Monday Poster Session
Category: Esophagus
P2786 - Ten-Year Outcomes of Racial and Demographic Disparities in Peroral Endoscopic Myotomy (POEM) for Achalasia: A Nationwide Real-World Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Archana Kharel, MD (she/her/hers)
Cleveland Clinic
Cleveland, OH
Presenting Author(s)
Archana Kharel, MD1, Umesh Bhagat, MD2, Shivali Chava, 3, Abhin Sapkota, MD4, Mohamad-Noor Abu-Hammour, MD1, Prabhat Kumar, MD5, Prashanthi Thota, MD2, Madhusudhan Sanaka, MD1
1Cleveland Clinic, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, OH; 3The University of Texas at Austin, Houston, TX; 4John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 5Virginia Commonwealth University, Richmond, VA
Introduction: Peroral endoscopic myotomy (POEM) is an established minimally invasive intervention for achalasia. However, disparities in utilization and clinical outcomes by race, ethnicity, sex, and age have not been well characterized in real-world U.S. practice. We aimed to evaluate 10-year outcomes following POEM, with a focus on demographic and racial/ethnic variation.
Methods: We queried the TriNetX Research USA Network (2015–2025) for adults (≥18 years) diagnosed with achalasia (ICD-10: K22.0) who underwent POEM (CPT: 43497). Patients with esophageal malignancy, pregnancy, or prior Heller myotomy were excluded. Primary outcomes included post-procedure GERD, esophageal perforation, aspiration pneumonia, PPI use, and all-cause mortality. Results were stratified by age, sex, race, and ethnicity.
Results: Among 1,666 POEM recipients, 61% were White, 10% Black or African American, 3% Asian, and 6% Hispanic or Latino. GERD developed in 70.9% of patients, with higher rates in females (76.5%) and those >75 years (77%). Esophageal perforation occurred in 1.9% of the cohort but was disproportionately higher among Hispanic (9.1%) and Black (4.6%) patients. Aspiration pneumonia was noted in 5.8%, with elevated rates in Asian patients (28.6%) and those over 80 years (52.6%). All-cause mortality was 2.1% overall, but significantly elevated in Asian (28.6%) and Black (4.6%) groups. Hispanic or Latino patients also had the highest PPI utilization (9.1%), suggesting possible disparities in reflux symptom burden or management.
Discussion: In this 10-year, multicenter cohort study, POEM outcomes varied significantly across racial and ethnic groups. Minority populations were both underrepresented and experienced higher complication and mortality rates. These findings underscore the importance of equity-focused strategies in procedural care pathways, symptom monitoring, and post-POEM follow-up.
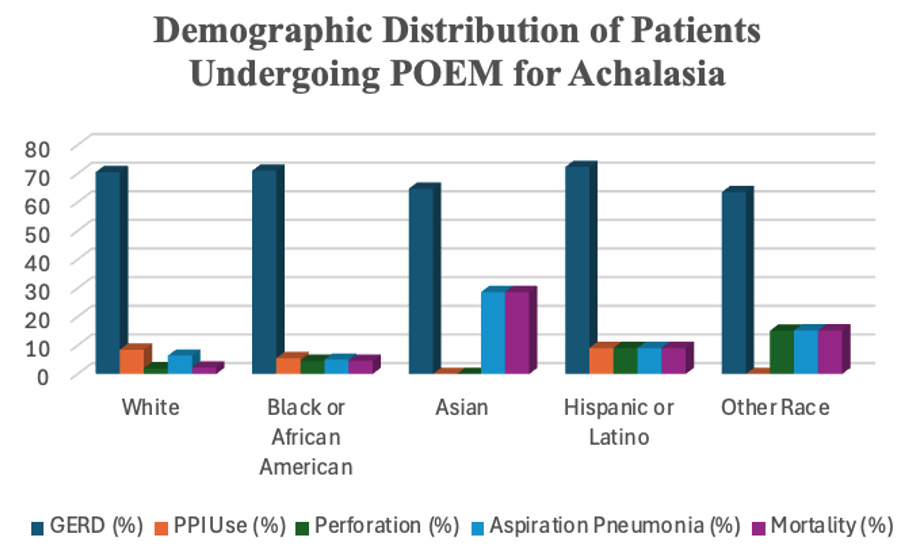
Figure: Chart. Demographic Distribution of Patients Undergoing POEM for Achalasia
Approximate racial and ethnic breakdown of adult patients (≥18 years) undergoing POEM between May 2015 and May 2025. Values represent the proportion of total patients within each category. Underrepresentation of minority groups and a high proportion of patients with unknown race/ethnicity were observed.
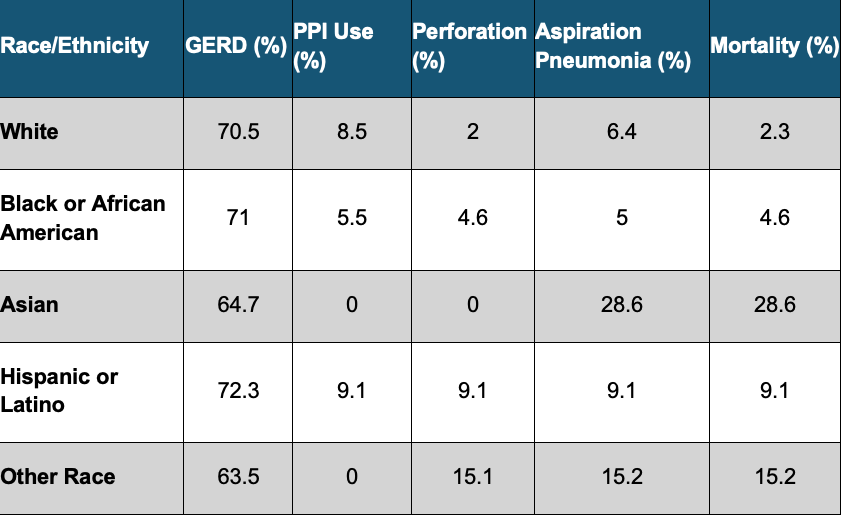
Figure: Table: 10-year outcomes following POEM, with a focus on demographic and racial/ethnic variation.
Disclosures:
Archana Kharel indicated no relevant financial relationships.
Umesh Bhagat indicated no relevant financial relationships.
Shivali Chava indicated no relevant financial relationships.
Abhin Sapkota indicated no relevant financial relationships.
Mohamad-Noor Abu-Hammour indicated no relevant financial relationships.
Prabhat Kumar indicated no relevant financial relationships.
Prashanthi Thota indicated no relevant financial relationships.
Madhusudhan Sanaka indicated no relevant financial relationships.
Archana Kharel, MD1, Umesh Bhagat, MD2, Shivali Chava, 3, Abhin Sapkota, MD4, Mohamad-Noor Abu-Hammour, MD1, Prabhat Kumar, MD5, Prashanthi Thota, MD2, Madhusudhan Sanaka, MD1. P2786 - Ten-Year Outcomes of Racial and Demographic Disparities in Peroral Endoscopic Myotomy (POEM) for Achalasia: A Nationwide Real-World Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cleveland Clinic, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, OH; 3The University of Texas at Austin, Houston, TX; 4John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 5Virginia Commonwealth University, Richmond, VA
Introduction: Peroral endoscopic myotomy (POEM) is an established minimally invasive intervention for achalasia. However, disparities in utilization and clinical outcomes by race, ethnicity, sex, and age have not been well characterized in real-world U.S. practice. We aimed to evaluate 10-year outcomes following POEM, with a focus on demographic and racial/ethnic variation.
Methods: We queried the TriNetX Research USA Network (2015–2025) for adults (≥18 years) diagnosed with achalasia (ICD-10: K22.0) who underwent POEM (CPT: 43497). Patients with esophageal malignancy, pregnancy, or prior Heller myotomy were excluded. Primary outcomes included post-procedure GERD, esophageal perforation, aspiration pneumonia, PPI use, and all-cause mortality. Results were stratified by age, sex, race, and ethnicity.
Results: Among 1,666 POEM recipients, 61% were White, 10% Black or African American, 3% Asian, and 6% Hispanic or Latino. GERD developed in 70.9% of patients, with higher rates in females (76.5%) and those >75 years (77%). Esophageal perforation occurred in 1.9% of the cohort but was disproportionately higher among Hispanic (9.1%) and Black (4.6%) patients. Aspiration pneumonia was noted in 5.8%, with elevated rates in Asian patients (28.6%) and those over 80 years (52.6%). All-cause mortality was 2.1% overall, but significantly elevated in Asian (28.6%) and Black (4.6%) groups. Hispanic or Latino patients also had the highest PPI utilization (9.1%), suggesting possible disparities in reflux symptom burden or management.
Discussion: In this 10-year, multicenter cohort study, POEM outcomes varied significantly across racial and ethnic groups. Minority populations were both underrepresented and experienced higher complication and mortality rates. These findings underscore the importance of equity-focused strategies in procedural care pathways, symptom monitoring, and post-POEM follow-up.
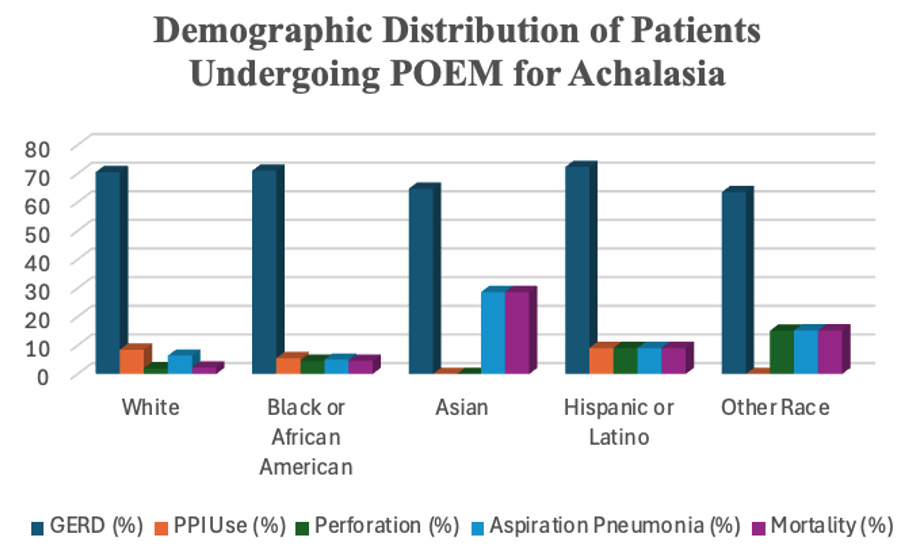
Figure: Chart. Demographic Distribution of Patients Undergoing POEM for Achalasia
Approximate racial and ethnic breakdown of adult patients (≥18 years) undergoing POEM between May 2015 and May 2025. Values represent the proportion of total patients within each category. Underrepresentation of minority groups and a high proportion of patients with unknown race/ethnicity were observed.
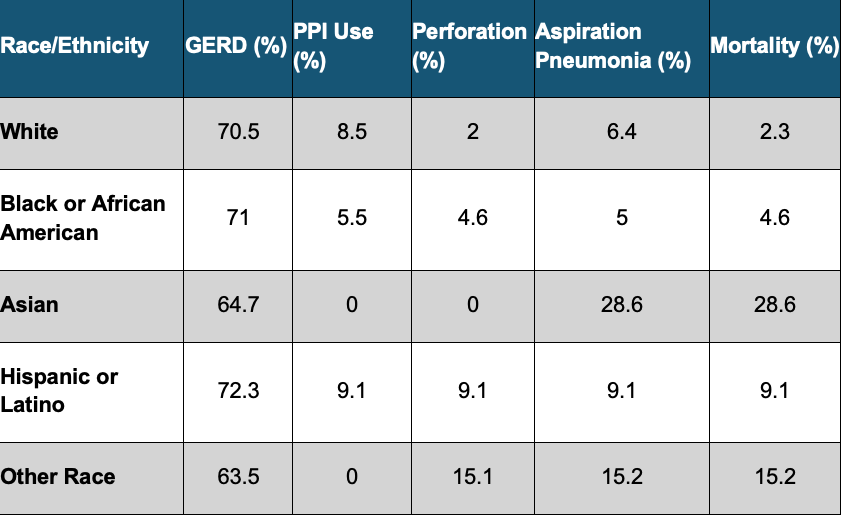
Figure: Table: 10-year outcomes following POEM, with a focus on demographic and racial/ethnic variation.
Disclosures:
Archana Kharel indicated no relevant financial relationships.
Umesh Bhagat indicated no relevant financial relationships.
Shivali Chava indicated no relevant financial relationships.
Abhin Sapkota indicated no relevant financial relationships.
Mohamad-Noor Abu-Hammour indicated no relevant financial relationships.
Prabhat Kumar indicated no relevant financial relationships.
Prashanthi Thota indicated no relevant financial relationships.
Madhusudhan Sanaka indicated no relevant financial relationships.
Archana Kharel, MD1, Umesh Bhagat, MD2, Shivali Chava, 3, Abhin Sapkota, MD4, Mohamad-Noor Abu-Hammour, MD1, Prabhat Kumar, MD5, Prashanthi Thota, MD2, Madhusudhan Sanaka, MD1. P2786 - Ten-Year Outcomes of Racial and Demographic Disparities in Peroral Endoscopic Myotomy (POEM) for Achalasia: A Nationwide Real-World Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

