Monday Poster Session
Category: Esophagus
P2782 - Trends in Incidence of Esophageal Squamous Cell Carcinoma in the United States Between 2001-2021: A United States Cancer Statistics Database Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Yazan Abboud, MD
Rutgers New Jersey Medical School
Newark, NJ
Presenting Author(s)
Yazan Abboud, MD1, Anila Vasireddy, MD2, Cadman Leggett, MD3, Prasad Iyer, MD, MS4, Srinivas Gaddam, MD, MPH5, Amrit K. Kamboj, MD5
1Rutgers New Jersey Medical School, Newark, NJ; 2University of Pennsylvania Health System, Philadelphia, PA; 3Mayo Clinic, Rochester, MN; 4Mayo Clinic, Phoenix, AZ; 5Cedars-Sinai Medical Center, Los Angeles, CA
Introduction: Although esophageal squamous cell carcinoma (ESCC) is the most common histological subtype of esophageal cancer worldwide, it is less common than esophageal adenocarcinoma (EAC) in the US. While there has been extensive research on the epidemiology of EAC in the US, ESCC remains understudied. This study aimed to examine trends in incidence of ESCC in the US over the past two decades using the United States Cancer Statistics (USCS) database.
Methods: ESCC incidence rates between 2001-2021 were age-adjusted to the standard 2000 US population and calculated from the USCS database (covers ~98% of US population). ESCC was identified using ICD-O 3rd edition codes. Incidence rates were categorized by sex (males and females), age (young-onset aged < 50 years and late-onset aged ³50 years), race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, non-Hispanic American Indian/Alaskan Native, and non-Hispanic Asian/Pacific Islander), stage of diagnosis (early and late), and geographical region (Northeast, Midwest, West, and South). Annual percentage change (APC) and average APC (AAPC) were calculated utilizing Joinpoint Regression and the weighted Bayesian Information Criteria method (p< 0.05).
Results: There were 99,501 patients diagnosed with ESCC between 2001-2021. Most patients were males (65%), non-Hispanic White (63%), >50 years of age (95%), from the southern region of the US (40%), and diagnosed at a late stage (66%). Overall, ESCC incidence decreased over the study period (AAPC -2.37, p< 0.001) (Table 1). The declining trend was seen in both males (AAPC -2.80, p< 0.001) and females (AAPC -1.67, p< 0.001), and in both young-onset (AAPC -3.17, p< 0.001) and late-onset ESCC (AAPC -2.30, p< 0.001) (Figure 1). All racial/ethnic groups experienced a similar decrease except non-Hispanic American Indian/Alaskan Natives who had a stable trend (AAPC -0.74, p=0.34). The decrease was noted in both early (AAPC -2.80, p< 0.001) and late-stage tumors (AAPC -1.28, p< 0.001), and in all geographical regions (p< 0.001 for all regions).
Discussion: This study provides the most comprehensive analysis of ESCC in the US using the USCS database which is representative of 98% of the population. Over the past two decades, there was a decline in ESCC incidence overall and across various subgroups. These findings may be attributed to advancements in endoscopic identification and management of esophageal squamous dysplasia and possibly due to public health efforts targeting risk factors such as tobacco use.
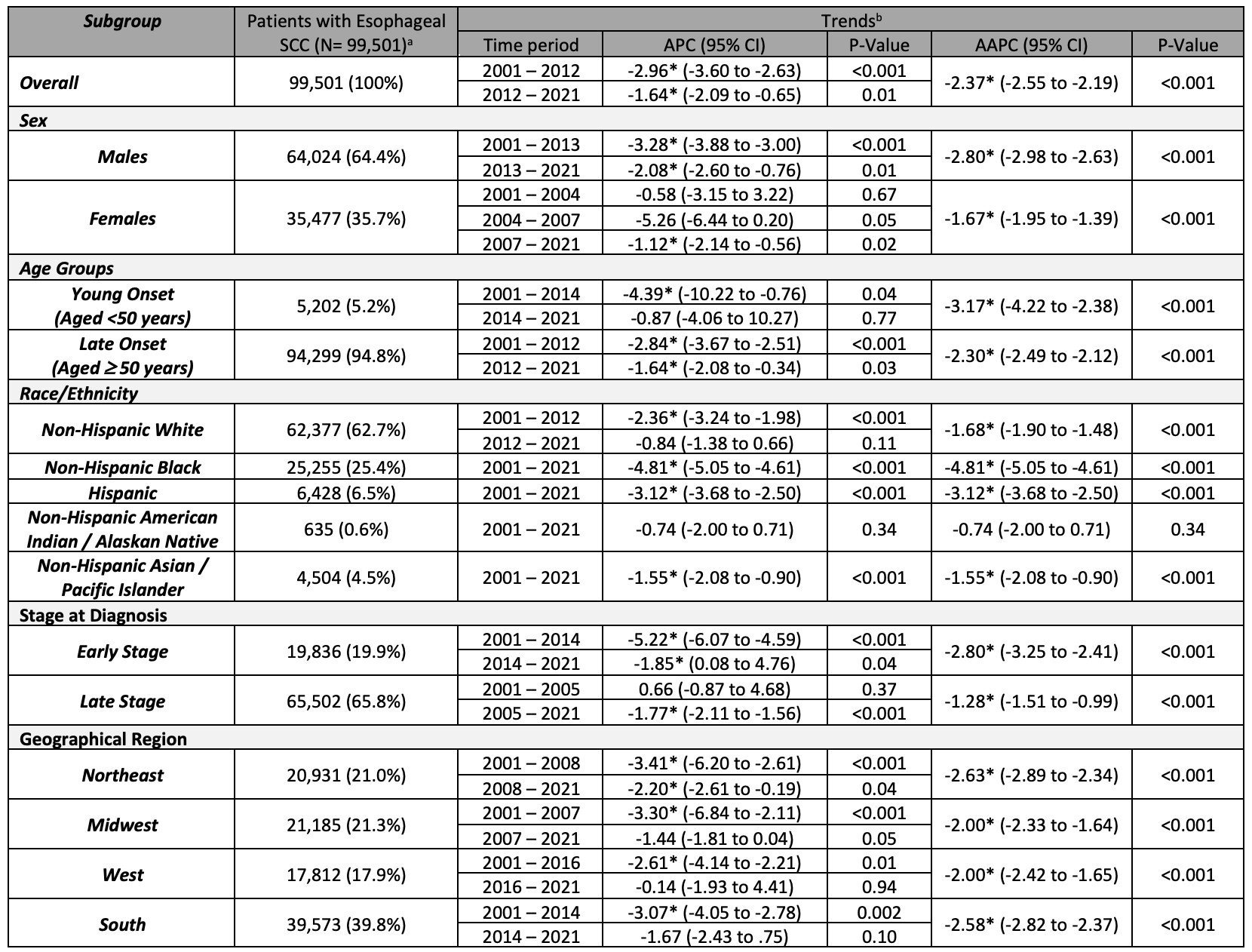
Figure: Table 1. Patient characteristics and trends related to esophageal squamous cell carcinoma (ESCC) in the United States between 2001-2021.
a Data are presented as count numbers followed by percentages of the count numbers from the total cases of ESCC in the database.
b Time-trends were computed using Joinpoint Regression Program (v5.1.0.0, NCI) with 3 maximum joinpoints allowed (4-line segments).
* Implies statistical significance.
APC: Annual Percentage Change, AAPC: Average Annual Percentage Change
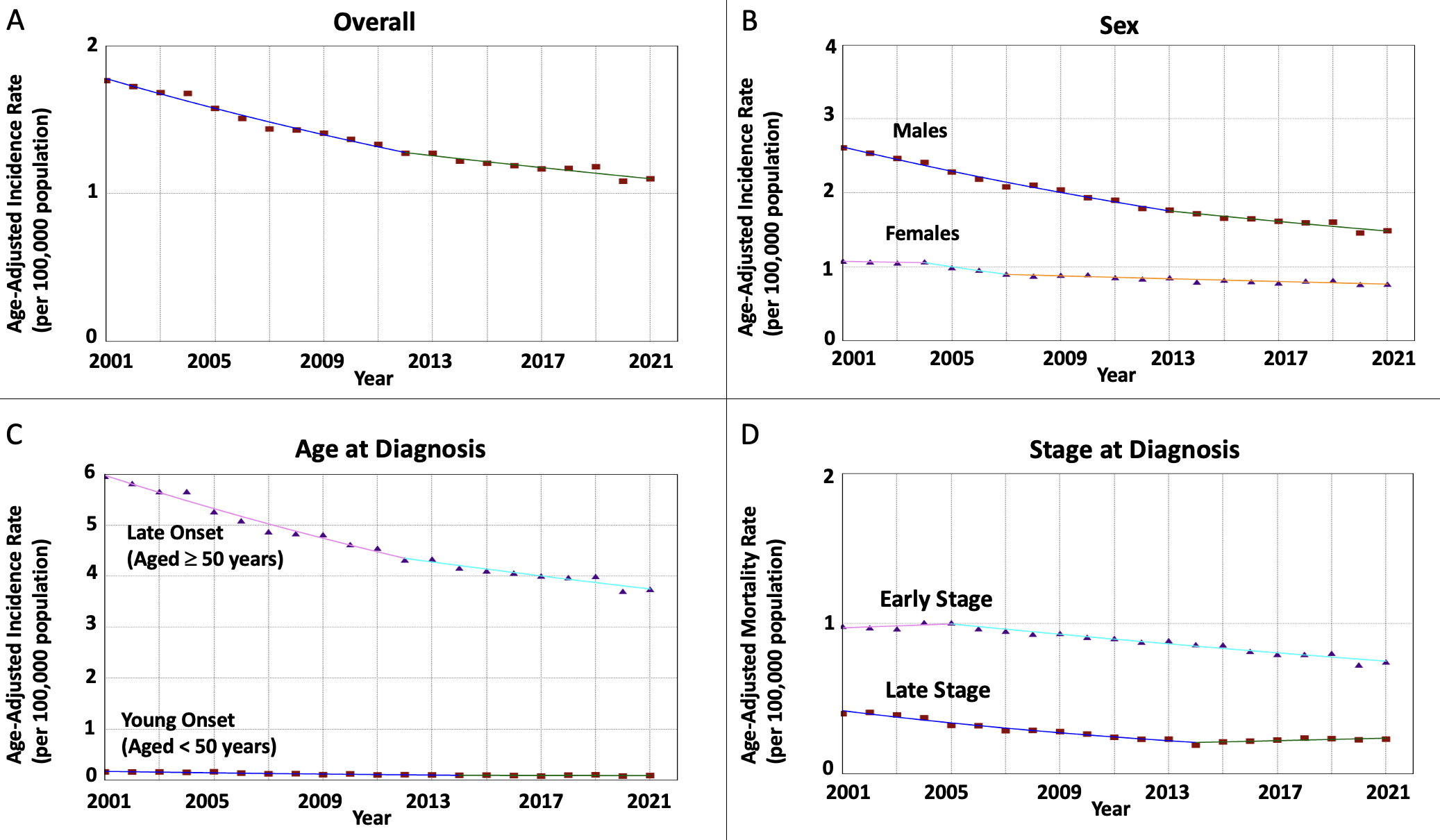
Figure: Figure 1. Time trends in incidence rates of esophageal squamous cell carcinoma in the United States from 2001-2021 as follows: A) Overall, and Subcategorized by B) Sex, C) Age at diagnosis, and D) Stage at diagnosis.
Disclosures:
Yazan Abboud indicated no relevant financial relationships.
Anila Vasireddy indicated no relevant financial relationships.
Cadman Leggett indicated no relevant financial relationships.
Prasad Iyer: CDx medical – Consultant, Grant/Research Support. Exact – Grant/Research Support. Exact Sciences – Consultant, Grant/Research Support. Medtronic – Consultant. Pentax Medical – Consultant, Grant/Research Support.
Srinivas Gaddam indicated no relevant financial relationships.
Amrit Kamboj: Sanofi – Speakers Bureau.
Yazan Abboud, MD1, Anila Vasireddy, MD2, Cadman Leggett, MD3, Prasad Iyer, MD, MS4, Srinivas Gaddam, MD, MPH5, Amrit K. Kamboj, MD5. P2782 - Trends in Incidence of Esophageal Squamous Cell Carcinoma in the United States Between 2001-2021: A United States Cancer Statistics Database Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Rutgers New Jersey Medical School, Newark, NJ; 2University of Pennsylvania Health System, Philadelphia, PA; 3Mayo Clinic, Rochester, MN; 4Mayo Clinic, Phoenix, AZ; 5Cedars-Sinai Medical Center, Los Angeles, CA
Introduction: Although esophageal squamous cell carcinoma (ESCC) is the most common histological subtype of esophageal cancer worldwide, it is less common than esophageal adenocarcinoma (EAC) in the US. While there has been extensive research on the epidemiology of EAC in the US, ESCC remains understudied. This study aimed to examine trends in incidence of ESCC in the US over the past two decades using the United States Cancer Statistics (USCS) database.
Methods: ESCC incidence rates between 2001-2021 were age-adjusted to the standard 2000 US population and calculated from the USCS database (covers ~98% of US population). ESCC was identified using ICD-O 3rd edition codes. Incidence rates were categorized by sex (males and females), age (young-onset aged < 50 years and late-onset aged ³50 years), race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, non-Hispanic American Indian/Alaskan Native, and non-Hispanic Asian/Pacific Islander), stage of diagnosis (early and late), and geographical region (Northeast, Midwest, West, and South). Annual percentage change (APC) and average APC (AAPC) were calculated utilizing Joinpoint Regression and the weighted Bayesian Information Criteria method (p< 0.05).
Results: There were 99,501 patients diagnosed with ESCC between 2001-2021. Most patients were males (65%), non-Hispanic White (63%), >50 years of age (95%), from the southern region of the US (40%), and diagnosed at a late stage (66%). Overall, ESCC incidence decreased over the study period (AAPC -2.37, p< 0.001) (Table 1). The declining trend was seen in both males (AAPC -2.80, p< 0.001) and females (AAPC -1.67, p< 0.001), and in both young-onset (AAPC -3.17, p< 0.001) and late-onset ESCC (AAPC -2.30, p< 0.001) (Figure 1). All racial/ethnic groups experienced a similar decrease except non-Hispanic American Indian/Alaskan Natives who had a stable trend (AAPC -0.74, p=0.34). The decrease was noted in both early (AAPC -2.80, p< 0.001) and late-stage tumors (AAPC -1.28, p< 0.001), and in all geographical regions (p< 0.001 for all regions).
Discussion: This study provides the most comprehensive analysis of ESCC in the US using the USCS database which is representative of 98% of the population. Over the past two decades, there was a decline in ESCC incidence overall and across various subgroups. These findings may be attributed to advancements in endoscopic identification and management of esophageal squamous dysplasia and possibly due to public health efforts targeting risk factors such as tobacco use.
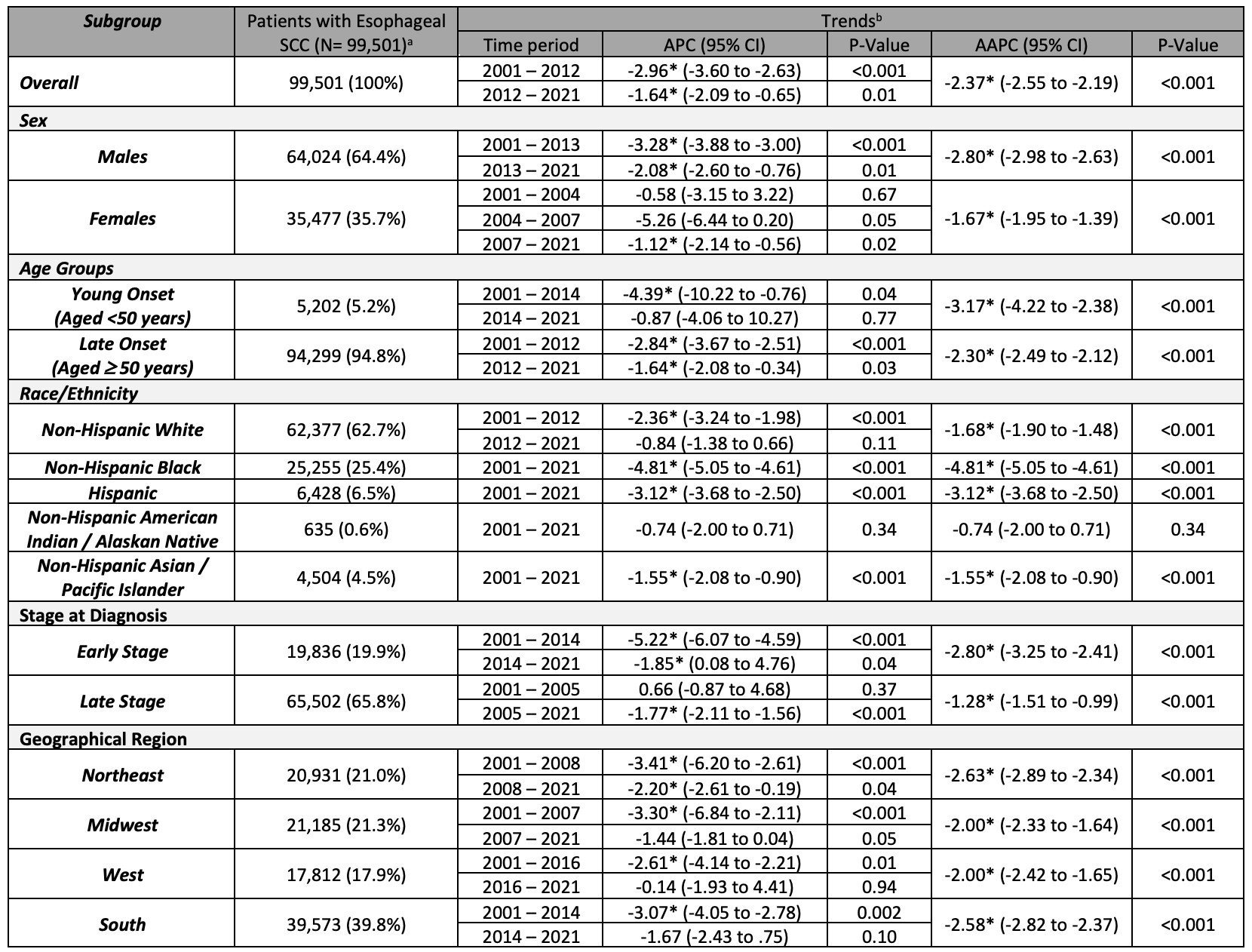
Figure: Table 1. Patient characteristics and trends related to esophageal squamous cell carcinoma (ESCC) in the United States between 2001-2021.
a Data are presented as count numbers followed by percentages of the count numbers from the total cases of ESCC in the database.
b Time-trends were computed using Joinpoint Regression Program (v5.1.0.0, NCI) with 3 maximum joinpoints allowed (4-line segments).
* Implies statistical significance.
APC: Annual Percentage Change, AAPC: Average Annual Percentage Change
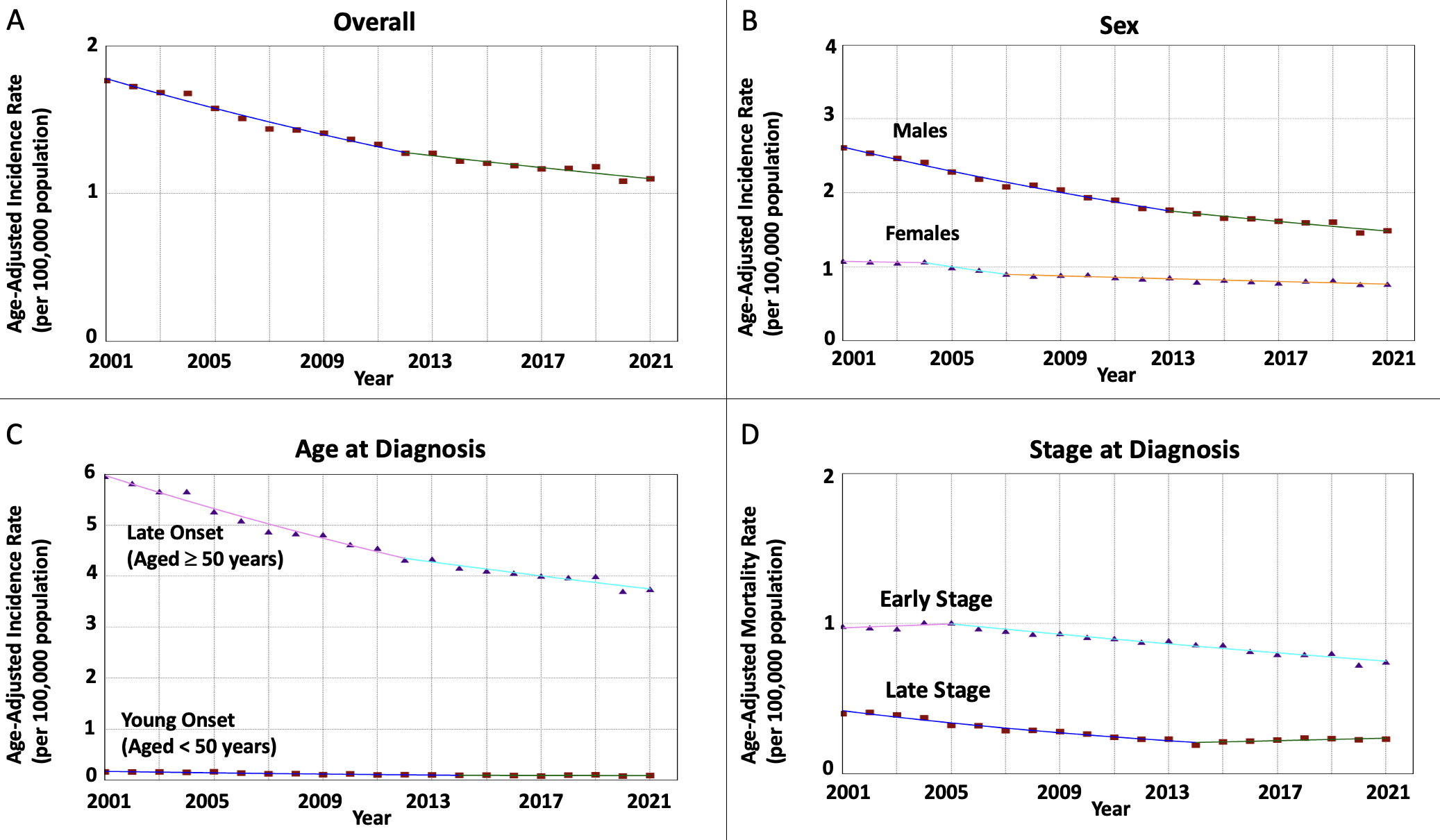
Figure: Figure 1. Time trends in incidence rates of esophageal squamous cell carcinoma in the United States from 2001-2021 as follows: A) Overall, and Subcategorized by B) Sex, C) Age at diagnosis, and D) Stage at diagnosis.
Disclosures:
Yazan Abboud indicated no relevant financial relationships.
Anila Vasireddy indicated no relevant financial relationships.
Cadman Leggett indicated no relevant financial relationships.
Prasad Iyer: CDx medical – Consultant, Grant/Research Support. Exact – Grant/Research Support. Exact Sciences – Consultant, Grant/Research Support. Medtronic – Consultant. Pentax Medical – Consultant, Grant/Research Support.
Srinivas Gaddam indicated no relevant financial relationships.
Amrit Kamboj: Sanofi – Speakers Bureau.
Yazan Abboud, MD1, Anila Vasireddy, MD2, Cadman Leggett, MD3, Prasad Iyer, MD, MS4, Srinivas Gaddam, MD, MPH5, Amrit K. Kamboj, MD5. P2782 - Trends in Incidence of Esophageal Squamous Cell Carcinoma in the United States Between 2001-2021: A United States Cancer Statistics Database Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

