Monday Poster Session
Category: General Endoscopy
P2996 - Endoscopic versus Surgical Resection of Duodenal Neuroendocrine Tumors: Systematic Review and Meta-Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- TA
Tareq Alsaleh, MD
Department of Internal Medicine, AdventHealth Orlando
Orlando, FL
Presenting Author(s)
Abdul Mohammed, MD1, Tareq Alsaleh, MD2, Magda Elamin, MD2, Ernesto Robalino. Gonzaga, MD1, John George, MD1
1Department of Gastroenterology and Hepatology, AdventHealth Orlando, Orlando, FL; 2Department of Internal Medicine, AdventHealth Orlando, Orlando, FL
Introduction: Duodenal neuroendocrine tumors (DNETs) are rare lesions with rising incidence due to increased endoscopic detection. Endoscopic resection (ER) offers a less invasive approach but is technically challenging due to the duodenum’s thin wall and high perforation risk. Surgical resection (SR) remains the standard for tumors >20 mm. Current guidelines favor ER for tumors < 10 mm, yet the optimal strategy for intermediate-sized DNETs (10–20 mm) remains uncertain. We conducted a systematic review and meta-analysis to compare outcomes, safety, and survival between ER and SR for DNETs.
Methods: A comprehensive search of MEDLINE, EMBASE, and Scopus was performed through April 2025 to identify studies comparing ER and SR for DNETs. Outcomes assessed included rates of R0 and R1 resection, overall survival, recurrence, and complications. Pooled effect estimates were calculated using a random-effects model and expressed as odds ratios (OR) or hazard ratios (HR) with 95% confidence intervals (CI). Heterogeneity was evaluated using the I² statistic.
Results: Six retrospective studies involving 1276 patients, of which 51.6% were males, were included: 827 underwent ER and 449 underwent SR. Five studies were multicenter, while one was single center. Median study follow up ranged from 28 months to 95.7 months (Table 1).
ER was associated with significantly lower odds of R0 resection (OR 0.10; 95% CI 0.05–0.20; P < 0.01) and higher odds of R1 resection (OR 4.00; 95% CI 2.04–7.82; P < 0.01). There was no significant difference in overall survival between the groups (HR 0.92; 95% CI 0.45–1.91; P = 0.83). Recurrence rates were also similar (OR 0.47; 95% CI 0.03–8.49; P = 0.61). While not statistically significant, there was a trend toward fewer complications in the ER group (OR 0.18; 95% CI 0.02–1.63; P = 0.13).
Discussion: Endoscopic resection appears to be a safe and less invasive alternative to surgery for DNETs, with comparable survival and recurrence outcomes. However, ER is associated with a higher rate of positive margins, which may necessitate additional treatments or closer follow-up. These findings highlight the need for prospective, well-powered studies specifically targeting DNETs between 10–20 mm to guide optimal management and refine selection criteria for ER versus SR.
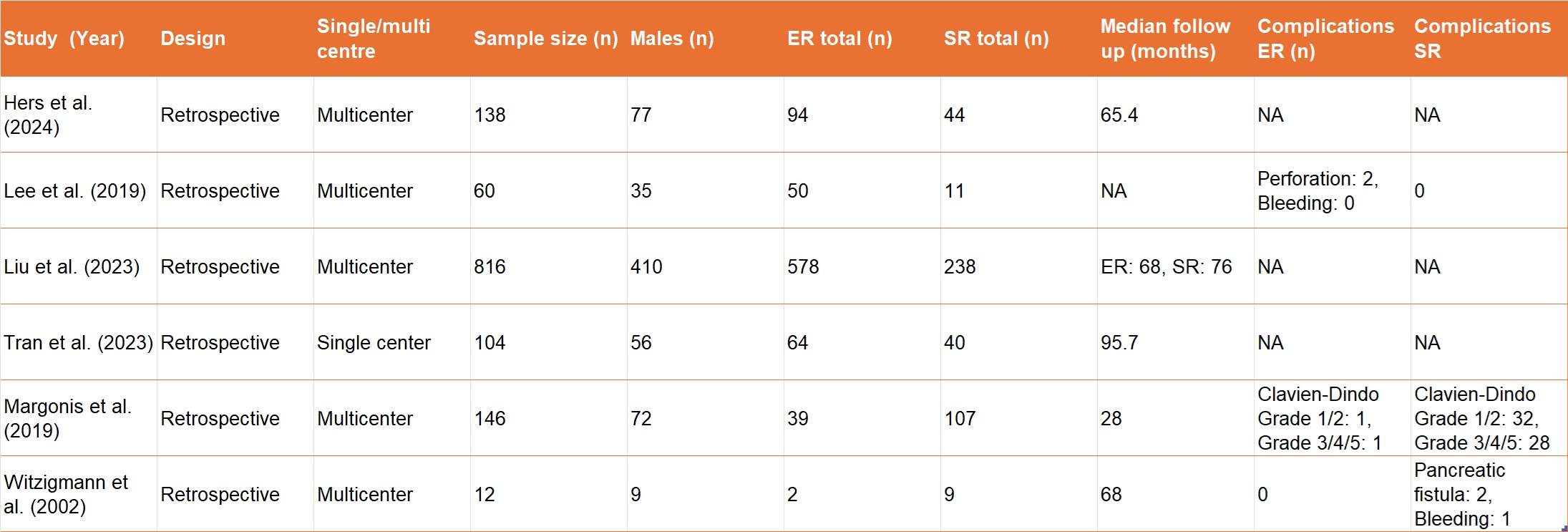
Figure: Table 1. Baseline characteristics of included studies
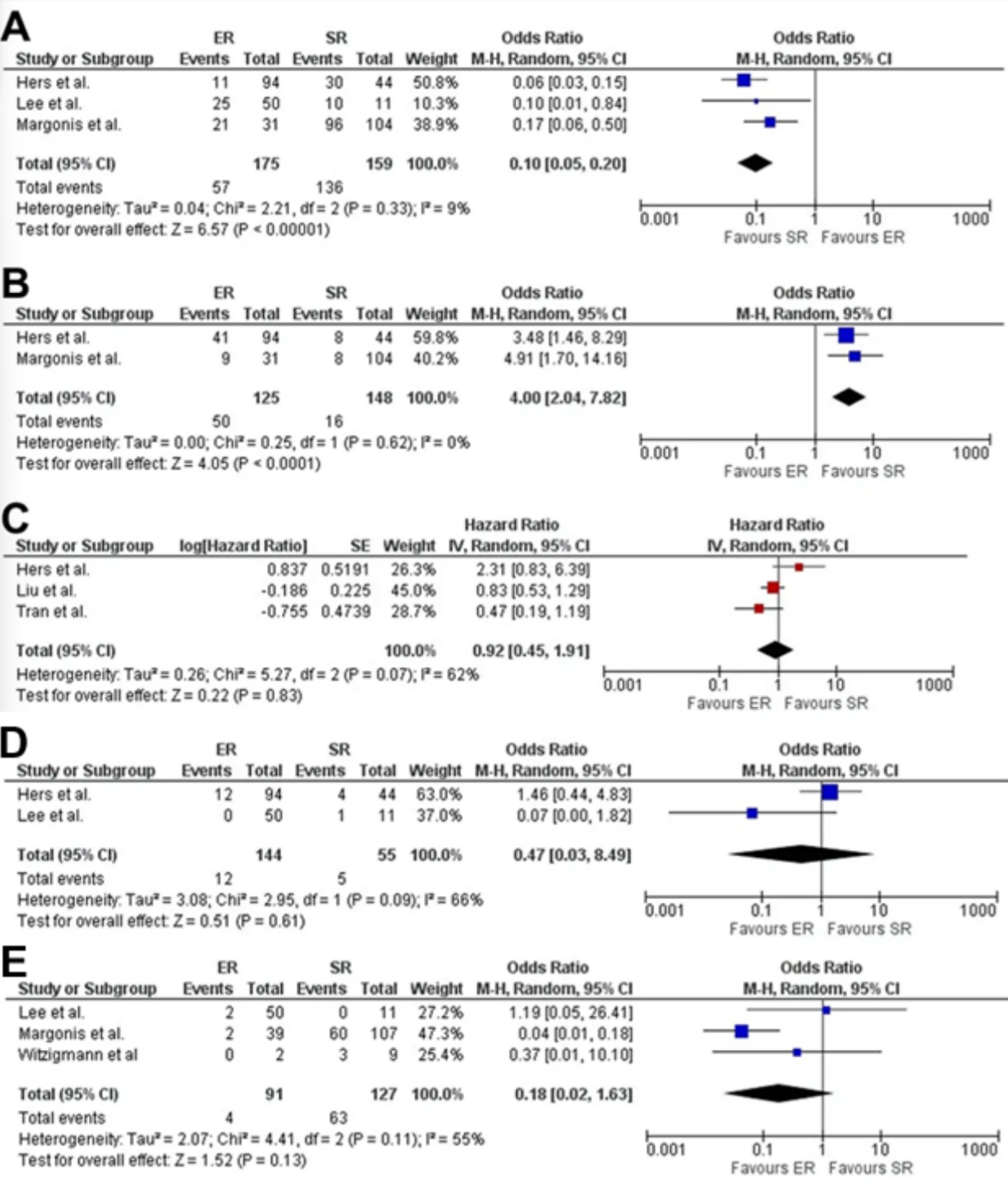
Figure: Figure 2. Pooled odds ratios (OR)/Hazards ratio(HR) of: A – R0 resection; B – R1 resection; C – Overall survival D – Recurrence; E – Complications;
Disclosures:
Abdul Mohammed indicated no relevant financial relationships.
Tareq Alsaleh indicated no relevant financial relationships.
Magda Elamin indicated no relevant financial relationships.
Ernesto Gonzaga indicated no relevant financial relationships.
John George indicated no relevant financial relationships.
Abdul Mohammed, MD1, Tareq Alsaleh, MD2, Magda Elamin, MD2, Ernesto Robalino. Gonzaga, MD1, John George, MD1. P2996 - Endoscopic versus Surgical Resection of Duodenal Neuroendocrine Tumors: Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Department of Gastroenterology and Hepatology, AdventHealth Orlando, Orlando, FL; 2Department of Internal Medicine, AdventHealth Orlando, Orlando, FL
Introduction: Duodenal neuroendocrine tumors (DNETs) are rare lesions with rising incidence due to increased endoscopic detection. Endoscopic resection (ER) offers a less invasive approach but is technically challenging due to the duodenum’s thin wall and high perforation risk. Surgical resection (SR) remains the standard for tumors >20 mm. Current guidelines favor ER for tumors < 10 mm, yet the optimal strategy for intermediate-sized DNETs (10–20 mm) remains uncertain. We conducted a systematic review and meta-analysis to compare outcomes, safety, and survival between ER and SR for DNETs.
Methods: A comprehensive search of MEDLINE, EMBASE, and Scopus was performed through April 2025 to identify studies comparing ER and SR for DNETs. Outcomes assessed included rates of R0 and R1 resection, overall survival, recurrence, and complications. Pooled effect estimates were calculated using a random-effects model and expressed as odds ratios (OR) or hazard ratios (HR) with 95% confidence intervals (CI). Heterogeneity was evaluated using the I² statistic.
Results: Six retrospective studies involving 1276 patients, of which 51.6% were males, were included: 827 underwent ER and 449 underwent SR. Five studies were multicenter, while one was single center. Median study follow up ranged from 28 months to 95.7 months (Table 1).
ER was associated with significantly lower odds of R0 resection (OR 0.10; 95% CI 0.05–0.20; P < 0.01) and higher odds of R1 resection (OR 4.00; 95% CI 2.04–7.82; P < 0.01). There was no significant difference in overall survival between the groups (HR 0.92; 95% CI 0.45–1.91; P = 0.83). Recurrence rates were also similar (OR 0.47; 95% CI 0.03–8.49; P = 0.61). While not statistically significant, there was a trend toward fewer complications in the ER group (OR 0.18; 95% CI 0.02–1.63; P = 0.13).
Discussion: Endoscopic resection appears to be a safe and less invasive alternative to surgery for DNETs, with comparable survival and recurrence outcomes. However, ER is associated with a higher rate of positive margins, which may necessitate additional treatments or closer follow-up. These findings highlight the need for prospective, well-powered studies specifically targeting DNETs between 10–20 mm to guide optimal management and refine selection criteria for ER versus SR.
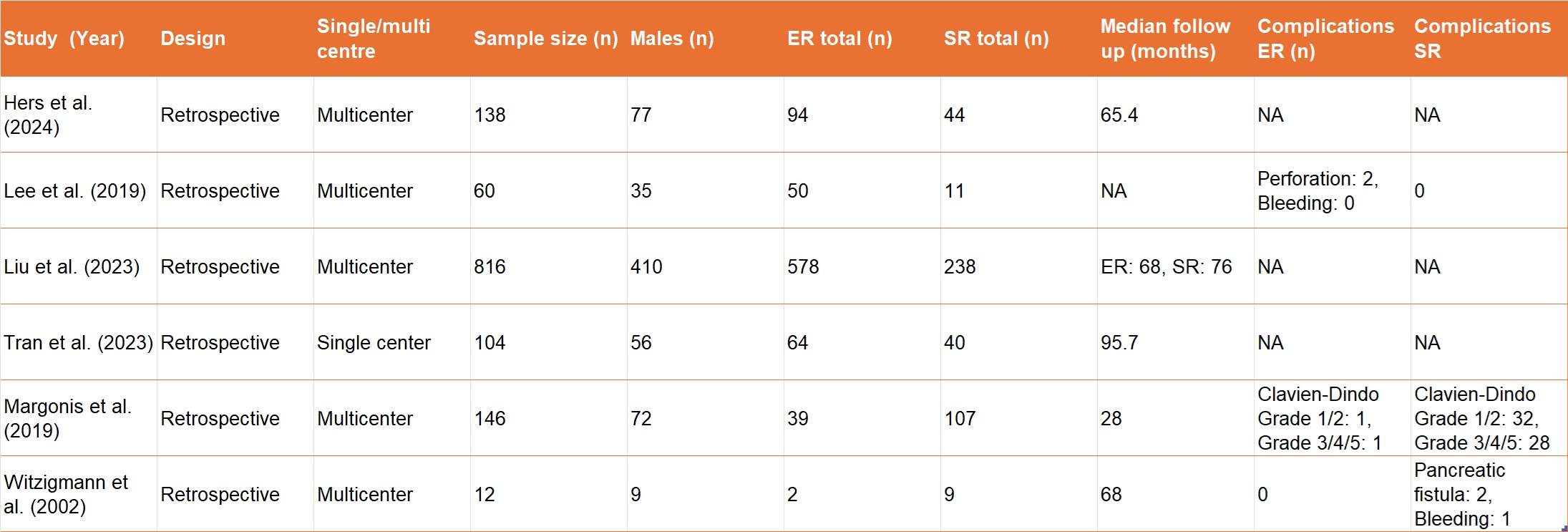
Figure: Table 1. Baseline characteristics of included studies
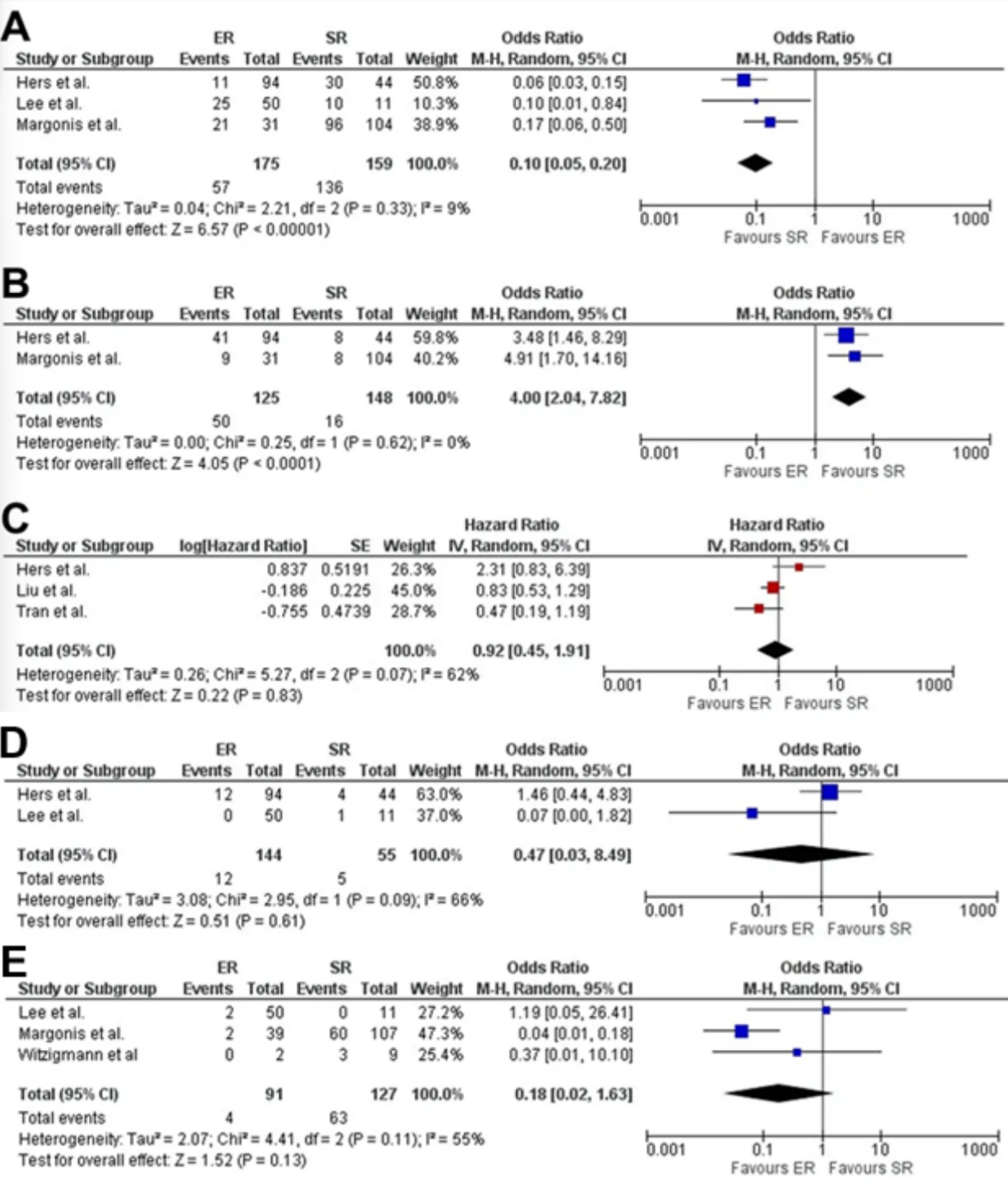
Figure: Figure 2. Pooled odds ratios (OR)/Hazards ratio(HR) of: A – R0 resection; B – R1 resection; C – Overall survival D – Recurrence; E – Complications;
Disclosures:
Abdul Mohammed indicated no relevant financial relationships.
Tareq Alsaleh indicated no relevant financial relationships.
Magda Elamin indicated no relevant financial relationships.
Ernesto Gonzaga indicated no relevant financial relationships.
John George indicated no relevant financial relationships.
Abdul Mohammed, MD1, Tareq Alsaleh, MD2, Magda Elamin, MD2, Ernesto Robalino. Gonzaga, MD1, John George, MD1. P2996 - Endoscopic versus Surgical Resection of Duodenal Neuroendocrine Tumors: Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
