Monday Poster Session
Category: Esophagus
P2910 - Esophageal Bullous Pemphigoid
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- MA
Molly Anderson, DO (she/her/hers)
Virginia Mason Franciscan Health
Seattle, WA
Presenting Author(s)
Muaaz Masood, MD1, Molly Anderson, DO2, Montana Hawksford, DO2, Christopher Gault, MD2, Otto Lin, MD2
1Division of Gastroenterology and Hepatology, Center for Digestive Health, Virginia Mason Franciscan Health, Seattle, WA; 2Virginia Mason Franciscan Health, Seattle, WA
Introduction: Bullous pemphigoid (BP) is an autoimmune condition which typically affects adults over 60 years old and involves IgG antibodies against hemidesmosomes in the basement membrane of the skin. Esophageal BP is rare and can occur in 4% of patients, typically manifesting as gastrointestinal (GI) bleeding, dysphagia or odynophagia.
Case Description/
Methods: An 82-year-old male with a history of cerebrovascular accident, dementia, and GERD, who initially presented to his primary care provider with dermatitis on the dorsum of his feet bilaterally. He improved with antifungals and corticosteroids, but subsequently presented two months later due to two weeks of hemoptysis. A laryngoscopy demonstrated multiple dilated vessels in the pharynx and fresh blood pooling around the esophageal orifice. Esophagogastroduodenoscopy (EGD) revealed ulceration in the posterior hypopharynx, desquamation of the proximal esophagus, severe distal esophagitis, and erythema in the gastric cardia and fundus. Esophageal biopsies showed patchy chronic inflammation and gastric biopsies confirmed H. pylori infection. He was treated with amoxicillin and omeprazole with eradication. He subsequently developed taut blisters involving the arms, legs and glans penis. A diagnosis of BP was confirmed with a punch biopsy of the skin which revealed linear depositions of IgG and C3 along the BM zone, positive anti-BP 180 antigen, and a positive immunobullous panel. He received one month of prednisone 40 mg daily followed by mycophenolate 1000 mg in the morning and 500 mg at night. Given recurrent blisters, his mycophenolate dosage was increased to 1000 mg BID and an additional course of prednisone was prescribed which then resulted in remission.
Discussion: BP is associated with blister formation due to the disadhesion of the subepidermal layer of the skin. Oral mucous membranes may be involved. While esophageal BP is rare, it may manifest as strictures, ulcers or hemorrhagic bullae. EGD may be challenging due to the formation of bullae and mucosal sloughing with contact. The diagnosis of BP is typically confirmed with a biopsy of the lesion and direct immunofluorescence. Treatment involves systemic steroids. Azathioprine and rituximab have been utilized as a steroid-sparing therapy. In cases of significant GI bleeding, argon plasma coagulation, which does not require contact with mucosa, may be used for treatment. Clinicians should include BP in the differential in a patient with desquamative esophageal lesions and cutaneous abnormalities.
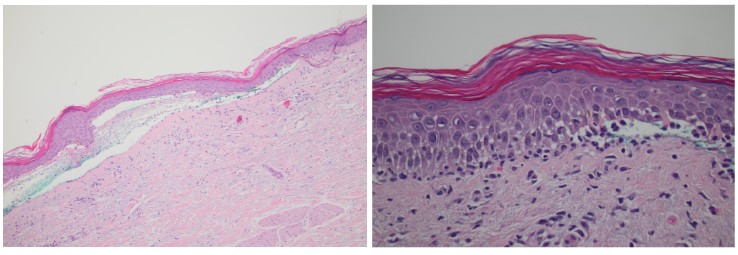
Figure: Panel A. Esophagogastroduodenoscopy (EGD) revealed desquamation of the proximal esophagus (top left, top right) in addition to ulceration in the posterior hypopharynx, severe distal esophagitis and erythema in the gastric cardia and fundus. The patient subsequently developed taut blisters involving the arms and axillary region, (bottom left, bottom right) as well as the legs and glans penis.
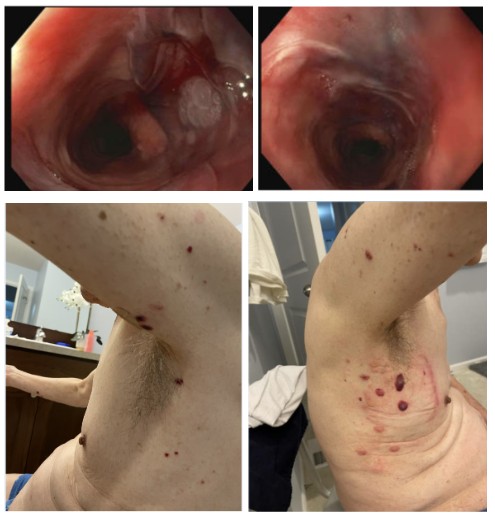
Figure: Panel B. Skin punch biopsy with H&E stained sections (left and right) revealed subepidermal bulla formation containing fibrin, erythrocytes, and mixed inflammation including eosinophils.
Disclosures:
Muaaz Masood indicated no relevant financial relationships.
Molly Anderson indicated no relevant financial relationships.
Montana Hawksford indicated no relevant financial relationships.
Christopher Gault indicated no relevant financial relationships.
Otto Lin indicated no relevant financial relationships.
Muaaz Masood, MD1, Molly Anderson, DO2, Montana Hawksford, DO2, Christopher Gault, MD2, Otto Lin, MD2. P2910 - Esophageal Bullous Pemphigoid, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Division of Gastroenterology and Hepatology, Center for Digestive Health, Virginia Mason Franciscan Health, Seattle, WA; 2Virginia Mason Franciscan Health, Seattle, WA
Introduction: Bullous pemphigoid (BP) is an autoimmune condition which typically affects adults over 60 years old and involves IgG antibodies against hemidesmosomes in the basement membrane of the skin. Esophageal BP is rare and can occur in 4% of patients, typically manifesting as gastrointestinal (GI) bleeding, dysphagia or odynophagia.
Case Description/
Methods: An 82-year-old male with a history of cerebrovascular accident, dementia, and GERD, who initially presented to his primary care provider with dermatitis on the dorsum of his feet bilaterally. He improved with antifungals and corticosteroids, but subsequently presented two months later due to two weeks of hemoptysis. A laryngoscopy demonstrated multiple dilated vessels in the pharynx and fresh blood pooling around the esophageal orifice. Esophagogastroduodenoscopy (EGD) revealed ulceration in the posterior hypopharynx, desquamation of the proximal esophagus, severe distal esophagitis, and erythema in the gastric cardia and fundus. Esophageal biopsies showed patchy chronic inflammation and gastric biopsies confirmed H. pylori infection. He was treated with amoxicillin and omeprazole with eradication. He subsequently developed taut blisters involving the arms, legs and glans penis. A diagnosis of BP was confirmed with a punch biopsy of the skin which revealed linear depositions of IgG and C3 along the BM zone, positive anti-BP 180 antigen, and a positive immunobullous panel. He received one month of prednisone 40 mg daily followed by mycophenolate 1000 mg in the morning and 500 mg at night. Given recurrent blisters, his mycophenolate dosage was increased to 1000 mg BID and an additional course of prednisone was prescribed which then resulted in remission.
Discussion: BP is associated with blister formation due to the disadhesion of the subepidermal layer of the skin. Oral mucous membranes may be involved. While esophageal BP is rare, it may manifest as strictures, ulcers or hemorrhagic bullae. EGD may be challenging due to the formation of bullae and mucosal sloughing with contact. The diagnosis of BP is typically confirmed with a biopsy of the lesion and direct immunofluorescence. Treatment involves systemic steroids. Azathioprine and rituximab have been utilized as a steroid-sparing therapy. In cases of significant GI bleeding, argon plasma coagulation, which does not require contact with mucosa, may be used for treatment. Clinicians should include BP in the differential in a patient with desquamative esophageal lesions and cutaneous abnormalities.
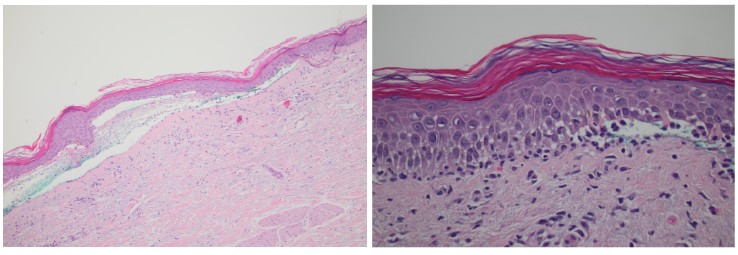
Figure: Panel A. Esophagogastroduodenoscopy (EGD) revealed desquamation of the proximal esophagus (top left, top right) in addition to ulceration in the posterior hypopharynx, severe distal esophagitis and erythema in the gastric cardia and fundus. The patient subsequently developed taut blisters involving the arms and axillary region, (bottom left, bottom right) as well as the legs and glans penis.
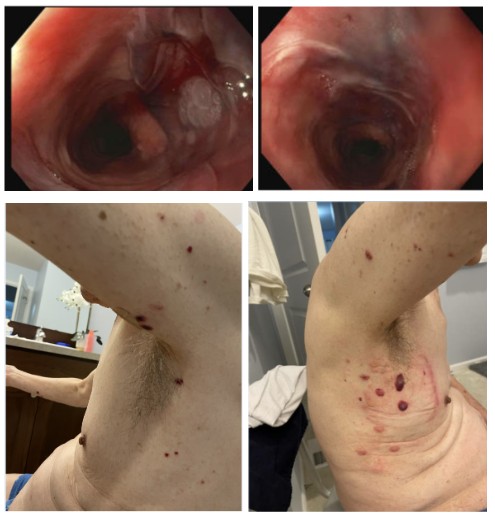
Figure: Panel B. Skin punch biopsy with H&E stained sections (left and right) revealed subepidermal bulla formation containing fibrin, erythrocytes, and mixed inflammation including eosinophils.
Disclosures:
Muaaz Masood indicated no relevant financial relationships.
Molly Anderson indicated no relevant financial relationships.
Montana Hawksford indicated no relevant financial relationships.
Christopher Gault indicated no relevant financial relationships.
Otto Lin indicated no relevant financial relationships.
Muaaz Masood, MD1, Molly Anderson, DO2, Montana Hawksford, DO2, Christopher Gault, MD2, Otto Lin, MD2. P2910 - Esophageal Bullous Pemphigoid, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
