopy
P3015 - When the Stomach Lives in the Chest: A Case of an Entirely Intrathoracic Type III Paraesophageal Hernia
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Pei-Hsuan Li, DO (she/her/hers)
Oregon Health & Science University
Portland, OR
Presenting Author(s)
Pei-Hsuan Li, DO1, Patrick Stauffer, MD1, Caitlin Citti, MD2
1Oregon Health & Science University, Portland, OR; 2VA Portland Medical Center, Portland, OR
Introduction: A paraesophageal hernia (PEH) occurs when the gastroesophageal (GE) junction, stomach, or other abdominal organs herniate through the diaphragmatic hiatus into the thoracic cavity. PEHs are classified into four types based on the degree of herniation and the structures involved. A type III PEH is a combination of both types I and II, in which both the GE junction and a portion of the stomach migrate into the chest. Symptoms can range from asymptomatic to postprandial discomfort, early satiety, and progressive dysphagia, which can ultimately result in malnutrition and failure to thrive. The anatomical distortion associated with type III PEHs poses a significant risk for serious complications, including aspiration, gastric volvulus, strangulation, and cardiopulmonary compromise. This case highlights the endoscopic finding of a large type III PEH with complete intrathoracic migration of the stomach.
Case Description/
Methods: A 65-year-old male presented with six months of progressive dysphagia accompanied by regurgitation, nausea, vomiting, and an insidious weight loss of 40 pounds. CT chest/abdomen/pelvis showed an infiltrative mass at the GE junction and proximal gastric cardia, along with enlarged paraesophageal lymph nodes (Figure 1). No evidence of metastatic disease was identified on the imaging, and subsequent malignancy workup was unremarkable. An EGD was performed and revealed LA Grade D esophagitis and a large type III PEH with complete intrathoracic migration of the stomach, with the antrum angulated cranially (Figure 2). His symptoms from esophagitis improved significantly with IV pantoprazole. He was referred to general surgery and has plans for hiatal hernia repair and Nissen fundoplication.
Discussion: This case presents radiographic concern for malignancy resulting in an endoscopic finding of a completely intrathoracic Type III PEH with LA grade D esophagitis in a hemodynamically stable patient. While no acute complications were present at the time of presentation, there is an increased risk of volvulus, strangulation, and gastric ischemia due to potential compromised vascular supply to the organs trapped in the chest. Upper GI bleeding from severe reflux esophagitis may also occur. Therefore, early recognition and surgical evaluation are important to prevent these life-threatening sequelae, even in the absence of severe or acute symptoms.
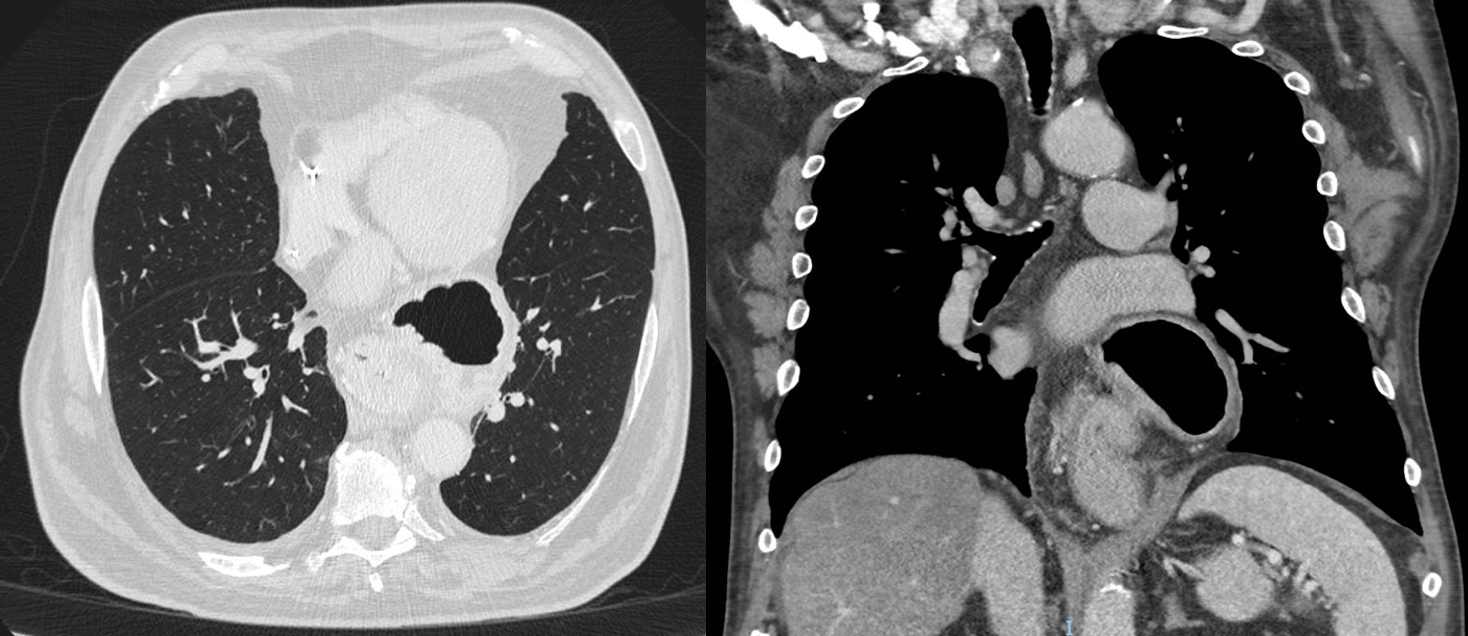
Figure: Figure 1: CT Chest showing a complete intrathoracic paraesophageal hernia in (A) axial view (B) coronal view

Figure: Figure 2: Endoscopic retroflexion of the GE junction within the hernia sac
Disclosures:
Pei-Hsuan Li indicated no relevant financial relationships.
Patrick Stauffer indicated no relevant financial relationships.
Caitlin Citti indicated no relevant financial relationships.
Pei-Hsuan Li, DO1, Patrick Stauffer, MD1, Caitlin Citti, MD2. P3015 - When the Stomach Lives in the Chest: A Case of an Entirely Intrathoracic Type III Paraesophageal Hernia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Oregon Health & Science University, Portland, OR; 2VA Portland Medical Center, Portland, OR
Introduction: A paraesophageal hernia (PEH) occurs when the gastroesophageal (GE) junction, stomach, or other abdominal organs herniate through the diaphragmatic hiatus into the thoracic cavity. PEHs are classified into four types based on the degree of herniation and the structures involved. A type III PEH is a combination of both types I and II, in which both the GE junction and a portion of the stomach migrate into the chest. Symptoms can range from asymptomatic to postprandial discomfort, early satiety, and progressive dysphagia, which can ultimately result in malnutrition and failure to thrive. The anatomical distortion associated with type III PEHs poses a significant risk for serious complications, including aspiration, gastric volvulus, strangulation, and cardiopulmonary compromise. This case highlights the endoscopic finding of a large type III PEH with complete intrathoracic migration of the stomach.
Case Description/
Methods: A 65-year-old male presented with six months of progressive dysphagia accompanied by regurgitation, nausea, vomiting, and an insidious weight loss of 40 pounds. CT chest/abdomen/pelvis showed an infiltrative mass at the GE junction and proximal gastric cardia, along with enlarged paraesophageal lymph nodes (Figure 1). No evidence of metastatic disease was identified on the imaging, and subsequent malignancy workup was unremarkable. An EGD was performed and revealed LA Grade D esophagitis and a large type III PEH with complete intrathoracic migration of the stomach, with the antrum angulated cranially (Figure 2). His symptoms from esophagitis improved significantly with IV pantoprazole. He was referred to general surgery and has plans for hiatal hernia repair and Nissen fundoplication.
Discussion: This case presents radiographic concern for malignancy resulting in an endoscopic finding of a completely intrathoracic Type III PEH with LA grade D esophagitis in a hemodynamically stable patient. While no acute complications were present at the time of presentation, there is an increased risk of volvulus, strangulation, and gastric ischemia due to potential compromised vascular supply to the organs trapped in the chest. Upper GI bleeding from severe reflux esophagitis may also occur. Therefore, early recognition and surgical evaluation are important to prevent these life-threatening sequelae, even in the absence of severe or acute symptoms.
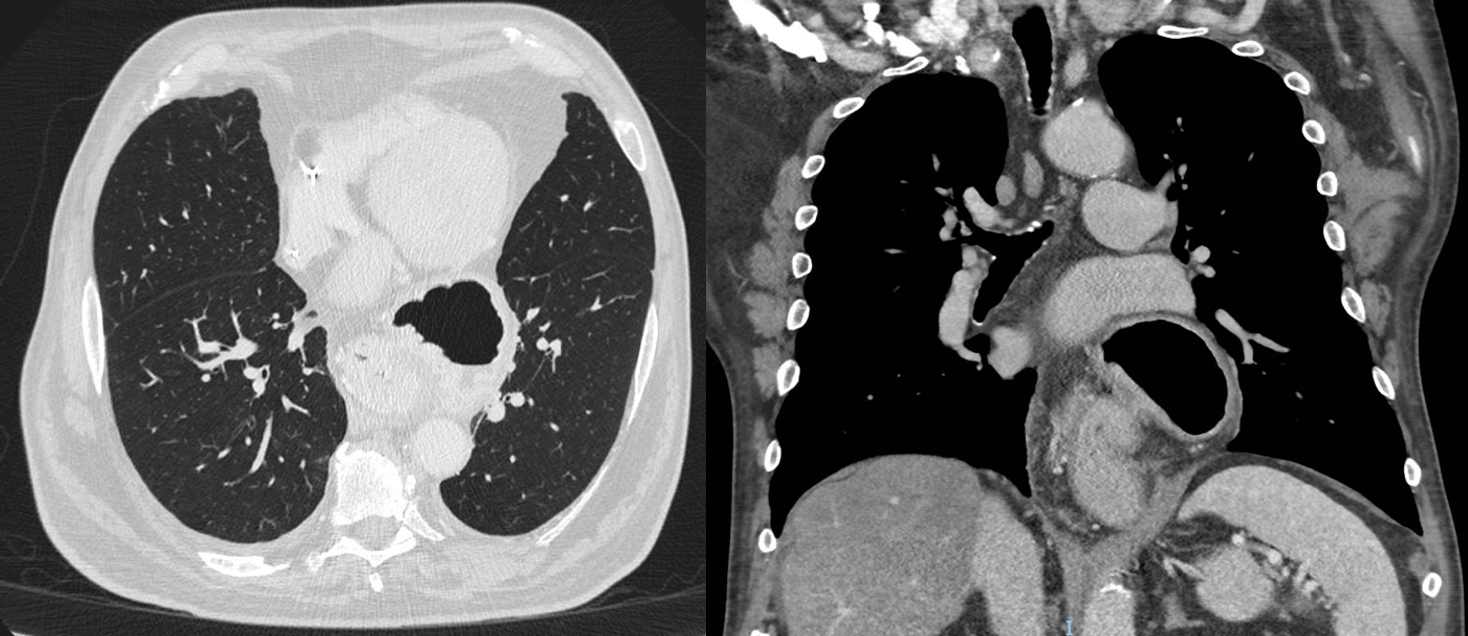
Figure: Figure 1: CT Chest showing a complete intrathoracic paraesophageal hernia in (A) axial view (B) coronal view

Figure: Figure 2: Endoscopic retroflexion of the GE junction within the hernia sac
Disclosures:
Pei-Hsuan Li indicated no relevant financial relationships.
Patrick Stauffer indicated no relevant financial relationships.
Caitlin Citti indicated no relevant financial relationships.
Pei-Hsuan Li, DO1, Patrick Stauffer, MD1, Caitlin Citti, MD2. P3015 - When the Stomach Lives in the Chest: A Case of an Entirely Intrathoracic Type III Paraesophageal Hernia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
