Monday Poster Session
Category: Functional Bowel Disease
P2924 - Low Rates of Trauma Screening Prior to Anorectal Manometry Procedures
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Abigail Bacharach, MD
Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Abigail Bacharach, MD1, Yuying Luo, MD2
1Icahn School of Medicine at Mount Sinai, New York, NY; 2Mount Sinai West & Morningside, New York, NY
Introduction: Almost a quarter of patients with defecatory disorders have a history of trauma and report greater distress during gastrointestinal (GI) procedures. Anorectal manometry (ARM) is commonly ordered to assess defecatory disorders and poses a risk for re-traumatization in some patients. Assessing if patients have a trauma history could help reduce this risk and patients with prior trauma think providers should inquire about it. Research is lacking on rates of trauma screening before ARM. We aimed to determine rates of provider screening for trauma history in patients undergoing ARM.
Methods: A retrospective chart review was performed on consecutive patients who underwent ARM at a tertiary academic center over four months. Demographic and clinical factors were collected including age, gender, indication for ARM, and psychiatric comorbidities. Our primary outcome was if trauma screening was performed; secondary outcomes included if screening was positive and the specialty that performed the screening. Descriptive statistics were performed.
Results: Our cohort included 62 patients (72.6% female) with an average age of 53.7 +/- 16.2 years at time of ARM. 58.1% (n=36) of the cohort was non-Hispanic; 53.2% (n=33) identified as white, 11% (n=7) identified as black. The indication for ARM was most commonly constipation (64.5%), followed by incontinence (27.4%). 19 patients (30.6%) were screened for trauma by any provider; GI providers screened only 5 of these patients with other screening performed by various specialties including psychiatry (n=4), medicine (n=4), obstetrics/gynecology (n=4), and colorectal surgery (n=1). Of the 19 patients screened, 7 screened positive for trauma. Trauma screening was never documented by the proceduralist during the consent process on the day of ARM. 16.1% (n=10) of patients had post-traumatic stress disorder, 38.7% (n=24) had major depressive disorder, 45.2% (n=28) had anxiety, and 16.1% (n=10) had an alternate psychiatric diagnosis. There was no statistically significant difference in demographic factors between those who were screened and those who were not.
Discussion: Fewer than one-third of patients were screened for trauma prior to ARM with GI providers performing a minority of the screening. However, of the patients screened, about one-third screened positive for trauma. Further studies are needed on the best method to screen for trauma in the GI clinical setting and how best to train providers on trauma-informed care, especially during vulnerable procedures.
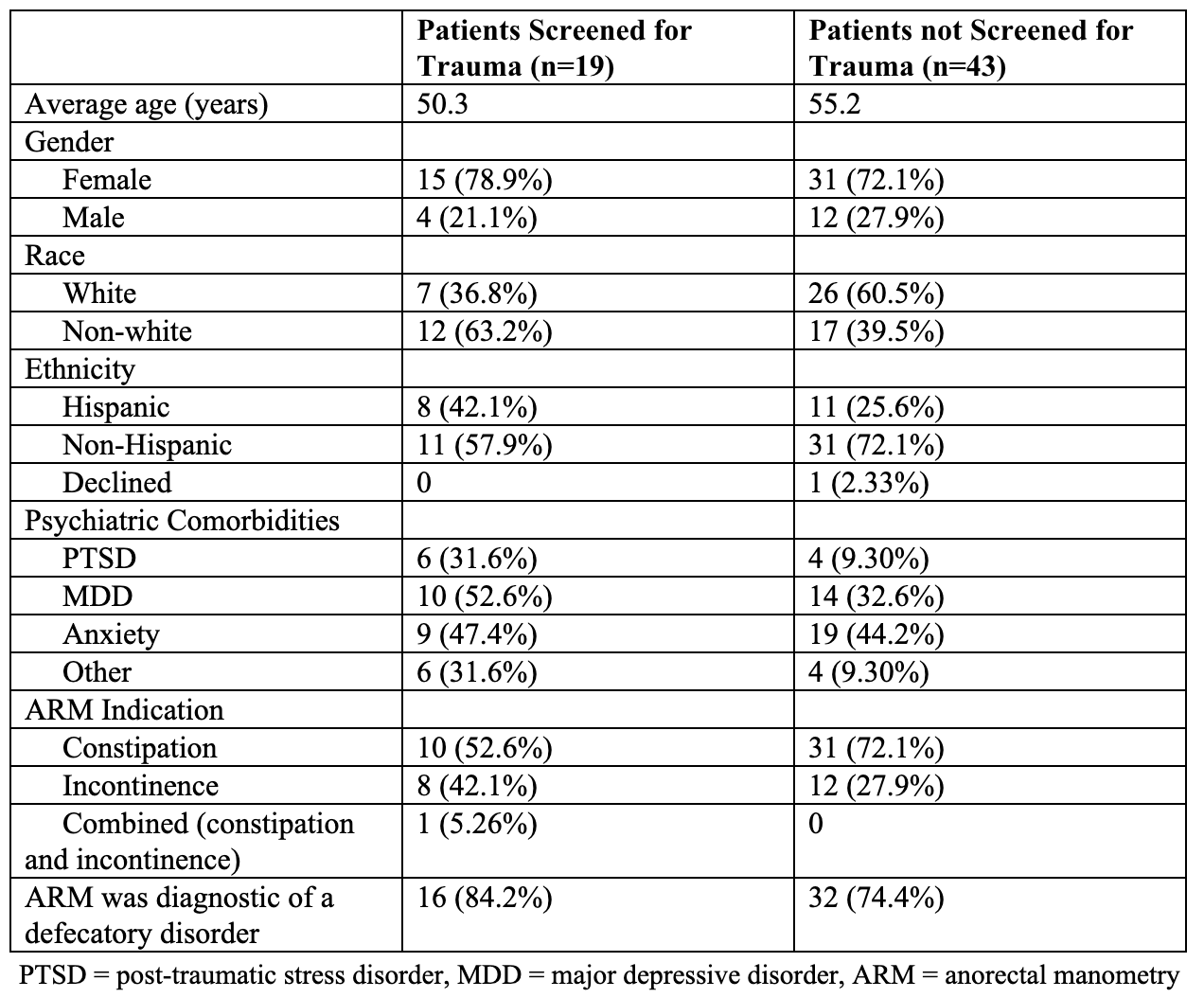
Figure: Demographic and clinical factors of patients who were screened for trauma before ARM and of those who were not screened
Disclosures:
Abigail Bacharach indicated no relevant financial relationships.
Yuying Luo: Ardelyx – Grant/Research Support.
Abigail Bacharach, MD1, Yuying Luo, MD2. P2924 - Low Rates of Trauma Screening Prior to Anorectal Manometry Procedures, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Icahn School of Medicine at Mount Sinai, New York, NY; 2Mount Sinai West & Morningside, New York, NY
Introduction: Almost a quarter of patients with defecatory disorders have a history of trauma and report greater distress during gastrointestinal (GI) procedures. Anorectal manometry (ARM) is commonly ordered to assess defecatory disorders and poses a risk for re-traumatization in some patients. Assessing if patients have a trauma history could help reduce this risk and patients with prior trauma think providers should inquire about it. Research is lacking on rates of trauma screening before ARM. We aimed to determine rates of provider screening for trauma history in patients undergoing ARM.
Methods: A retrospective chart review was performed on consecutive patients who underwent ARM at a tertiary academic center over four months. Demographic and clinical factors were collected including age, gender, indication for ARM, and psychiatric comorbidities. Our primary outcome was if trauma screening was performed; secondary outcomes included if screening was positive and the specialty that performed the screening. Descriptive statistics were performed.
Results: Our cohort included 62 patients (72.6% female) with an average age of 53.7 +/- 16.2 years at time of ARM. 58.1% (n=36) of the cohort was non-Hispanic; 53.2% (n=33) identified as white, 11% (n=7) identified as black. The indication for ARM was most commonly constipation (64.5%), followed by incontinence (27.4%). 19 patients (30.6%) were screened for trauma by any provider; GI providers screened only 5 of these patients with other screening performed by various specialties including psychiatry (n=4), medicine (n=4), obstetrics/gynecology (n=4), and colorectal surgery (n=1). Of the 19 patients screened, 7 screened positive for trauma. Trauma screening was never documented by the proceduralist during the consent process on the day of ARM. 16.1% (n=10) of patients had post-traumatic stress disorder, 38.7% (n=24) had major depressive disorder, 45.2% (n=28) had anxiety, and 16.1% (n=10) had an alternate psychiatric diagnosis. There was no statistically significant difference in demographic factors between those who were screened and those who were not.
Discussion: Fewer than one-third of patients were screened for trauma prior to ARM with GI providers performing a minority of the screening. However, of the patients screened, about one-third screened positive for trauma. Further studies are needed on the best method to screen for trauma in the GI clinical setting and how best to train providers on trauma-informed care, especially during vulnerable procedures.
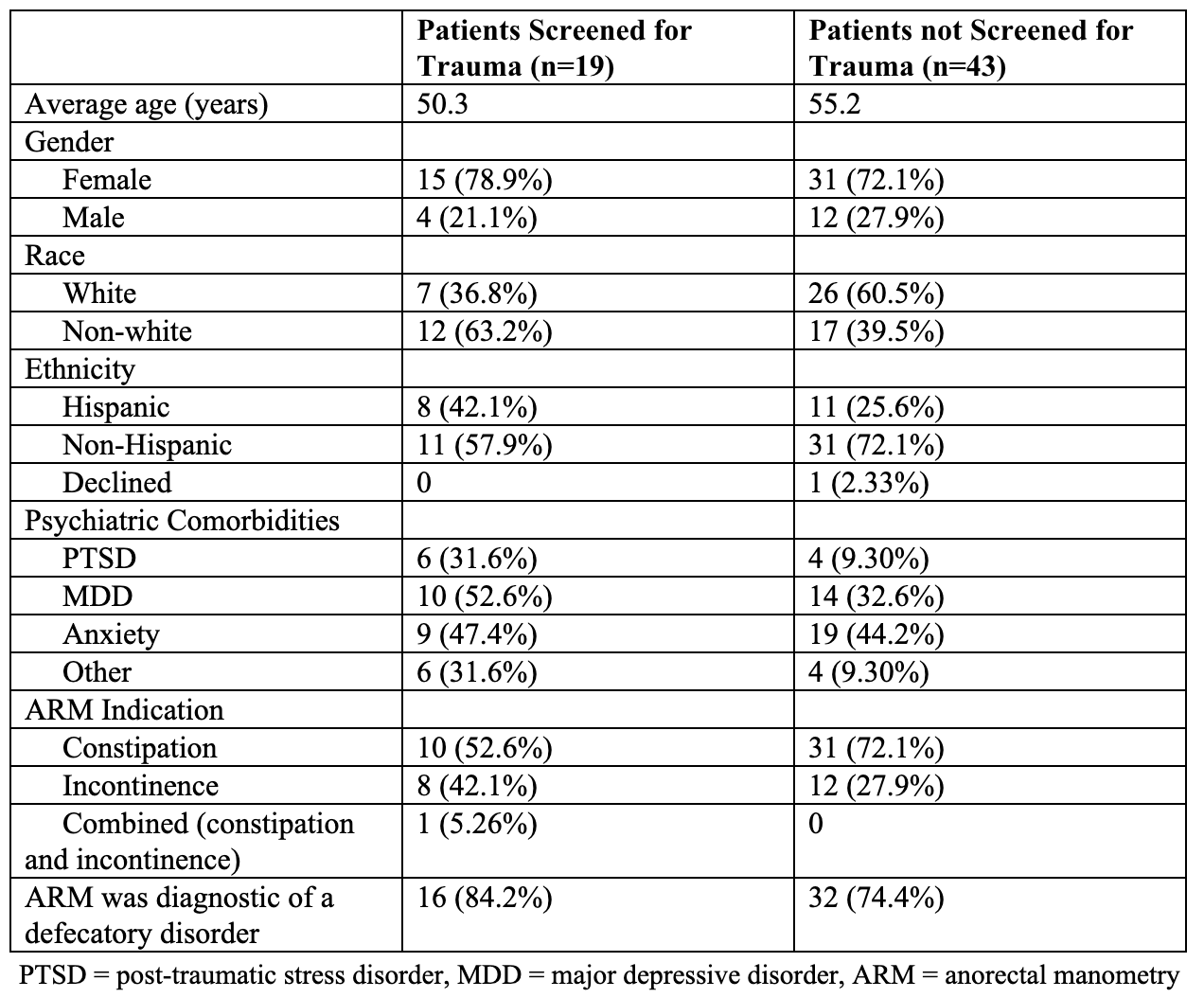
Figure: Demographic and clinical factors of patients who were screened for trauma before ARM and of those who were not screened
Disclosures:
Abigail Bacharach indicated no relevant financial relationships.
Yuying Luo: Ardelyx – Grant/Research Support.
Abigail Bacharach, MD1, Yuying Luo, MD2. P2924 - Low Rates of Trauma Screening Prior to Anorectal Manometry Procedures, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
