Monday Poster Session
Category: Functional Bowel Disease
P2943 - Barriers to Peripherally Acting Mu-Opioid Receptor Antagonist Utilization in Opioid-Induced Constipation: Patient and Provider Perspectives
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Ariana Chen, BS (she/her/hers)
University of Michigan Medical School
Ann Arbor, MI
Presenting Author(s)
Ariana Chen, BS1, Katie Liu, MD2, Prashant Singh, MD1, Allen Lee, MD, MS1
1University of Michigan Medical School, Ann Arbor, MI; 2University of Michigan, Ann Arbor, MI
Introduction: Peripherally acting mu-opioid receptor antagonists (PAMORAs) are recommended in patients with opioid-induced constipation (OIC) who have suboptimal symptom control after an adequate trial of first-line laxatives. We aim to understand the barriers to PAMORA utilization from both patient and provider perspectives.
Methods: We conducted anonymous online surveys of patients with OIC (defined as new or worsening constipation after starting opioid medications) and providers who care for patients with OIC at a single large academic center from March to May 2025.
Results: Of 172 patients (mean age 39.7 years, 52% male) who responded, 73% (n=125) had discussed PAMORAs with their providers, with 87% (n=109) of those having been prescribed a PAMORA. A vast majority of respondents reported attending 7-10 healthcare visits specifically to discuss OIC-related concerns and identified primary care physicians as the most common provider managing their OIC (Figure 1). 80% of patients were satisfied (n=75) or very satisfied (n=11) with the PAMORA they were prescribed. Concern for worsening of pain was the most commonly reported barrier (n=40), followed by concern for side effects (n=38), and concern for interaction with other drugs (n=36). Only 6 respondents selected insurance coverage/out of pocket costs as a barrier.
Of 36 providers who responded (Figure 2), 43% (n=15) did not feel adequately educated on OIC treatment options and were interested in further education. 83% (n=29) of providers knew of PAMORAs; however, 38% (n=11) had never prescribed PAMORAs before. Primary care had the lowest rates of prescribing PAMORAs, with 62% reporting never having prescribed a PAMORA. The most commonly reported barrier to prescribing PAMORAs was high cost and/or insurance coverage (n=17), followed by burdensome prior authorization process (n=11) and limited experience in prescribing PAMORAs (n=10).
Discussion: Patients and providers may have different concerns and perceptions of barriers to utilizing PAMORAs for OIC. While patients perceive their effect on pain to be the most significant barrier in utilizing PAMORAs, providers are most concerned about insurance coverage. Both patients and providers could benefit from further education on PAMORAs, especially in the primary care setting where OIC is most commonly managed but PAMORAs are grossly underutilized.
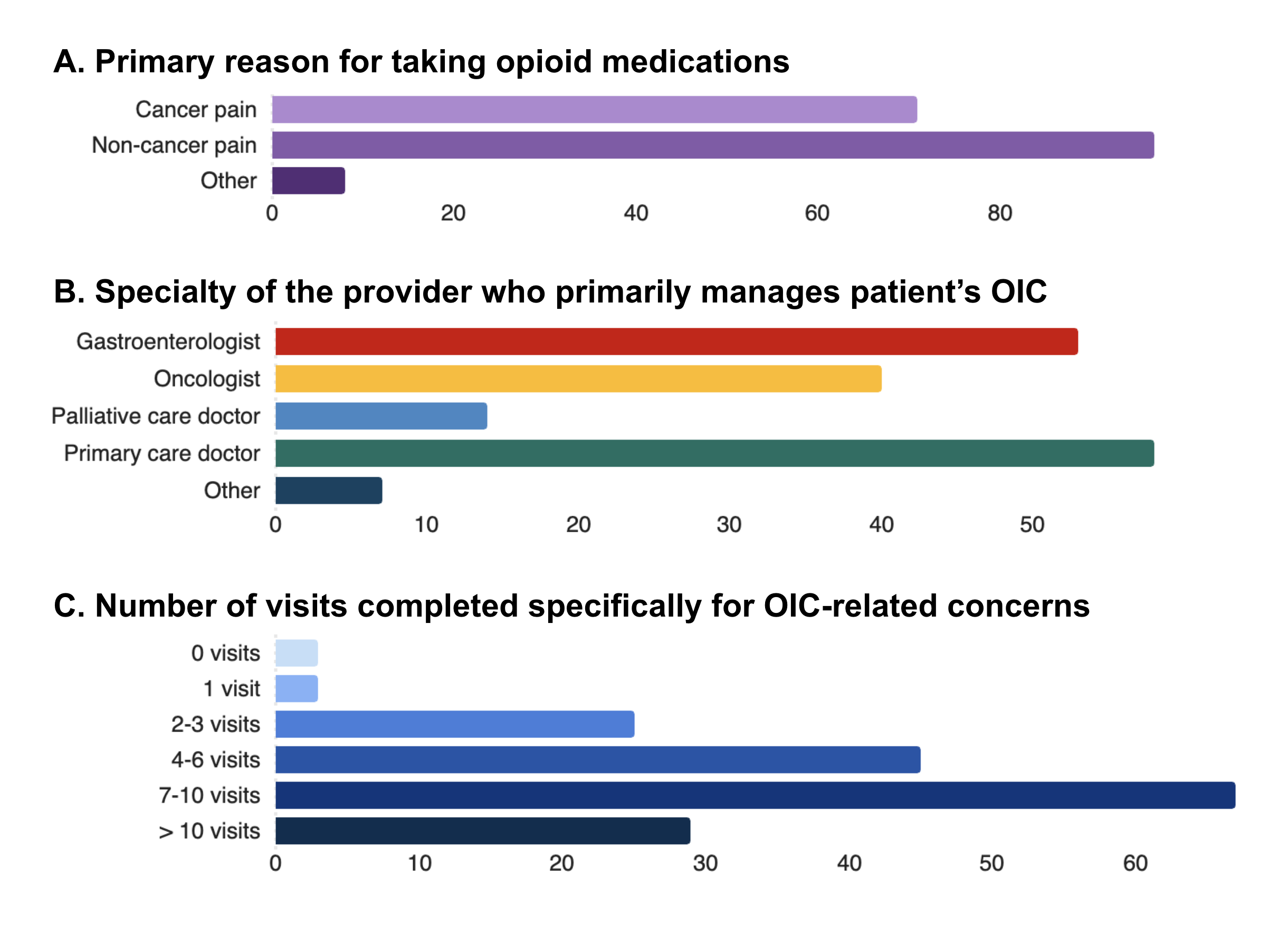
Figure: Figure 1. Patient management characteristics
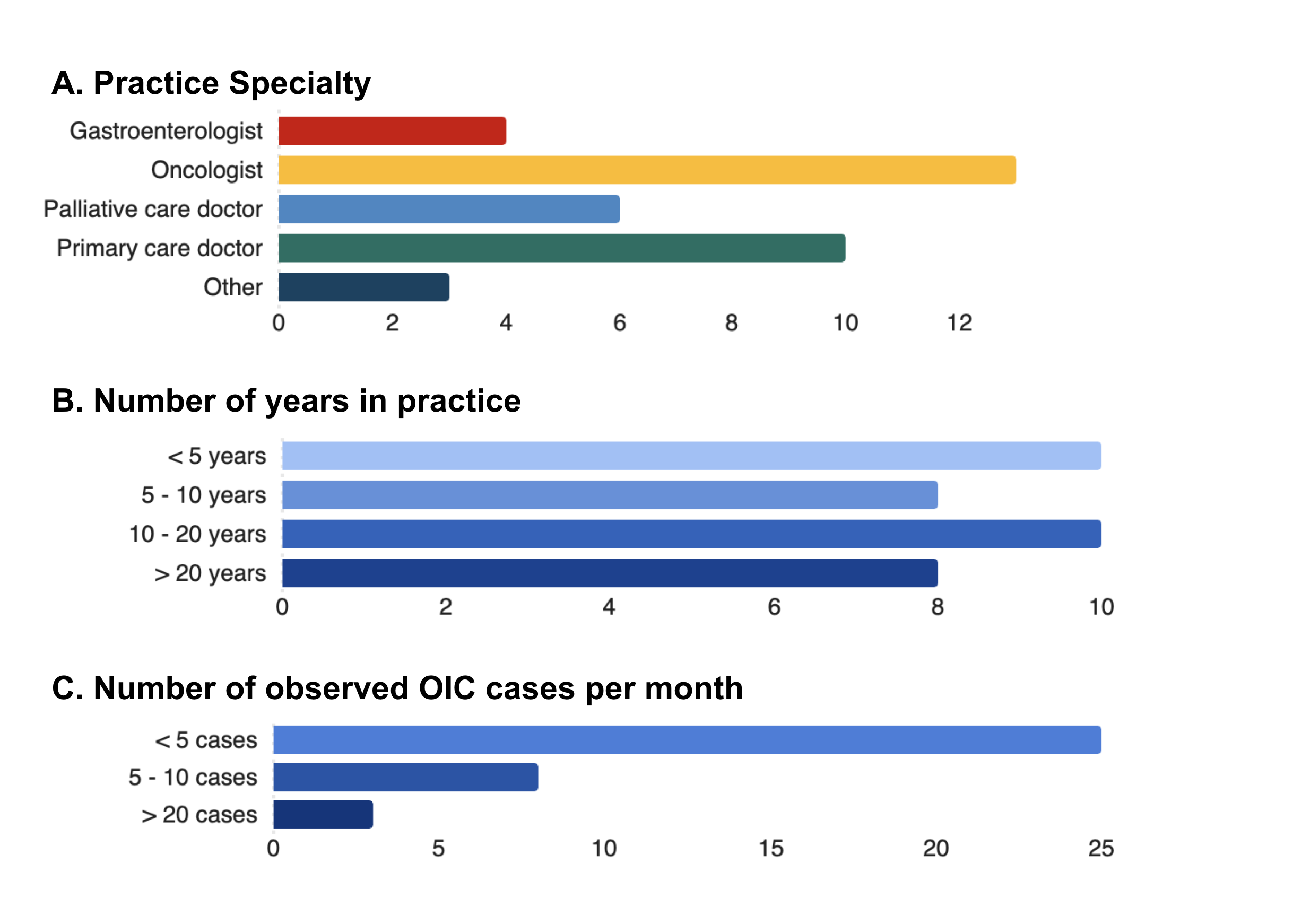
Figure: Figure 2. Provider practice characteristics
Disclosures:
Ariana Chen indicated no relevant financial relationships.
Katie Liu indicated no relevant financial relationships.
Prashant Singh: Uptodate – Royalties.
Allen Lee: Atmo Biosciences – Consultant.
Ariana Chen, BS1, Katie Liu, MD2, Prashant Singh, MD1, Allen Lee, MD, MS1. P2943 - Barriers to Peripherally Acting Mu-Opioid Receptor Antagonist Utilization in Opioid-Induced Constipation: Patient and Provider Perspectives, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Michigan Medical School, Ann Arbor, MI; 2University of Michigan, Ann Arbor, MI
Introduction: Peripherally acting mu-opioid receptor antagonists (PAMORAs) are recommended in patients with opioid-induced constipation (OIC) who have suboptimal symptom control after an adequate trial of first-line laxatives. We aim to understand the barriers to PAMORA utilization from both patient and provider perspectives.
Methods: We conducted anonymous online surveys of patients with OIC (defined as new or worsening constipation after starting opioid medications) and providers who care for patients with OIC at a single large academic center from March to May 2025.
Results: Of 172 patients (mean age 39.7 years, 52% male) who responded, 73% (n=125) had discussed PAMORAs with their providers, with 87% (n=109) of those having been prescribed a PAMORA. A vast majority of respondents reported attending 7-10 healthcare visits specifically to discuss OIC-related concerns and identified primary care physicians as the most common provider managing their OIC (Figure 1). 80% of patients were satisfied (n=75) or very satisfied (n=11) with the PAMORA they were prescribed. Concern for worsening of pain was the most commonly reported barrier (n=40), followed by concern for side effects (n=38), and concern for interaction with other drugs (n=36). Only 6 respondents selected insurance coverage/out of pocket costs as a barrier.
Of 36 providers who responded (Figure 2), 43% (n=15) did not feel adequately educated on OIC treatment options and were interested in further education. 83% (n=29) of providers knew of PAMORAs; however, 38% (n=11) had never prescribed PAMORAs before. Primary care had the lowest rates of prescribing PAMORAs, with 62% reporting never having prescribed a PAMORA. The most commonly reported barrier to prescribing PAMORAs was high cost and/or insurance coverage (n=17), followed by burdensome prior authorization process (n=11) and limited experience in prescribing PAMORAs (n=10).
Discussion: Patients and providers may have different concerns and perceptions of barriers to utilizing PAMORAs for OIC. While patients perceive their effect on pain to be the most significant barrier in utilizing PAMORAs, providers are most concerned about insurance coverage. Both patients and providers could benefit from further education on PAMORAs, especially in the primary care setting where OIC is most commonly managed but PAMORAs are grossly underutilized.
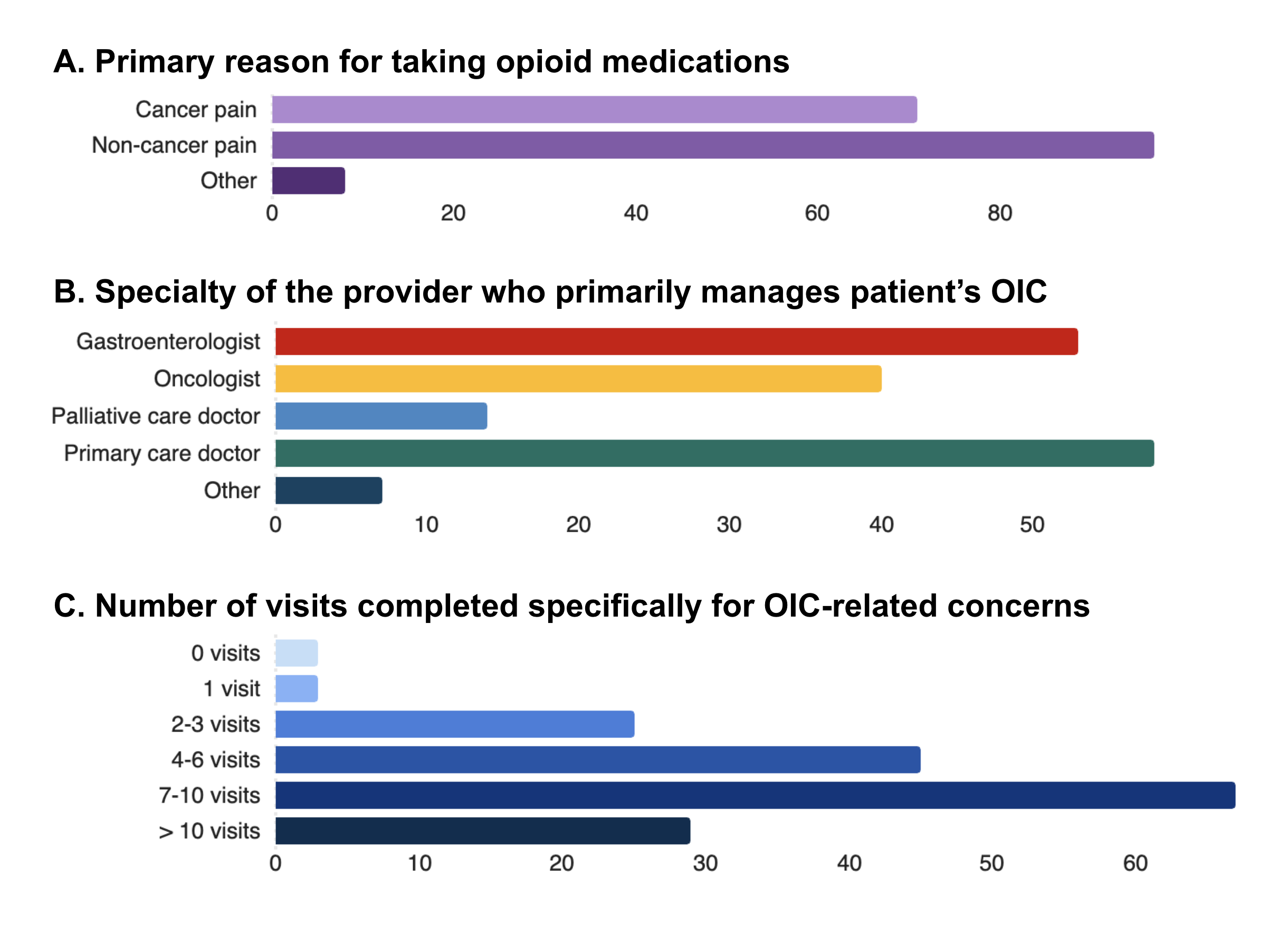
Figure: Figure 1. Patient management characteristics
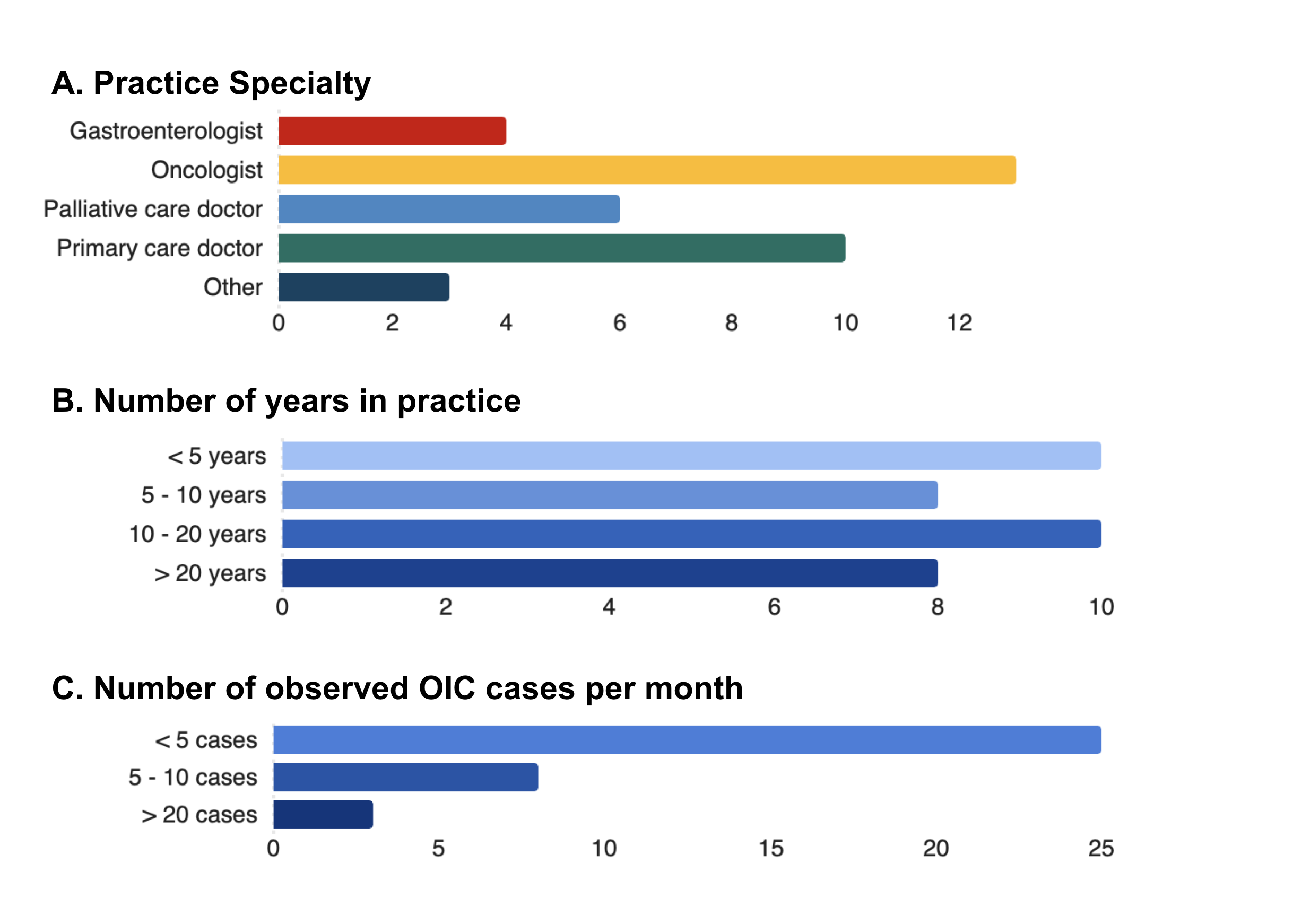
Figure: Figure 2. Provider practice characteristics
Disclosures:
Ariana Chen indicated no relevant financial relationships.
Katie Liu indicated no relevant financial relationships.
Prashant Singh: Uptodate – Royalties.
Allen Lee: Atmo Biosciences – Consultant.
Ariana Chen, BS1, Katie Liu, MD2, Prashant Singh, MD1, Allen Lee, MD, MS1. P2943 - Barriers to Peripherally Acting Mu-Opioid Receptor Antagonist Utilization in Opioid-Induced Constipation: Patient and Provider Perspectives, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
