Monday Poster Session
Category: Functional Bowel Disease
P2919 - The Association Between Functional Dyspepsia and Celiac Disease: A Nationwide Inpatient Sample Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Gedion Yilma Amdetsion, MD (he/him/his)
Cook County Health
Chicago, IL
Presenting Author(s)
Gedion Yilma Amdetsion, MD1, Chun-wei Pan, MD1, Hiwot G. Tebeje, MD, MPH2, Shreyas Nandyal, MD1, Abhin Sapkota, MBBS3, Seema Gandhi, MD4
1Cook County Health, Chicago, IL; 2Washington University in St. Louis, Saint Louis, MO; 3John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 4John H. Stroger Hospital of Cook Co, Chicago, IL
Introduction: Functional dyspepsia (FD) is a common gastrointestinal disorder, affecting approximately 5 to 16 percent of people worldwide. Although dyspepsia can be a manifestation of Celiac disease(CD), most FD patients do not undergo serological screening for CD, and data on the prevalence of CD in dyspepsia patients is limited. This gap in research has prompted our investigation into the association between FD and celiac disease.
Methods: We conducted a retrospective analysis using the 2017–2022 Nationwide Inpatient Sample (NIS). Demographic covariates, including sex, age and median household income quartile were considered. Clinical risk factors evaluated included anxiety, depression, Helicobacter pylori (H. Pylori), obesity, and smoking history. Associations are reported as odds ratios (OR) after conducting multivariable logistic regression, adjusting for these covariates and clinical risk factors.
Results: Of the 36,146 patients with functional dyspepsia included in our study, 57% were female, 45% had anxiety or depression, 0.07% had a history of H. pylori infection, and 159(0.44%) had Celiac disease. Celiac emerged as a strong predictor of functional dyspepsia, with individuals carrying the diagnosis exhibiting nearly three times the odds of dyspeptic symptoms compared to those without celiac (OR 2.81; 95% CI 2.36–3.34; z = 11.69; P < 0.001). Psychiatric comorbidities also demonstrated significant associations: anxiety was linked to a 74% increase in odds (OR 1.74; 95% CI 1.69–1.79; z = 38.38; P < 0.001), and depression conferred a 26% increase (OR 1.26; 95% CI 1.23–1.30; z = 15.47; P < 0.001). A history of H. pylori infection was similarly associated with higher odds of functional dyspepsia (OR 2.93; 95% CI 1.84–4.65; z = 4.55; P < 0.001).
Discussion: Our findings suggest that celiac disease is an independent risk factor for functional dyspepsia, alongside traditional factors like mood disorders and prior H. pylori infection. Further research is needed to explore these immunological links and the possible role of screening for celiac disease in patients with functional dyspepsia.
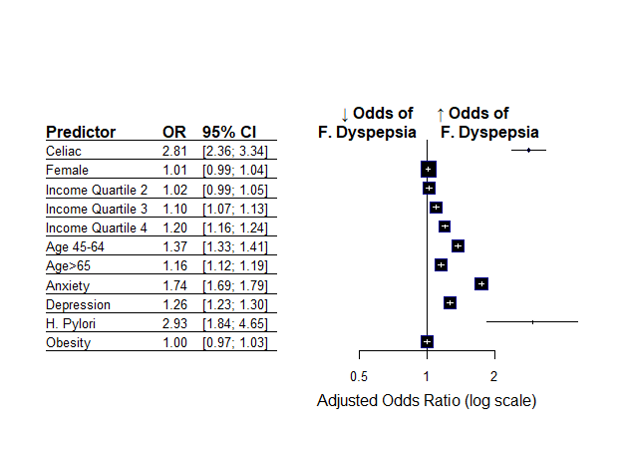
Figure: Fig 1. Multivariate logistic regression on factors associated with Functional dyspepsia
Disclosures:
Gedion Yilma Amdetsion indicated no relevant financial relationships.
Chun-wei Pan indicated no relevant financial relationships.
Hiwot Tebeje indicated no relevant financial relationships.
Shreyas Nandyal indicated no relevant financial relationships.
Abhin Sapkota indicated no relevant financial relationships.
Seema Gandhi indicated no relevant financial relationships.
Gedion Yilma Amdetsion, MD1, Chun-wei Pan, MD1, Hiwot G. Tebeje, MD, MPH2, Shreyas Nandyal, MD1, Abhin Sapkota, MBBS3, Seema Gandhi, MD4. P2919 - The Association Between Functional Dyspepsia and Celiac Disease: A Nationwide Inpatient Sample Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cook County Health, Chicago, IL; 2Washington University in St. Louis, Saint Louis, MO; 3John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 4John H. Stroger Hospital of Cook Co, Chicago, IL
Introduction: Functional dyspepsia (FD) is a common gastrointestinal disorder, affecting approximately 5 to 16 percent of people worldwide. Although dyspepsia can be a manifestation of Celiac disease(CD), most FD patients do not undergo serological screening for CD, and data on the prevalence of CD in dyspepsia patients is limited. This gap in research has prompted our investigation into the association between FD and celiac disease.
Methods: We conducted a retrospective analysis using the 2017–2022 Nationwide Inpatient Sample (NIS). Demographic covariates, including sex, age and median household income quartile were considered. Clinical risk factors evaluated included anxiety, depression, Helicobacter pylori (H. Pylori), obesity, and smoking history. Associations are reported as odds ratios (OR) after conducting multivariable logistic regression, adjusting for these covariates and clinical risk factors.
Results: Of the 36,146 patients with functional dyspepsia included in our study, 57% were female, 45% had anxiety or depression, 0.07% had a history of H. pylori infection, and 159(0.44%) had Celiac disease. Celiac emerged as a strong predictor of functional dyspepsia, with individuals carrying the diagnosis exhibiting nearly three times the odds of dyspeptic symptoms compared to those without celiac (OR 2.81; 95% CI 2.36–3.34; z = 11.69; P < 0.001). Psychiatric comorbidities also demonstrated significant associations: anxiety was linked to a 74% increase in odds (OR 1.74; 95% CI 1.69–1.79; z = 38.38; P < 0.001), and depression conferred a 26% increase (OR 1.26; 95% CI 1.23–1.30; z = 15.47; P < 0.001). A history of H. pylori infection was similarly associated with higher odds of functional dyspepsia (OR 2.93; 95% CI 1.84–4.65; z = 4.55; P < 0.001).
Discussion: Our findings suggest that celiac disease is an independent risk factor for functional dyspepsia, alongside traditional factors like mood disorders and prior H. pylori infection. Further research is needed to explore these immunological links and the possible role of screening for celiac disease in patients with functional dyspepsia.
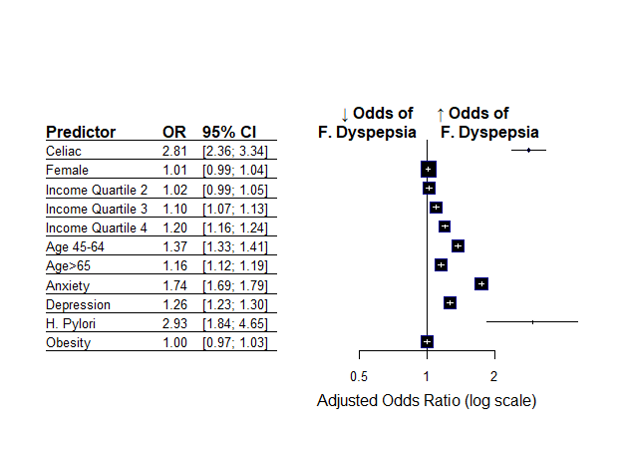
Figure: Fig 1. Multivariate logistic regression on factors associated with Functional dyspepsia
Disclosures:
Gedion Yilma Amdetsion indicated no relevant financial relationships.
Chun-wei Pan indicated no relevant financial relationships.
Hiwot Tebeje indicated no relevant financial relationships.
Shreyas Nandyal indicated no relevant financial relationships.
Abhin Sapkota indicated no relevant financial relationships.
Seema Gandhi indicated no relevant financial relationships.
Gedion Yilma Amdetsion, MD1, Chun-wei Pan, MD1, Hiwot G. Tebeje, MD, MPH2, Shreyas Nandyal, MD1, Abhin Sapkota, MBBS3, Seema Gandhi, MD4. P2919 - The Association Between Functional Dyspepsia and Celiac Disease: A Nationwide Inpatient Sample Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
