Monday Poster Session
Category: Functional Bowel Disease
P2939 - Fewer Acute Care and Outpatient Visits With Nasal vs Oral Metoclopramide in Diabetic Gastroparesis: A Real-World Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Pierantonio Russo, MD (he/him/his)
EVERSANA Life Sciences
Overland Park, KY
Presenting Author(s)
Pierantonio Russo, MD1, Ramaa Nathan, PhD2, Priyanka Tripathi, MS2, Michael Cline, DO3, David C. Kunkel, MD4
1EVERSANA Life Sciences, Overland Park, KY; 2EVERSANA Life Sciences, Overland Park, KS; 3Cleveland Clinic, Cleveland, OH; 4University of California San Diego, La Jolla, CA
Introduction: Oral metoclopramide (OMCP) is the primary pharmacologic treatment for gastroparesis (GP), but its effectiveness is often limited in patients with delayed gastric emptying, nausea, and vomiting, which impair gastrointestinal absorption. This is particularly challenging in diabetic gastroparesis (DG), where autonomic dysfunction further complicates gastric transit. An intranasal formulation of metoclopramide (NMCP) bypasses the gastrointestinal tract, potentially offering a more reliable route of administration. This study compares the impact of NMCP versus OMCP on healthcare resource utilization (HCRU) over 12 months in patients with type 2 diabetes (T2D) and GP.
Methods: We conducted a retrospective real-world evidence study using the Symphony Integrated Dataverse administrative claims data (Jan 2020–Feb 2025). Adult patients with T2D and GP who were initiated on either NMCP or OMCP were identified. Patients were considered to have T2D if they had at least one claim for T2D and to have GP if they had a GP diagnosis or had experienced GP symptoms within 12 months prior to treatment initiation. Entropy balancing was applied to adjust for covariates such as age, sex, insurance type, and Elixhauser comorbidity index. HCRU was measured through outpatient visits and acute care episodes, including hospitalizations and emergency room visits. All patients had at least 12 months of baseline data and 12 months of follow-up.
Results: The cohort included 372,700 patients with T2D and GP. Of these, the study cohort included 569 were prescribed NMCP (75% female, median age 57) and 56,900 only OMCP (68% female, median age 58); 56% of NMCP patients were initially on OMCP (Figure 1). Over 12 months, NMCP patients had fewer acute care episodes (924/1,000/year) vs. OMCP (1,313/1,000/year; ratio 0.7, 95% CI 0.67–0.74), lower outpatient visits (5,391 vs. 5,974/1,000/year), and longer median time to hospitalization (12 vs. 7 months; p< 0.01) (Figure 2).
Discussion: This real-world analysis shows that intranasal metoclopramide is associated with lower healthcare resource utilization compared to oral metoclopramide in patients with diabetic gastroparesis. These results suggest that a non-oral treatment option may offer clinical and economic benefits, particularly in patients whose symptoms impair oral drug absorption. Further prospective studies are needed to confirm these findings
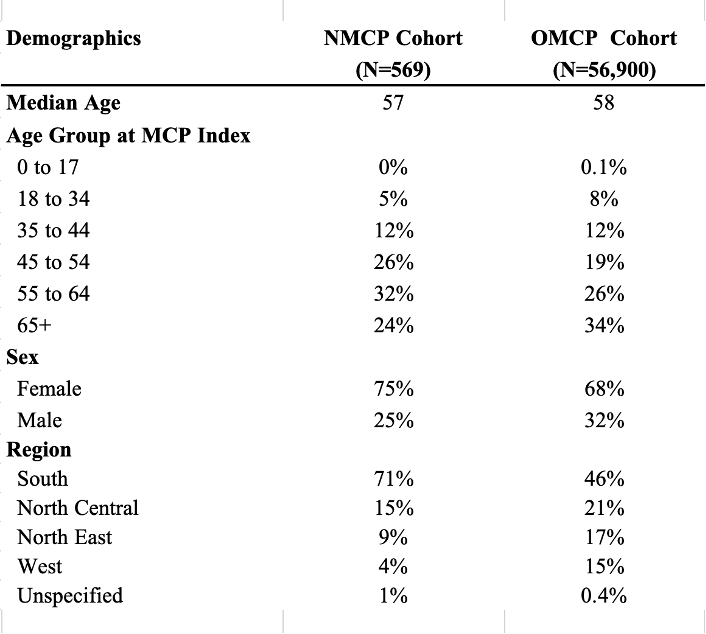
Figure: Demographics of Patients with Type 2 Diabetes (T2D) and Gastroparesis and prescribed Oral or Nasal Metoclopramide

Figure: Time from MCP Initiation to Acute Episode
Disclosures:
Pierantonio Russo indicated no relevant financial relationships.
Ramaa Nathan indicated no relevant financial relationships.
Priyanka Tripathi indicated no relevant financial relationships.
Michael Cline: EVOKE Pharmaceuticals – Key Opinion Leader. Kate Farms – Key Opinion Leader.
David Kunkel: Atmo Biosciences – Grant/Research Support. Gemelli Biotech – Consultant. Phathom Pharmaceuticals – Speakers Bureau. Regeneron Pharmaceuticals – Speakers Bureau. Sanofi – Speakers Bureau. Vanda Pharmaceuticals – Grant/Research Support.
Pierantonio Russo, MD1, Ramaa Nathan, PhD2, Priyanka Tripathi, MS2, Michael Cline, DO3, David C. Kunkel, MD4. P2939 - Fewer Acute Care and Outpatient Visits With Nasal vs Oral Metoclopramide in Diabetic Gastroparesis: A Real-World Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1EVERSANA Life Sciences, Overland Park, KY; 2EVERSANA Life Sciences, Overland Park, KS; 3Cleveland Clinic, Cleveland, OH; 4University of California San Diego, La Jolla, CA
Introduction: Oral metoclopramide (OMCP) is the primary pharmacologic treatment for gastroparesis (GP), but its effectiveness is often limited in patients with delayed gastric emptying, nausea, and vomiting, which impair gastrointestinal absorption. This is particularly challenging in diabetic gastroparesis (DG), where autonomic dysfunction further complicates gastric transit. An intranasal formulation of metoclopramide (NMCP) bypasses the gastrointestinal tract, potentially offering a more reliable route of administration. This study compares the impact of NMCP versus OMCP on healthcare resource utilization (HCRU) over 12 months in patients with type 2 diabetes (T2D) and GP.
Methods: We conducted a retrospective real-world evidence study using the Symphony Integrated Dataverse administrative claims data (Jan 2020–Feb 2025). Adult patients with T2D and GP who were initiated on either NMCP or OMCP were identified. Patients were considered to have T2D if they had at least one claim for T2D and to have GP if they had a GP diagnosis or had experienced GP symptoms within 12 months prior to treatment initiation. Entropy balancing was applied to adjust for covariates such as age, sex, insurance type, and Elixhauser comorbidity index. HCRU was measured through outpatient visits and acute care episodes, including hospitalizations and emergency room visits. All patients had at least 12 months of baseline data and 12 months of follow-up.
Results: The cohort included 372,700 patients with T2D and GP. Of these, the study cohort included 569 were prescribed NMCP (75% female, median age 57) and 56,900 only OMCP (68% female, median age 58); 56% of NMCP patients were initially on OMCP (Figure 1). Over 12 months, NMCP patients had fewer acute care episodes (924/1,000/year) vs. OMCP (1,313/1,000/year; ratio 0.7, 95% CI 0.67–0.74), lower outpatient visits (5,391 vs. 5,974/1,000/year), and longer median time to hospitalization (12 vs. 7 months; p< 0.01) (Figure 2).
Discussion: This real-world analysis shows that intranasal metoclopramide is associated with lower healthcare resource utilization compared to oral metoclopramide in patients with diabetic gastroparesis. These results suggest that a non-oral treatment option may offer clinical and economic benefits, particularly in patients whose symptoms impair oral drug absorption. Further prospective studies are needed to confirm these findings
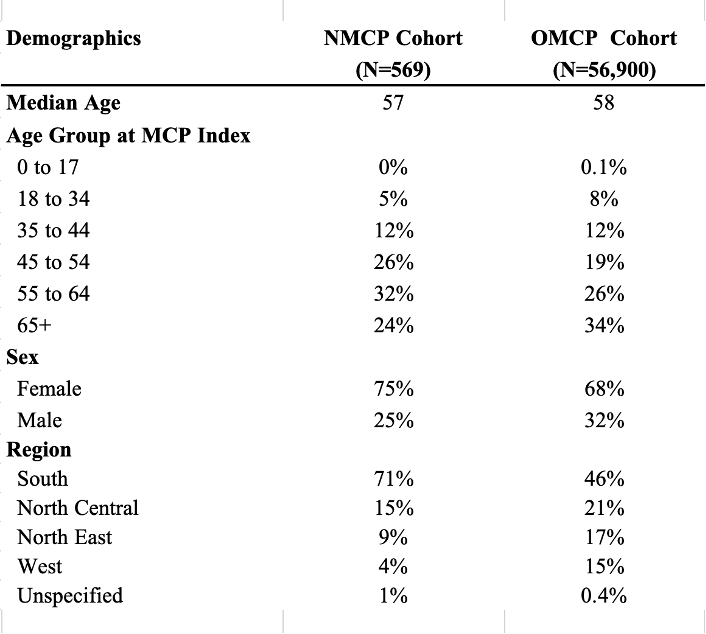
Figure: Demographics of Patients with Type 2 Diabetes (T2D) and Gastroparesis and prescribed Oral or Nasal Metoclopramide

Figure: Time from MCP Initiation to Acute Episode
Disclosures:
Pierantonio Russo indicated no relevant financial relationships.
Ramaa Nathan indicated no relevant financial relationships.
Priyanka Tripathi indicated no relevant financial relationships.
Michael Cline: EVOKE Pharmaceuticals – Key Opinion Leader. Kate Farms – Key Opinion Leader.
David Kunkel: Atmo Biosciences – Grant/Research Support. Gemelli Biotech – Consultant. Phathom Pharmaceuticals – Speakers Bureau. Regeneron Pharmaceuticals – Speakers Bureau. Sanofi – Speakers Bureau. Vanda Pharmaceuticals – Grant/Research Support.
Pierantonio Russo, MD1, Ramaa Nathan, PhD2, Priyanka Tripathi, MS2, Michael Cline, DO3, David C. Kunkel, MD4. P2939 - Fewer Acute Care and Outpatient Visits With Nasal vs Oral Metoclopramide in Diabetic Gastroparesis: A Real-World Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
