Monday Poster Session
Category: Functional Bowel Disease
P2922 - Healthcare Utilization Patterns in Patients With Irritable Bowel Syndrome and Association With IBS-specific Quality of Life (IBS-QOL) Measures
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- JL
Jacqueline Liu, MD
Boston Medical Center
Boston, MA
Presenting Author(s)
Jacqueline Liu, MD1, Kathleen Cheng, MD1, Yu Lu, MPH2, Howard Cabral, PhD2, Horst C. Weber, MD3
1Boston Medical Center, Boston, MA; 2Boston University School of Public Health, Boston, MA; 3VA Boston Healthcare System, Jamaica Plain, MA
Introduction: Irritable bowel syndrome (IBS) is a highly prevalent disorder of gut brain interaction (DGBI) with negative impact on quality of life (QOL), the primary driver of increased healthcare utilization (HCU). A prior prospective study showed that IBS-specific QOL (IBS-QOL) was reduced across racial groups. The aim of this study was to compare measures of HCU between IBS patients and non-IBS controls in that cohort.
Methods: Patients with confirmed IBS (by Rome III) and non-IBS controls from the prospective study cohort were enrolled. Questionnaires for IBS- QOL were completed. Clinical data were collected retrospectively from 2002 to 2015. Measures of HCU included number of office visits, endoscopic procedures, GI referrals, hospitalizations, and abdominal surgeries. Chi-square, Fischer’s exact, two-tailed t-test, and multiple logistic regression analysis were used.
Results: A total of 253 participants were enrolled (IBS, N=72; non-IBS controls, N=181). Basic demographics of participants who underwent EGD and colonoscopy (CLS) for IBS and non-IBS patients were similar except the age distribution for the CLS comparison (Table 1). Regression modeling also showed age was the only significant factor associated with the outcome (p < 0.0001), in contrast to race (p = 0.1), gender (p = 0.5), BMI (p = 1.0), and smoking (p = 0.6). Total and IBS-related GI and PCP visit numbers were significantly higher in the IBS group (p< 0.0001), and PCP visits when related to IBS symptoms, were significantly higher in the IBS cohort (p< 0.005; Fig.1). In both IBS and control groups, increased HCU showed weak to moderate negative correlations with several QoL domains, particularly dysphoria, health worry, relationship, and social reaction. These associations were more pronounced in the IBS cohort, with GI visit frequency showing a stronger inverse relationship with dysphoria and health worry scores. Other measures of HCU did not differ across racial groups except for abdominal surgeries.
Discussion: In this cohort, HCU is significantly higher in IBS patients as compared to non-IBS control participants as measured by office visits and is disparate across racial groups. GI visit frequencies show a moderate inverse relationship with dysphoria and health worry scores in contrast to non-IBS controls suggesting that visit volume may reflect greater symptom burden among IBS patients. Management of IBS should aim to improve QOL to reduce HCU taking into account racial differences.
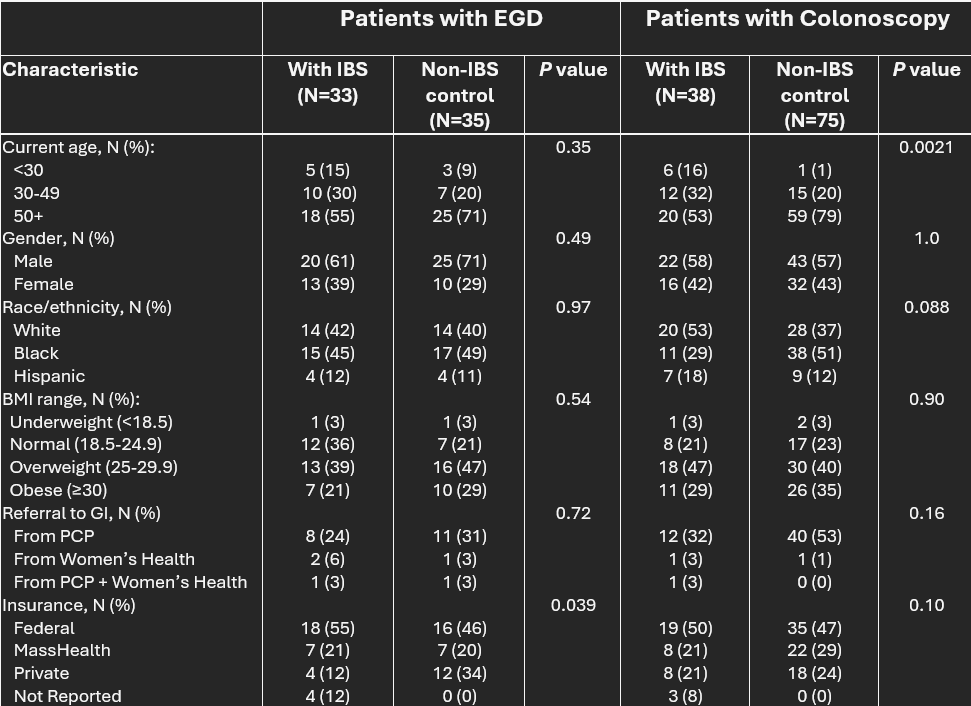
Figure: Table 1: Demographic Data of IBS and Non-IBS control participants are included who underwent at least one EGD or at least one colonoscopy during the 15-year retrospective study duration. Data are presented as counts and column percent: N (%). IBS, Irritable Bowel Syndrome; EGD, Esophago-Gastro-Duodenoscopy; BMI, Body Mass Index (BW KG/Height m2); PCP, Primary Care Physician.
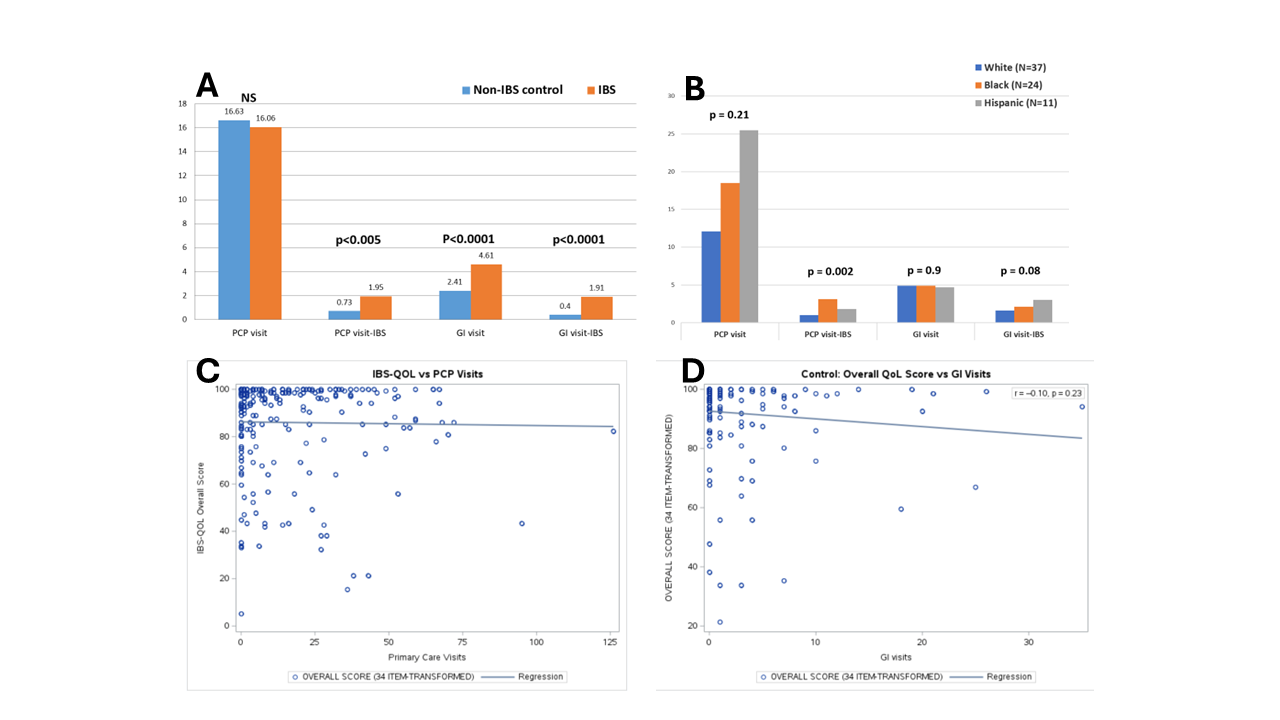
Figure: Figure 1: Number of visits with PCP and GI (total and IBS-related events) were enumerated from a 15-year period (Panel A and B). Office visits of IBS participants were significantly more numerous in the GI and in PCP office space but only for IBS-related symptoms in the PCP office space. Correlation of number of office visits against the individual IBS-QoL scores was determined by generating scatter plots (Panel C and D).
Disclosures:
Jacqueline Liu indicated no relevant financial relationships.
Kathleen Cheng indicated no relevant financial relationships.
Yu Lu indicated no relevant financial relationships.
Howard Cabral indicated no relevant financial relationships.
Horst Weber indicated no relevant financial relationships.
Jacqueline Liu, MD1, Kathleen Cheng, MD1, Yu Lu, MPH2, Howard Cabral, PhD2, Horst C. Weber, MD3. P2922 - Healthcare Utilization Patterns in Patients With Irritable Bowel Syndrome and Association With IBS-specific Quality of Life (IBS-QOL) Measures, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Boston Medical Center, Boston, MA; 2Boston University School of Public Health, Boston, MA; 3VA Boston Healthcare System, Jamaica Plain, MA
Introduction: Irritable bowel syndrome (IBS) is a highly prevalent disorder of gut brain interaction (DGBI) with negative impact on quality of life (QOL), the primary driver of increased healthcare utilization (HCU). A prior prospective study showed that IBS-specific QOL (IBS-QOL) was reduced across racial groups. The aim of this study was to compare measures of HCU between IBS patients and non-IBS controls in that cohort.
Methods: Patients with confirmed IBS (by Rome III) and non-IBS controls from the prospective study cohort were enrolled. Questionnaires for IBS- QOL were completed. Clinical data were collected retrospectively from 2002 to 2015. Measures of HCU included number of office visits, endoscopic procedures, GI referrals, hospitalizations, and abdominal surgeries. Chi-square, Fischer’s exact, two-tailed t-test, and multiple logistic regression analysis were used.
Results: A total of 253 participants were enrolled (IBS, N=72; non-IBS controls, N=181). Basic demographics of participants who underwent EGD and colonoscopy (CLS) for IBS and non-IBS patients were similar except the age distribution for the CLS comparison (Table 1). Regression modeling also showed age was the only significant factor associated with the outcome (p < 0.0001), in contrast to race (p = 0.1), gender (p = 0.5), BMI (p = 1.0), and smoking (p = 0.6). Total and IBS-related GI and PCP visit numbers were significantly higher in the IBS group (p< 0.0001), and PCP visits when related to IBS symptoms, were significantly higher in the IBS cohort (p< 0.005; Fig.1). In both IBS and control groups, increased HCU showed weak to moderate negative correlations with several QoL domains, particularly dysphoria, health worry, relationship, and social reaction. These associations were more pronounced in the IBS cohort, with GI visit frequency showing a stronger inverse relationship with dysphoria and health worry scores. Other measures of HCU did not differ across racial groups except for abdominal surgeries.
Discussion: In this cohort, HCU is significantly higher in IBS patients as compared to non-IBS control participants as measured by office visits and is disparate across racial groups. GI visit frequencies show a moderate inverse relationship with dysphoria and health worry scores in contrast to non-IBS controls suggesting that visit volume may reflect greater symptom burden among IBS patients. Management of IBS should aim to improve QOL to reduce HCU taking into account racial differences.
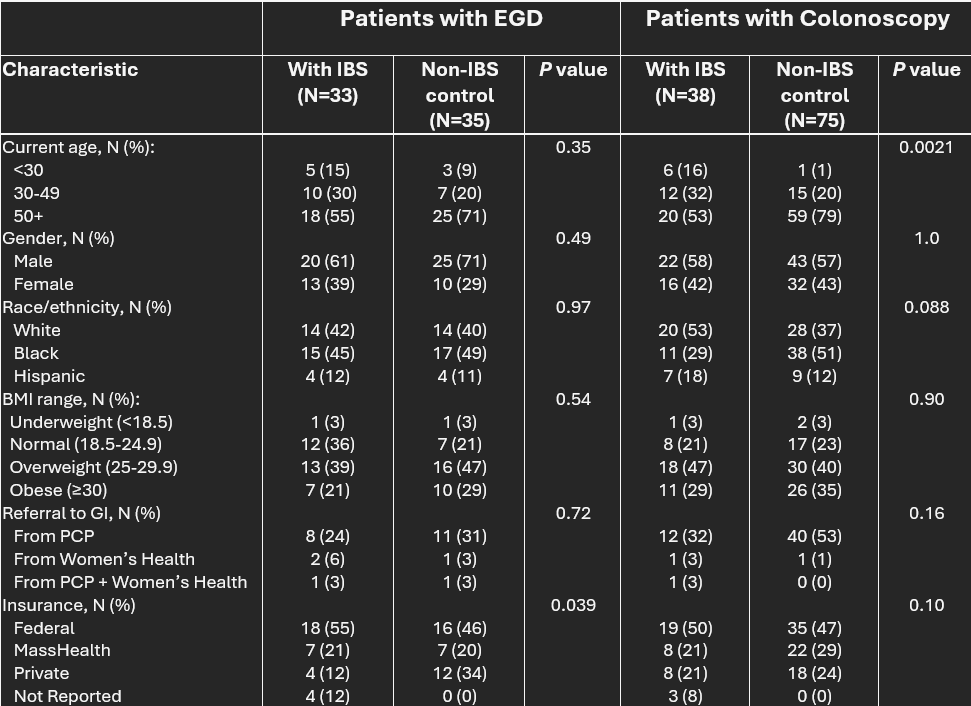
Figure: Table 1: Demographic Data of IBS and Non-IBS control participants are included who underwent at least one EGD or at least one colonoscopy during the 15-year retrospective study duration. Data are presented as counts and column percent: N (%). IBS, Irritable Bowel Syndrome; EGD, Esophago-Gastro-Duodenoscopy; BMI, Body Mass Index (BW KG/Height m2); PCP, Primary Care Physician.
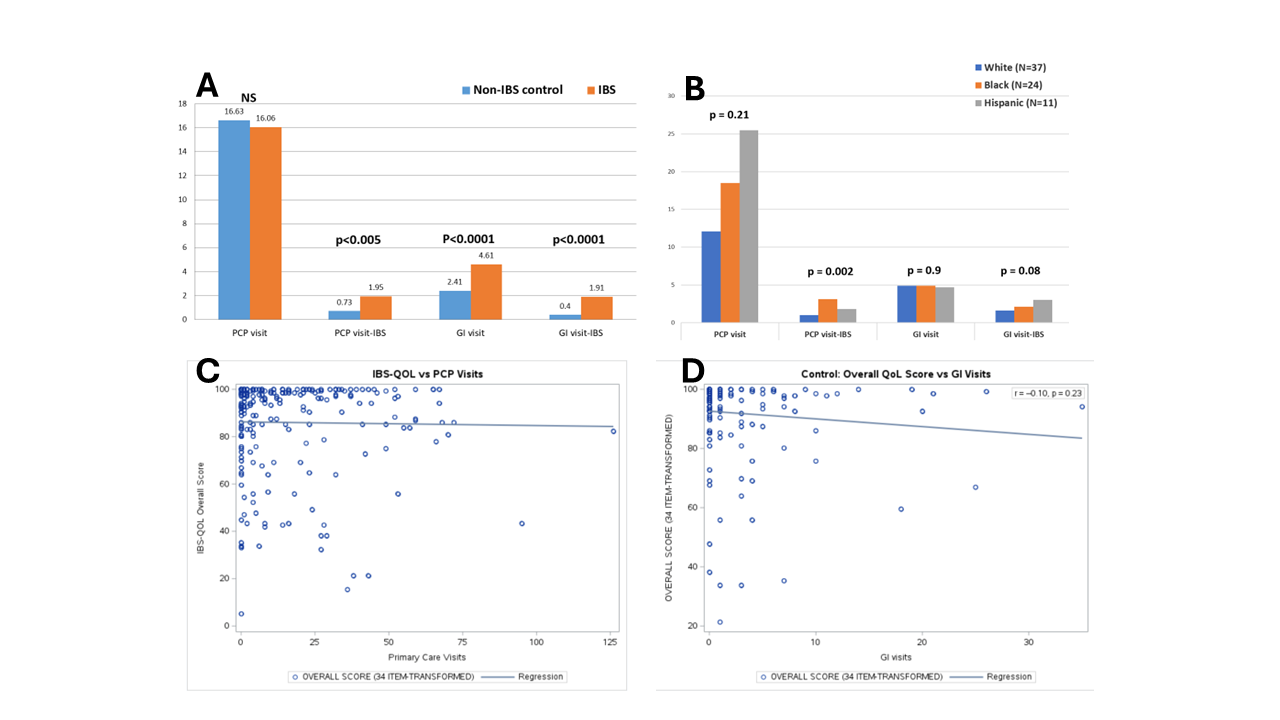
Figure: Figure 1: Number of visits with PCP and GI (total and IBS-related events) were enumerated from a 15-year period (Panel A and B). Office visits of IBS participants were significantly more numerous in the GI and in PCP office space but only for IBS-related symptoms in the PCP office space. Correlation of number of office visits against the individual IBS-QoL scores was determined by generating scatter plots (Panel C and D).
Disclosures:
Jacqueline Liu indicated no relevant financial relationships.
Kathleen Cheng indicated no relevant financial relationships.
Yu Lu indicated no relevant financial relationships.
Howard Cabral indicated no relevant financial relationships.
Horst Weber indicated no relevant financial relationships.
Jacqueline Liu, MD1, Kathleen Cheng, MD1, Yu Lu, MPH2, Howard Cabral, PhD2, Horst C. Weber, MD3. P2922 - Healthcare Utilization Patterns in Patients With Irritable Bowel Syndrome and Association With IBS-specific Quality of Life (IBS-QOL) Measures, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

