Monday Poster Session
Category: Functional Bowel Disease
P2951 - Predictors of Improvement Among Patients With Disorders of Gut-Brain Interaction in a Virtual Multidisciplinary Care Model
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- MB
Madeline Berschback, MD (she/her/hers)
Massachusetts General Hospital
Boston, MA
Presenting Author(s)
Madeline Berschback, MD1, Treta Purohit, MD, MPH2, Sanskriti Varma, MD1, Sameer Berry, MD3, Ketan Patel, 4, Kyle Staller, MD, MPH1
1Massachusetts General Hospital, Boston, MA; 2Oshi Health, Saratoga, CA; 3NYU Langone Health, New York, NY; 4Oshi Health, Chicago, IL
Introduction: Disorders of gut-brain interaction (DGBI) such as IBS require multifaceted care including pharmacologic, dietary, and behavioral interventions. Traditional in-person care models can fall short in delivering comprehensive support. While digital delivery of gut-brain therapies is promising, real world data evaluating predictors of response across these modalities remains limited.
Methods: We conducted a retrospective cohort study of adult patients (≥18 years) with confirmed DGBI diagnoses who enrolled in a virtual care program (Oshi Health) including services from GI providers, registered dietitians (RD), and behavioral health (BH). As part of the program, patients engaged with a GI APP who designed an individualized care plan. We analyzed demographic and clinical characteristics, including baseline symptom burden, diagnosis, and care components received. Patient-reported outcomes on symptom severity and improvement were collected through in-program surveys. Multivariable logistic regression identified predictors of clinical improvement, defined as self-reported symptom improvement or resolution.
Results: From January 2023 to May 2025, a total of 4,818 patients were evaluated; 3,485 (72%) engaged with multidisciplinary care. The mean age of the cohort was 43.3, most patients were female (70.5%), and IBS was the most common diagnosis (93.7% with any subtype). Participant characteristics are included in Table 1 and patient flow in Figure 1. Overall, 81.2% of patients achieved symptom improvement over an average of 1.2 months. In unadjusted analysis, patients prescribed any neuromodulator had 1.73 greater odds of symptom improvement compared to those not prescribed a neuromodulator. This relationship was no longer significant after multivariable adjustment (OR 1.56, CI 0.95-2.57). Among patients who received neuromodulators, higher numbers of GI, RD, and BH visits were associated with greater odds of improvement per visit (OR 1.4, 1.9, 2.2 respectively; all p< 0.05).
Discussion: This study characterizes the real-world application of a virtual care model and identifies patient-level predictors associated with clinical improvement and treatment response. These findings may inform tailored care pathways and help target which patients are most likely to benefit from specific interventions. Further analysis is planned to better delineate factors associated with overall clinical improvement, neuromodulator initiation, and treatment response patterns.
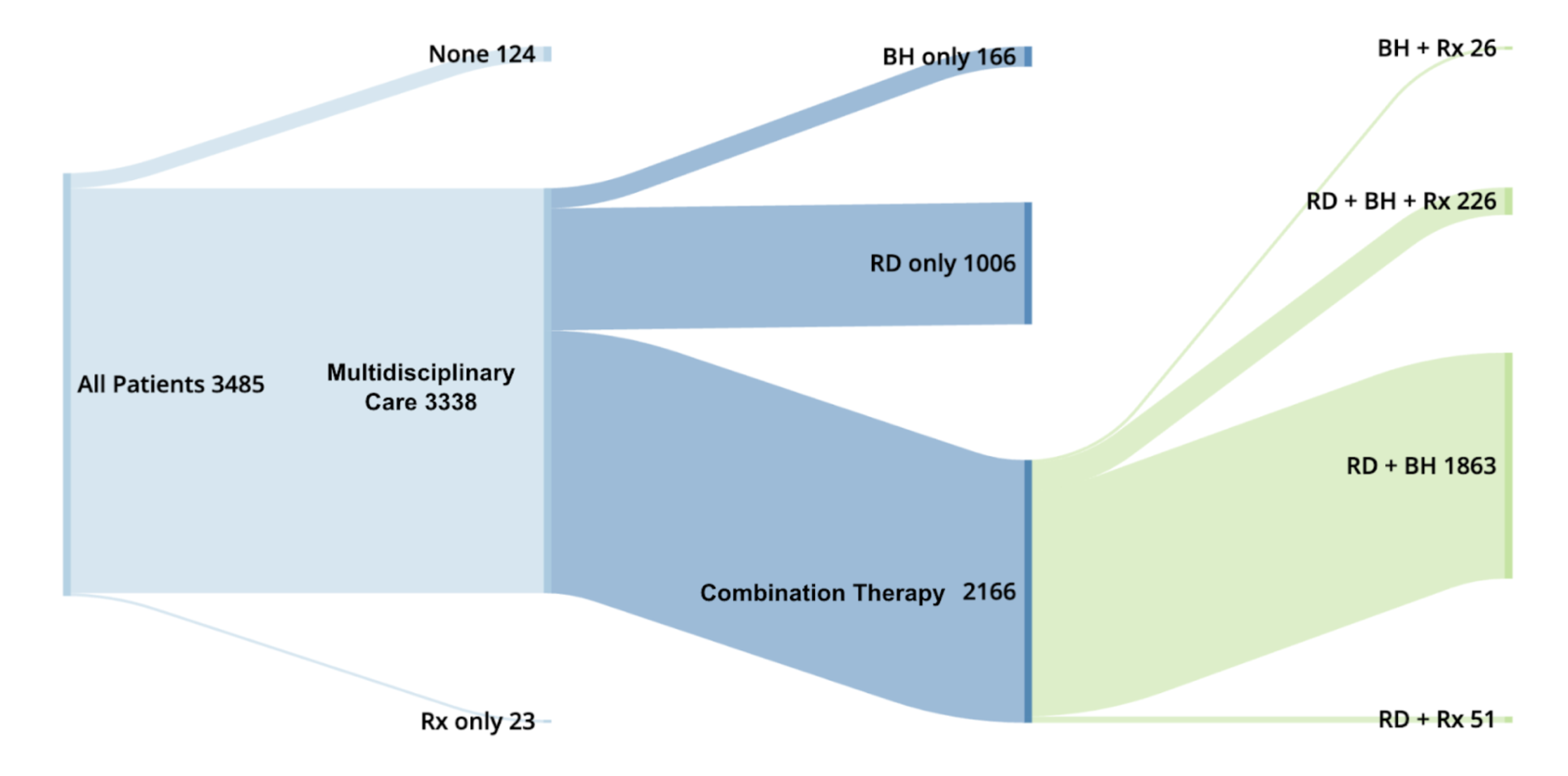
Figure: Table 1: Participant Characteristics
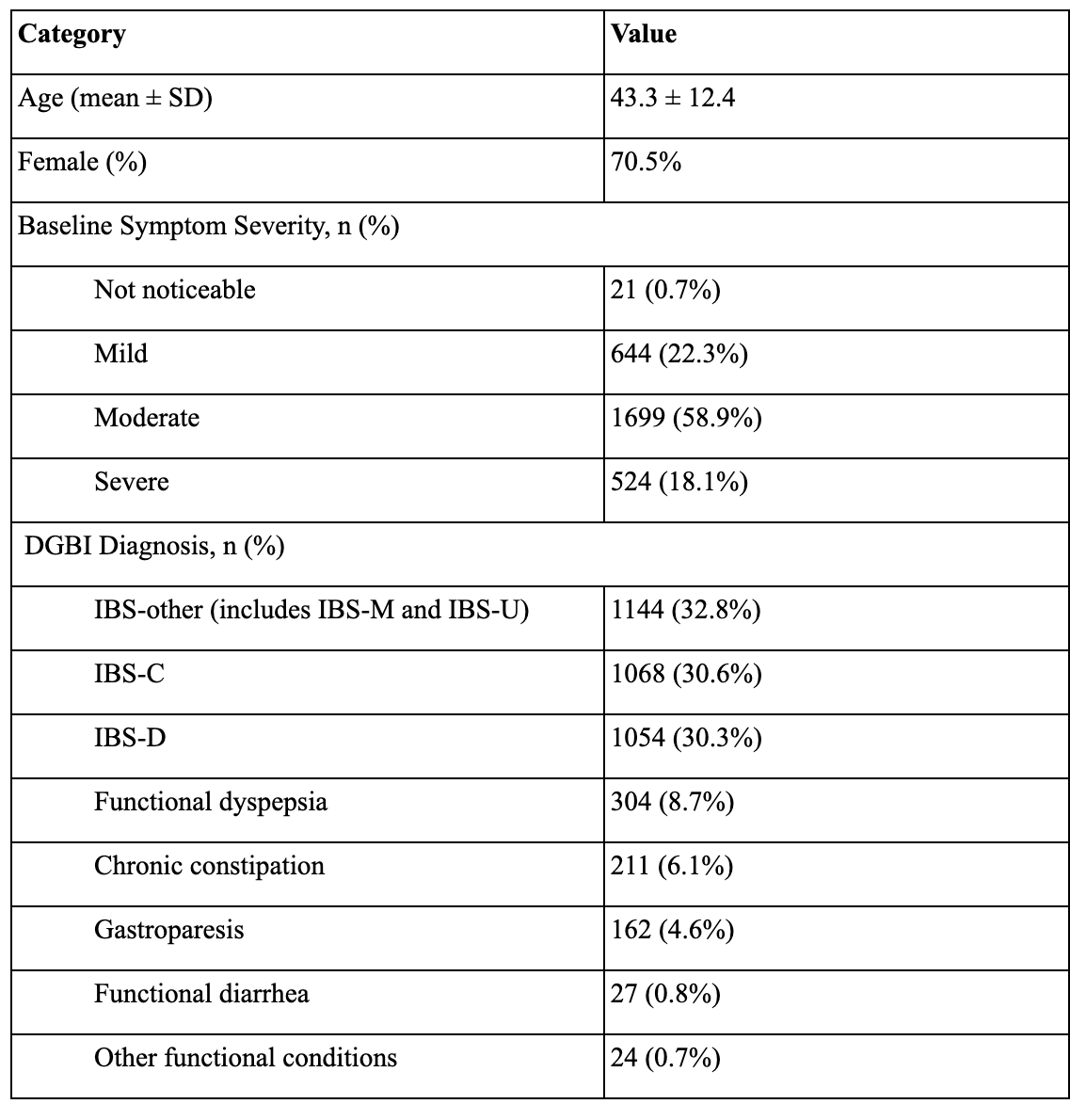
Figure: Figure 1: Distribution of Care Modalities Received by Patients
BH only = behavioral health visit alone. RD only = registered dietitian visit alone. Rx only= only neuromodulator prescribed.
Disclosures:
Madeline Berschback indicated no relevant financial relationships.
Treta Purohit indicated no relevant financial relationships.
Sanskriti Varma: Oshi Health – Consultant.
Sameer Berry: Oshi Health – Employee.
Ketan Patel indicated no relevant financial relationships.
Kyle Staller: Ardelyx – Grant/Research Support. Gemelli – Consultant. Laborie – Consultant. Mahana – Consultant. Salix – Consultant. Takeda – Expert witness.
Madeline Berschback, MD1, Treta Purohit, MD, MPH2, Sanskriti Varma, MD1, Sameer Berry, MD3, Ketan Patel, 4, Kyle Staller, MD, MPH1. P2951 - Predictors of Improvement Among Patients With Disorders of Gut-Brain Interaction in a Virtual Multidisciplinary Care Model, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Massachusetts General Hospital, Boston, MA; 2Oshi Health, Saratoga, CA; 3NYU Langone Health, New York, NY; 4Oshi Health, Chicago, IL
Introduction: Disorders of gut-brain interaction (DGBI) such as IBS require multifaceted care including pharmacologic, dietary, and behavioral interventions. Traditional in-person care models can fall short in delivering comprehensive support. While digital delivery of gut-brain therapies is promising, real world data evaluating predictors of response across these modalities remains limited.
Methods: We conducted a retrospective cohort study of adult patients (≥18 years) with confirmed DGBI diagnoses who enrolled in a virtual care program (Oshi Health) including services from GI providers, registered dietitians (RD), and behavioral health (BH). As part of the program, patients engaged with a GI APP who designed an individualized care plan. We analyzed demographic and clinical characteristics, including baseline symptom burden, diagnosis, and care components received. Patient-reported outcomes on symptom severity and improvement were collected through in-program surveys. Multivariable logistic regression identified predictors of clinical improvement, defined as self-reported symptom improvement or resolution.
Results: From January 2023 to May 2025, a total of 4,818 patients were evaluated; 3,485 (72%) engaged with multidisciplinary care. The mean age of the cohort was 43.3, most patients were female (70.5%), and IBS was the most common diagnosis (93.7% with any subtype). Participant characteristics are included in Table 1 and patient flow in Figure 1. Overall, 81.2% of patients achieved symptom improvement over an average of 1.2 months. In unadjusted analysis, patients prescribed any neuromodulator had 1.73 greater odds of symptom improvement compared to those not prescribed a neuromodulator. This relationship was no longer significant after multivariable adjustment (OR 1.56, CI 0.95-2.57). Among patients who received neuromodulators, higher numbers of GI, RD, and BH visits were associated with greater odds of improvement per visit (OR 1.4, 1.9, 2.2 respectively; all p< 0.05).
Discussion: This study characterizes the real-world application of a virtual care model and identifies patient-level predictors associated with clinical improvement and treatment response. These findings may inform tailored care pathways and help target which patients are most likely to benefit from specific interventions. Further analysis is planned to better delineate factors associated with overall clinical improvement, neuromodulator initiation, and treatment response patterns.
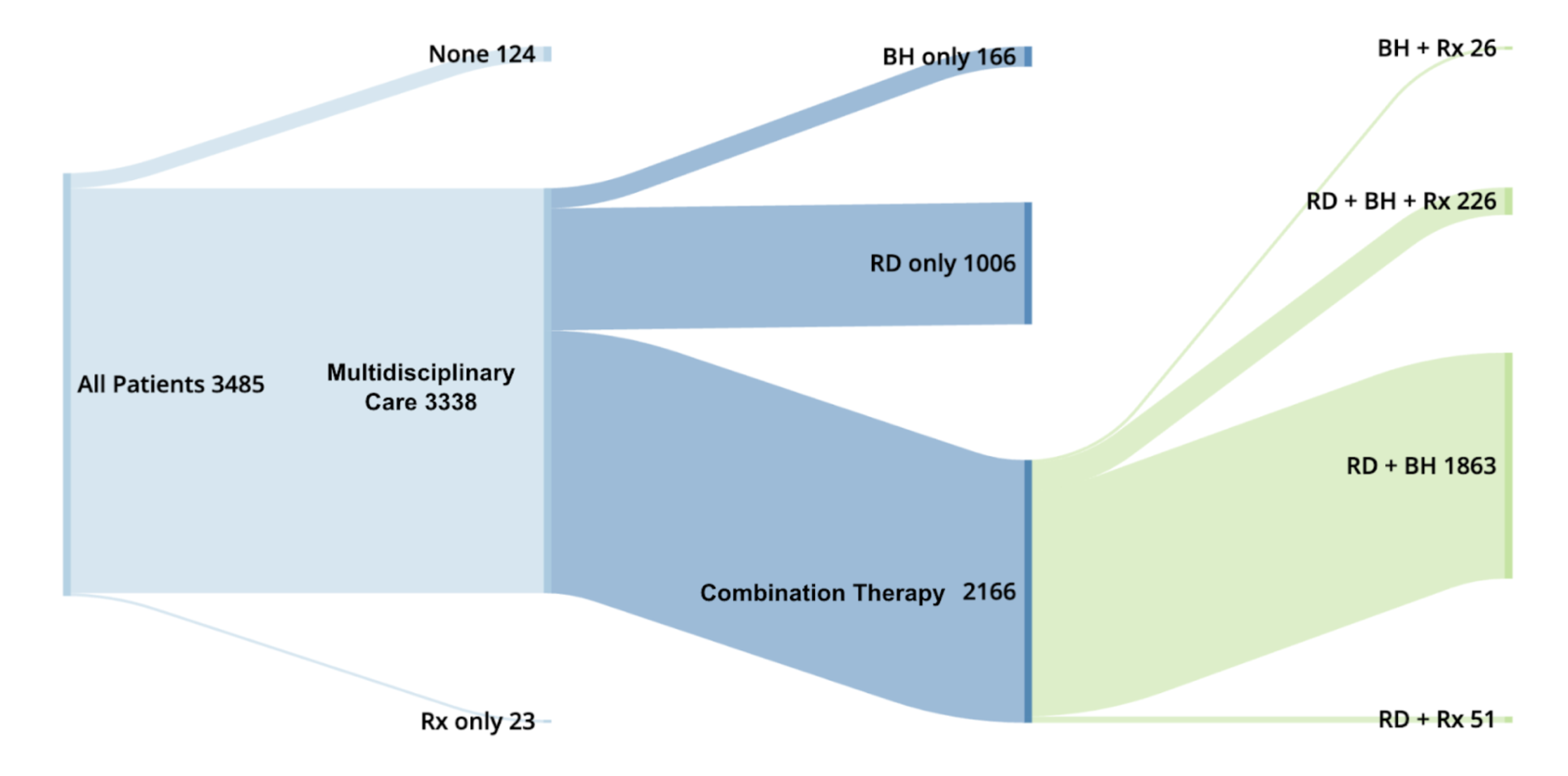
Figure: Table 1: Participant Characteristics
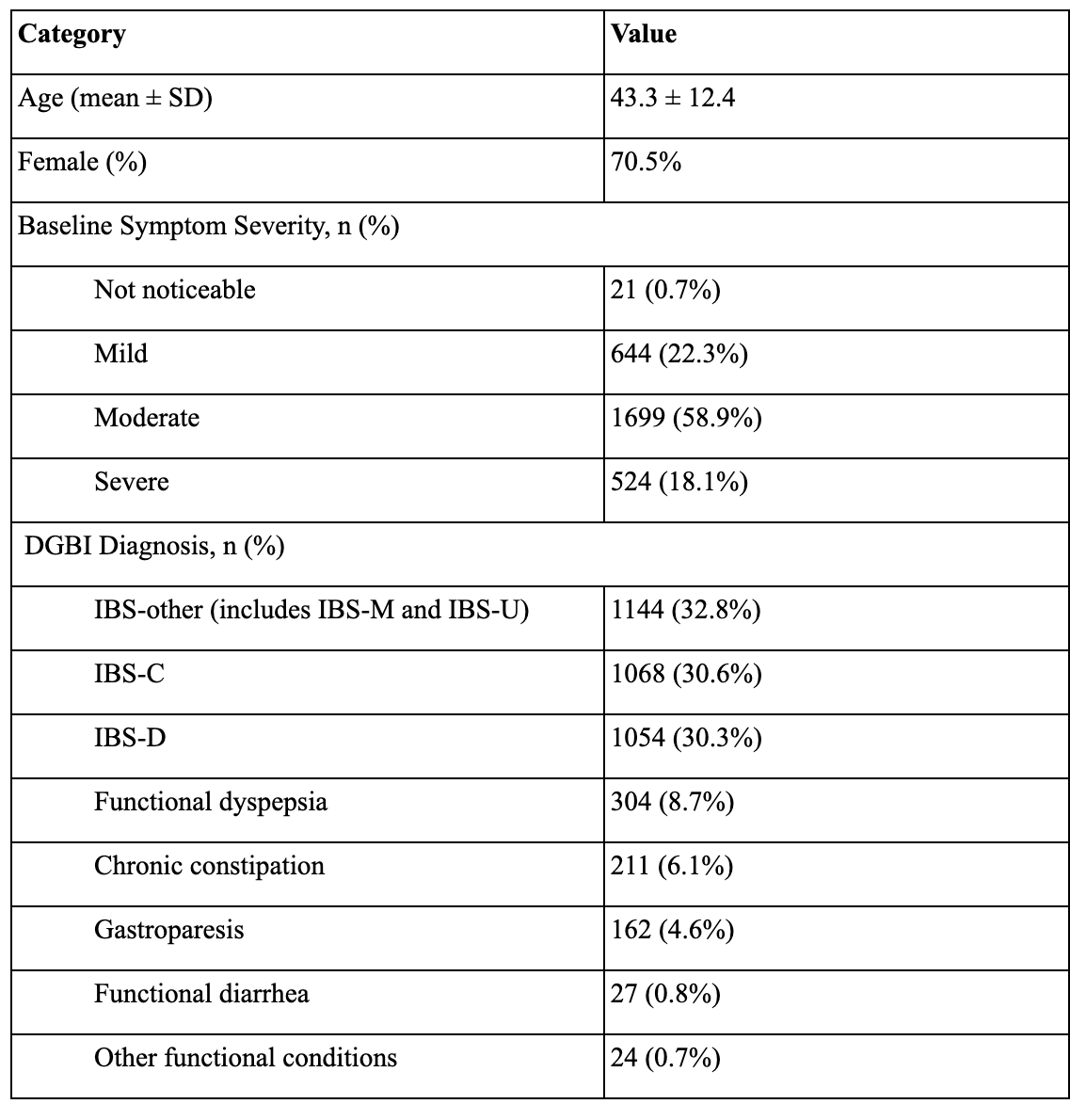
Figure: Figure 1: Distribution of Care Modalities Received by Patients
BH only = behavioral health visit alone. RD only = registered dietitian visit alone. Rx only= only neuromodulator prescribed.
Disclosures:
Madeline Berschback indicated no relevant financial relationships.
Treta Purohit indicated no relevant financial relationships.
Sanskriti Varma: Oshi Health – Consultant.
Sameer Berry: Oshi Health – Employee.
Ketan Patel indicated no relevant financial relationships.
Kyle Staller: Ardelyx – Grant/Research Support. Gemelli – Consultant. Laborie – Consultant. Mahana – Consultant. Salix – Consultant. Takeda – Expert witness.
Madeline Berschback, MD1, Treta Purohit, MD, MPH2, Sanskriti Varma, MD1, Sameer Berry, MD3, Ketan Patel, 4, Kyle Staller, MD, MPH1. P2951 - Predictors of Improvement Among Patients With Disorders of Gut-Brain Interaction in a Virtual Multidisciplinary Care Model, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
