Monday Poster Session
Category: Esophagus
P2787 - Ten-Year Comparative Outcomes of POEM versus Laparoscopic Heller Myotomy for Achalasia: A Propensity-Matched Analysis From a Multicenter Real-World Database
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Archana Kharel, MD (she/her/hers)
Cleveland Clinic
Cleveland, OH
Presenting Author(s)
Archana Kharel, MD1, Shivali Chava, 2, Barish Eren, MD3, Abhin Sapkota, MD4, Umesh Bhagat, MD3, Prabhat Kumar, MD5, Prashanthi Thota, MD3, Madhusudhan Sanaka, MD1
1Cleveland Clinic, Cleveland, OH; 2The University of Texas at Austin, Houston, TX; 3Cleveland Clinic Foundation, Cleveland, OH; 4John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 5Virginia Commonwealth University, Richmond, VA
Introduction: Peroral endoscopic myotomy (POEM) has emerged as a minimally invasive alternative to laparoscopic Heller myotomy (LHM) for achalasia. However, comparative data on long-term outcomes between these modalities remain limited. We aimed to evaluate the 10-year clinical outcomes of POEM versus LHM using a large federated electronic health record database.
Methods: We performed a retrospective cohort study using the TriNetX Research Network, including 100 healthcare organizations. Adult patients (≥18 years) with a diagnosis of achalasia (ICD-10: K22.0) who underwent either POEM (CPT: 43497) or LHM with fundoplasty (CPT: 43279) were identified. Patients with systemic sclerosis or esophageal cancer were excluded. Propensity score matching (1:1) was applied to balance demographics and comorbidities. Primary outcomes included rates of esophageal perforation, esophagectomy, stricture, dysphagia, aspiration pneumonia, GERD, PEG placement, mortality, and need for redo POEM. Kaplan-Meier survival and risk analyses were performed over a 10-year period post-procedure.
Results: After matching, 4,050 patients were included (2,025 per group). Esophageal perforation rates were similar (1.1% POEM vs. 0.7% Heller; p=0.25). POEM was associated with significantly lower rates of esophagectomy (0% vs. 0.5%; p=0.002), esophageal stricture (3.8% vs. 9.0%; p< 0.001), and dysphagia (14.6% vs. 21.8%; p=0.005). Aspiration pneumonia was less frequent in POEM (1.3% vs. 2.3%; p=0.028). GERD incidence was modestly higher in POEM (29.8% vs. 26.5%; p=0.15), accompanied by significantly greater PPI use (68.7% vs. 43.8%; p< 0.001). PEG placement trended lower (0.6% vs. 1.2%; p=0.061). All-cause mortality was substantially reduced in POEM (1.8% vs. 6.7%; p< 0.001). A small subset of POEM patients (3.7%) underwent repeat POEM during the 10-year follow-up.
Discussion: In this large, multicenter analysis, POEM demonstrated favorable long-term outcomes compared to LHM, with reduced esophagectomy, stricture, dysphagia, aspiration pneumonia, and mortality. Higher GERD rates and redo procedures remain considerations. These results support POEM as a durable and effective therapeutic option for achalasia.
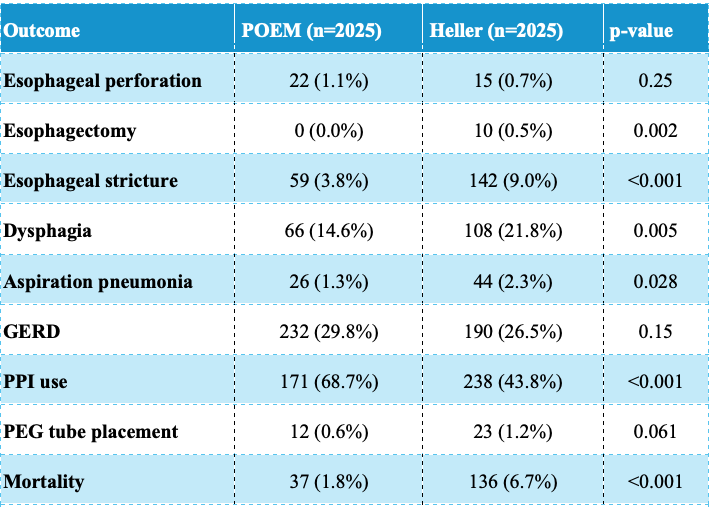
Figure: Table: Comparative 10-Year Outcomes of POEM Versus Laparoscopic Heller Myotomy in Patients With Achalasia
Reported outcomes represent incidence proportions (%) over a 10-year period following initial intervention. Data reflect 1:1 propensity score–matched cohorts (n = 2,025 each). Risk analysis excluded patients with the outcome prior to the index procedure. P-values derived from z-test or log-rank tests, where applicable.
Disclosures:
Archana Kharel indicated no relevant financial relationships.
Shivali Chava indicated no relevant financial relationships.
Barish Eren indicated no relevant financial relationships.
Abhin Sapkota indicated no relevant financial relationships.
Umesh Bhagat indicated no relevant financial relationships.
Prabhat Kumar indicated no relevant financial relationships.
Prashanthi Thota indicated no relevant financial relationships.
Madhusudhan Sanaka indicated no relevant financial relationships.
Archana Kharel, MD1, Shivali Chava, 2, Barish Eren, MD3, Abhin Sapkota, MD4, Umesh Bhagat, MD3, Prabhat Kumar, MD5, Prashanthi Thota, MD3, Madhusudhan Sanaka, MD1. P2787 - Ten-Year Comparative Outcomes of POEM versus Laparoscopic Heller Myotomy for Achalasia: A Propensity-Matched Analysis From a Multicenter Real-World Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cleveland Clinic, Cleveland, OH; 2The University of Texas at Austin, Houston, TX; 3Cleveland Clinic Foundation, Cleveland, OH; 4John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 5Virginia Commonwealth University, Richmond, VA
Introduction: Peroral endoscopic myotomy (POEM) has emerged as a minimally invasive alternative to laparoscopic Heller myotomy (LHM) for achalasia. However, comparative data on long-term outcomes between these modalities remain limited. We aimed to evaluate the 10-year clinical outcomes of POEM versus LHM using a large federated electronic health record database.
Methods: We performed a retrospective cohort study using the TriNetX Research Network, including 100 healthcare organizations. Adult patients (≥18 years) with a diagnosis of achalasia (ICD-10: K22.0) who underwent either POEM (CPT: 43497) or LHM with fundoplasty (CPT: 43279) were identified. Patients with systemic sclerosis or esophageal cancer were excluded. Propensity score matching (1:1) was applied to balance demographics and comorbidities. Primary outcomes included rates of esophageal perforation, esophagectomy, stricture, dysphagia, aspiration pneumonia, GERD, PEG placement, mortality, and need for redo POEM. Kaplan-Meier survival and risk analyses were performed over a 10-year period post-procedure.
Results: After matching, 4,050 patients were included (2,025 per group). Esophageal perforation rates were similar (1.1% POEM vs. 0.7% Heller; p=0.25). POEM was associated with significantly lower rates of esophagectomy (0% vs. 0.5%; p=0.002), esophageal stricture (3.8% vs. 9.0%; p< 0.001), and dysphagia (14.6% vs. 21.8%; p=0.005). Aspiration pneumonia was less frequent in POEM (1.3% vs. 2.3%; p=0.028). GERD incidence was modestly higher in POEM (29.8% vs. 26.5%; p=0.15), accompanied by significantly greater PPI use (68.7% vs. 43.8%; p< 0.001). PEG placement trended lower (0.6% vs. 1.2%; p=0.061). All-cause mortality was substantially reduced in POEM (1.8% vs. 6.7%; p< 0.001). A small subset of POEM patients (3.7%) underwent repeat POEM during the 10-year follow-up.
Discussion: In this large, multicenter analysis, POEM demonstrated favorable long-term outcomes compared to LHM, with reduced esophagectomy, stricture, dysphagia, aspiration pneumonia, and mortality. Higher GERD rates and redo procedures remain considerations. These results support POEM as a durable and effective therapeutic option for achalasia.
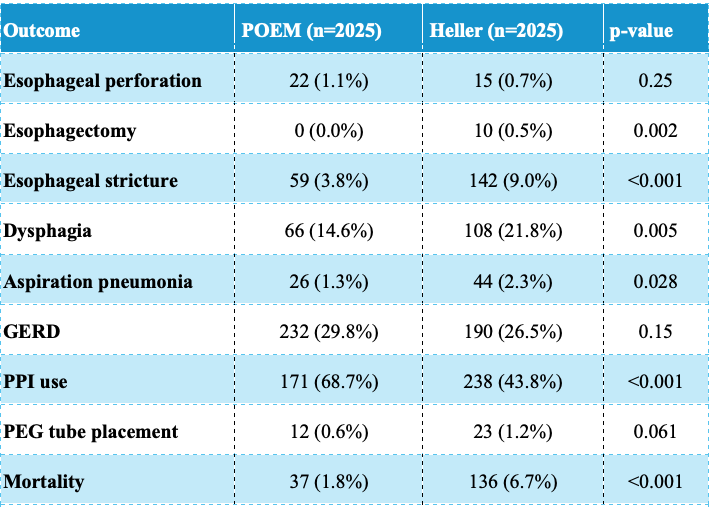
Figure: Table: Comparative 10-Year Outcomes of POEM Versus Laparoscopic Heller Myotomy in Patients With Achalasia
Reported outcomes represent incidence proportions (%) over a 10-year period following initial intervention. Data reflect 1:1 propensity score–matched cohorts (n = 2,025 each). Risk analysis excluded patients with the outcome prior to the index procedure. P-values derived from z-test or log-rank tests, where applicable.
Disclosures:
Archana Kharel indicated no relevant financial relationships.
Shivali Chava indicated no relevant financial relationships.
Barish Eren indicated no relevant financial relationships.
Abhin Sapkota indicated no relevant financial relationships.
Umesh Bhagat indicated no relevant financial relationships.
Prabhat Kumar indicated no relevant financial relationships.
Prashanthi Thota indicated no relevant financial relationships.
Madhusudhan Sanaka indicated no relevant financial relationships.
Archana Kharel, MD1, Shivali Chava, 2, Barish Eren, MD3, Abhin Sapkota, MD4, Umesh Bhagat, MD3, Prabhat Kumar, MD5, Prashanthi Thota, MD3, Madhusudhan Sanaka, MD1. P2787 - Ten-Year Comparative Outcomes of POEM versus Laparoscopic Heller Myotomy for Achalasia: A Propensity-Matched Analysis From a Multicenter Real-World Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
