Monday Poster Session
Category: General Endoscopy
P3011 - Beyond the Bloodstream: Gastrointestinal Involvement in Idiopathic Hyper-Eosinophilic Syndrome
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- JS
Jowana Saba, MD (she/her/hers)
Texas Tech University Health Sciences Center
Lubbock, TX
Presenting Author(s)
Jowana Saba, MD1, Mohamad Altabaa, MBA1, Arman Vaghefi, BS2, Marcial Ruiz, 3, Houssam Kharrat, MD4
1Texas Tech University Health Sciences Center, Lubbock, TX; 2Rocky Vista University, Colorado Springs, CO; 3Caprock Gastro Research, Lubbock, TX; 4West Texas Digestive Disease Center, Lubbock, TX
Introduction: Hypereosinophilic Syndrome (HES) is a rare group of disorders characterized by prolonged eosinophilia, with tissue damage. We present here a rare case of idiopathic hypereosinophilic syndrome with primary gastrointestinal involvement.
Case Description/
Methods: The patient is a 25-year-old woman, history of asthma and multiple food allergies, with a two-week history of intermittent right-sided abdominal pain, worsened by food, associated with nausea, vomiting, and intermittent diarrhea. Her vital signs were normal, she appeared ill with dry mucous membranes and diffuse abdominal tenderness. Laboratory tests elevated WBC 44, with 69% eosinophils, Hgb of 14.5, and platelet 258. A CT scan of the abdomen and pelvis showed dilated, fluid-filled loops of the small bowel, multiple thickened small bowel loops, ascites, and small bilateral pleural effusions.
Despite empiric treatment with albendazole initiated by the infectious disease team, her eosinophil count continued to rise. Stool testing was negative. Peripheral smear showed severe eosinophilia with mild neutrophilia.
Given that the absolute neutrophil count was 30, the patient met the criteria for idiopathic hypereosinophilic syndrome and was started on Solumedrol 60 mg IV TID. She exhibited a dramatic decrease in WBC count from 42 (79% eosinophils) in the morning to 17 (65.8% eosinophils) by the afternoon, and further to 11 (2.4% eosinophils) the following day, with marked improvement in her symptoms. The patient was then transitioned to a tapering dose of steroids, along with an antihistamine, an H2 blocker, and an anti-IL-5 antibody.
Discussion: Hypereosinophilic syndrome (HES) is diagnosed when hypereosinophilia is accompanied by tissue damage and other potential causes of eosinophilia or tissue damage are excluded.
HES with primary gastrointestinal eosinophilic diseases (EGIDs) is rare, with only 34 reported cases.
we report a 25-year-old female with idiopathic IHES and multifocal gastrointestinal involvement.
There are no formal guidelines for managing EGIDs, current recommendations include dietary modifications, Glucocorticoids, In our case, Solumedrol 60 mg IV TID led to significant and rapid improvement in both laboratory markers and clinical symptoms.
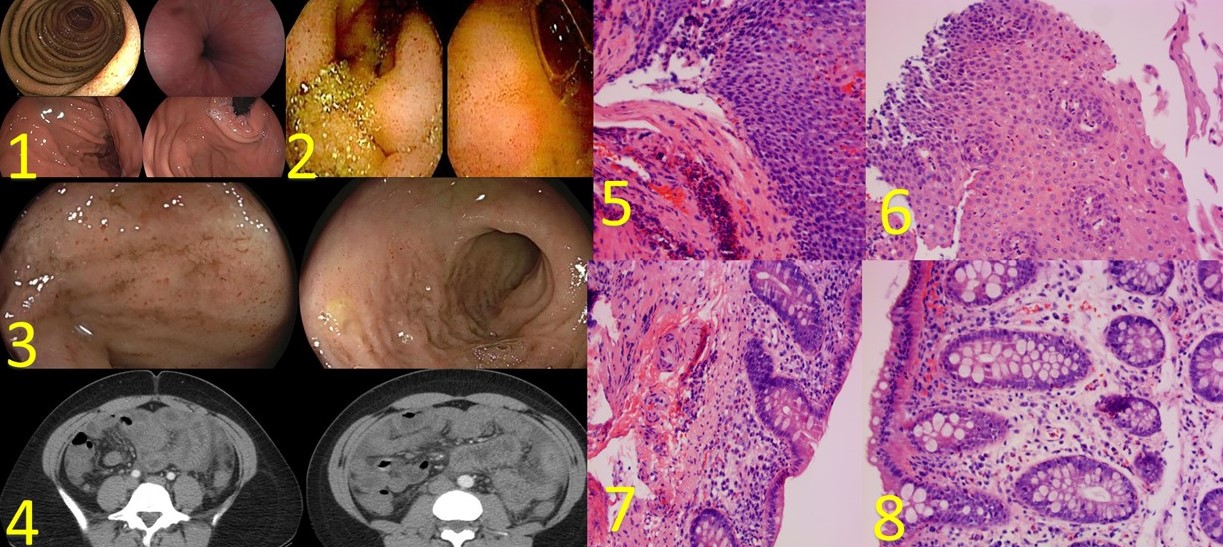
Figure: 1 Gastric Mucosa Erythema
2 Capsule endoscopy, erythema throughout the small bowel
3 Colonic erythema
4 CT, Small Bowel filled with fluid and small bowel edema.
5-6 Esophagus with eosinophilic infiltrations
7-8 Cecum and descending colon with eosinophilic infiltrations
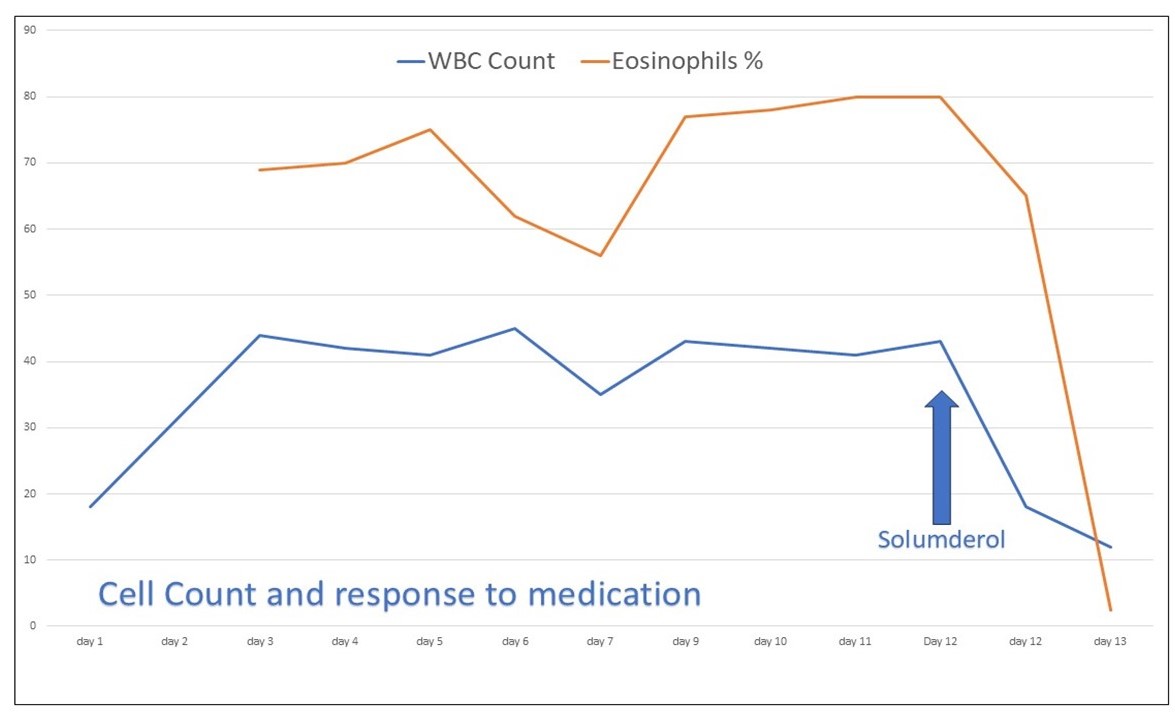
Figure: Dramatic response to Steroid
Disclosures:
Jowana Saba indicated no relevant financial relationships.
Mohamad Altabaa indicated no relevant financial relationships.
Arman Vaghefi indicated no relevant financial relationships.
Marcial Ruiz indicated no relevant financial relationships.
Houssam Kharrat indicated no relevant financial relationships.
Jowana Saba, MD1, Mohamad Altabaa, MBA1, Arman Vaghefi, BS2, Marcial Ruiz, 3, Houssam Kharrat, MD4. P3011 - Beyond the Bloodstream: Gastrointestinal Involvement in Idiopathic Hyper-Eosinophilic Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Texas Tech University Health Sciences Center, Lubbock, TX; 2Rocky Vista University, Colorado Springs, CO; 3Caprock Gastro Research, Lubbock, TX; 4West Texas Digestive Disease Center, Lubbock, TX
Introduction: Hypereosinophilic Syndrome (HES) is a rare group of disorders characterized by prolonged eosinophilia, with tissue damage. We present here a rare case of idiopathic hypereosinophilic syndrome with primary gastrointestinal involvement.
Case Description/
Methods: The patient is a 25-year-old woman, history of asthma and multiple food allergies, with a two-week history of intermittent right-sided abdominal pain, worsened by food, associated with nausea, vomiting, and intermittent diarrhea. Her vital signs were normal, she appeared ill with dry mucous membranes and diffuse abdominal tenderness. Laboratory tests elevated WBC 44, with 69% eosinophils, Hgb of 14.5, and platelet 258. A CT scan of the abdomen and pelvis showed dilated, fluid-filled loops of the small bowel, multiple thickened small bowel loops, ascites, and small bilateral pleural effusions.
Despite empiric treatment with albendazole initiated by the infectious disease team, her eosinophil count continued to rise. Stool testing was negative. Peripheral smear showed severe eosinophilia with mild neutrophilia.
- EGD: Mildly inflamed stomach with a normal duodenum. with increased tissue eosinophilia involving the lamina propria.
- Colonoscopy: inflamed, and nodular mucosa in the colon and terminal ileum. with increased lamina propria eosinophils throughout.
- Bone marrow biopsy: negative.
Given that the absolute neutrophil count was 30, the patient met the criteria for idiopathic hypereosinophilic syndrome and was started on Solumedrol 60 mg IV TID. She exhibited a dramatic decrease in WBC count from 42 (79% eosinophils) in the morning to 17 (65.8% eosinophils) by the afternoon, and further to 11 (2.4% eosinophils) the following day, with marked improvement in her symptoms. The patient was then transitioned to a tapering dose of steroids, along with an antihistamine, an H2 blocker, and an anti-IL-5 antibody.
Discussion: Hypereosinophilic syndrome (HES) is diagnosed when hypereosinophilia is accompanied by tissue damage and other potential causes of eosinophilia or tissue damage are excluded.
HES with primary gastrointestinal eosinophilic diseases (EGIDs) is rare, with only 34 reported cases.
we report a 25-year-old female with idiopathic IHES and multifocal gastrointestinal involvement.
There are no formal guidelines for managing EGIDs, current recommendations include dietary modifications, Glucocorticoids, In our case, Solumedrol 60 mg IV TID led to significant and rapid improvement in both laboratory markers and clinical symptoms.
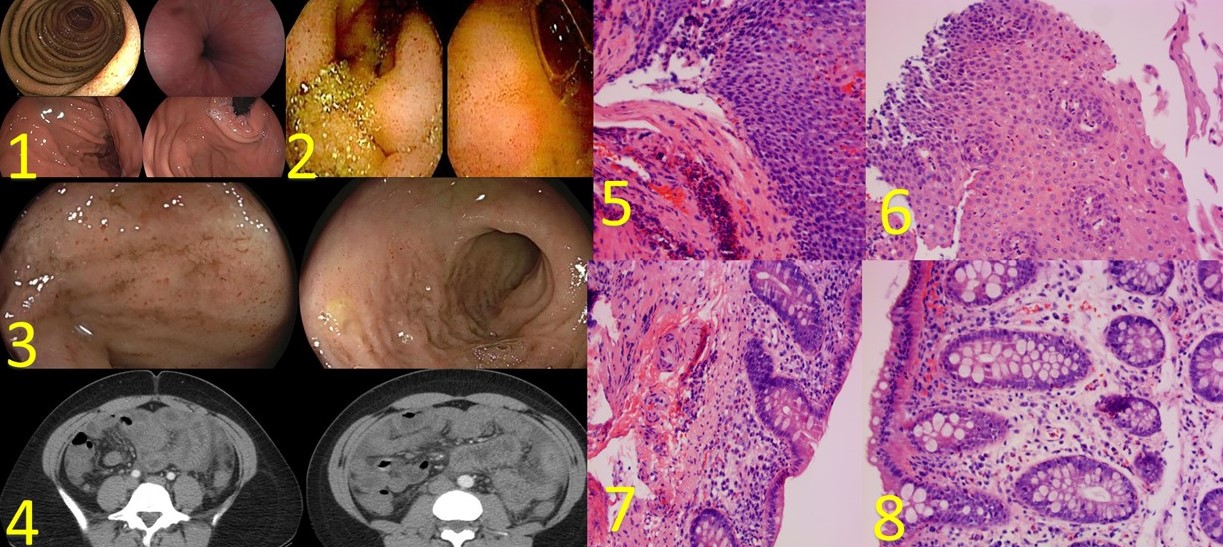
Figure: 1 Gastric Mucosa Erythema
2 Capsule endoscopy, erythema throughout the small bowel
3 Colonic erythema
4 CT, Small Bowel filled with fluid and small bowel edema.
5-6 Esophagus with eosinophilic infiltrations
7-8 Cecum and descending colon with eosinophilic infiltrations
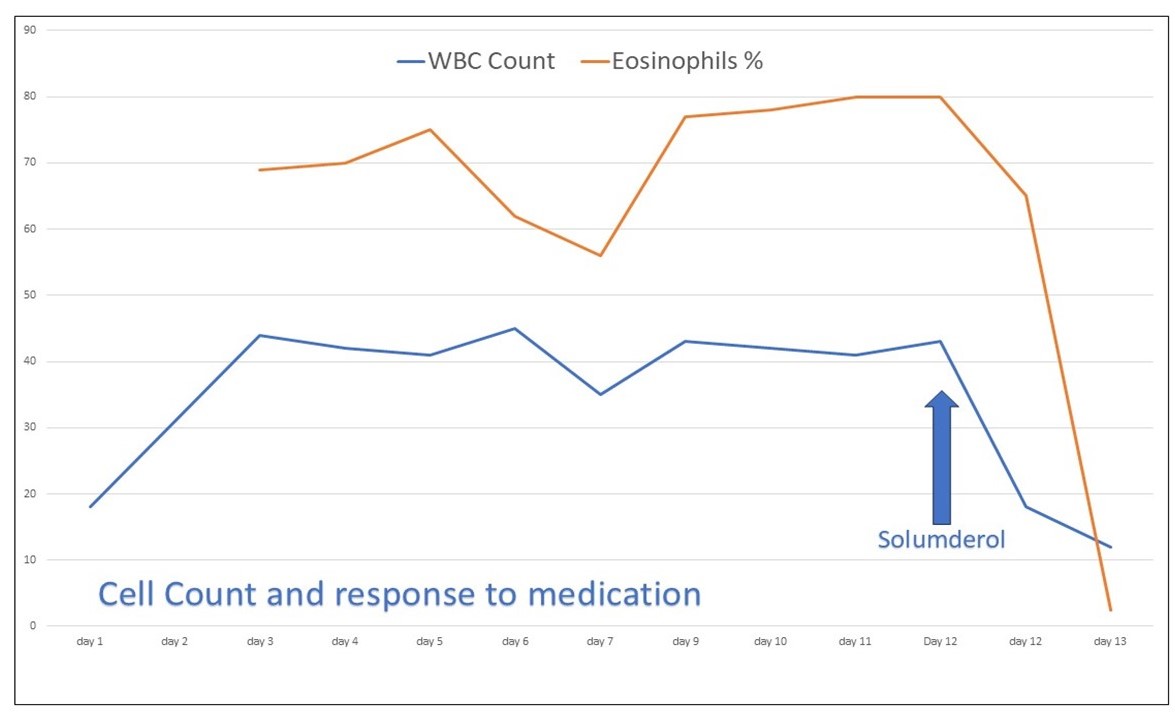
Figure: Dramatic response to Steroid
Disclosures:
Jowana Saba indicated no relevant financial relationships.
Mohamad Altabaa indicated no relevant financial relationships.
Arman Vaghefi indicated no relevant financial relationships.
Marcial Ruiz indicated no relevant financial relationships.
Houssam Kharrat indicated no relevant financial relationships.
Jowana Saba, MD1, Mohamad Altabaa, MBA1, Arman Vaghefi, BS2, Marcial Ruiz, 3, Houssam Kharrat, MD4. P3011 - Beyond the Bloodstream: Gastrointestinal Involvement in Idiopathic Hyper-Eosinophilic Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
