Monday Poster Session
Category: Esophagus
P2776 - Clinical and Demographic Predictors of Peptic Stricture: A Cohort Study of Over 5 Million GERD Patients Using a Large US National Health Record Database
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Sven Eriksson, MD, MS
Allegheny Health Network
Pittsburgh, PA
Presenting Author(s)
Sven Eriksson, MD, MS1, Inanc Sarici, MD1, Ping Zheng, MD1, Shahin Ayazi, MD2
1Allegheny Health Network, Pittsburgh, PA; 2Allegheny General Hospital, Pittsburgh, PA
Introduction: Peptic stricture is a common complication of GERD, yet population-level data on risk factors for its formation are limited. This study aimed to identify demographic, clinical, and medication exposure predictors of esophageal stricture in a large national cohort of GERD patients.
Methods: We conducted a retrospective cohort study using TriNetX, a federated electronic health record database. Adults diagnosed with GERD from 2015–2020 were selected. Patients were stratified by subsequent development of esophageal stricture, defined using diagnosis and procedure codes. Demographic characteristics, comorbidities, and medication use were compared between groups. Only patients who underwent endoscopy were included in comparative analysis.
Results: There were 5,035,574 patients with GERD. At a mean (SD) follow-up of 4.88 (3.6) years, 165,017 (3.4%) developed esophageal stricture, with a median time from GERD diagnosis to stricture of 888 days.
Of the GERD population, 1,280,887 patients (25.4%) underwent endoscopy. This group was divided based on the presence or absence of esophageal stricture, and their demographic and clinical characteristics are compared in Table 1. Stricture formation was more likely in older and Caucasian patients. Asian patients were less likely to form strictures (OR 0.43).
Hiatal hernia and esophagitis were strong clinical predictors of stricture. Barrett’s esophagus was also more prevalent. Stricture was associated with subsequent esophageal cancer [0.36% vs 0.13%, OR 2.85 (2.6–3.1), p< 0.0001]. Aspiration pneumonia was more common in patients with stricture [7.1% vs 4.1%, OR 1.79 (1.75–1.83), p< 0.0001]. Among systemic comorbidities, scleroderma had the strongest association. In contrast, H. pylori (OR 0.50) and Crohn’s (OR 0.84) were protective.
NSAID and steroid use are compared in Table 2. Strictures were slightly more common in selective and non-selective NSAIDs, as well as glucocorticoids, particularly dexamethasone and budesonide.
Discussion: Peptic stricture in GERD reflects a distinct clinical phenotype, characterized by older age, Caucasian race, hiatal hernia, and inflammatory injury. Strong associations with esophageal cancer and aspiration pneumonia underscore the serious implications of this complication. Inverse associations with Helicobacter pylori and Asian race suggest biological or environmental factors influence progression. These findings highlight the heterogeneity of GERD and support a personalized, risk-based approach to surveillance and management.
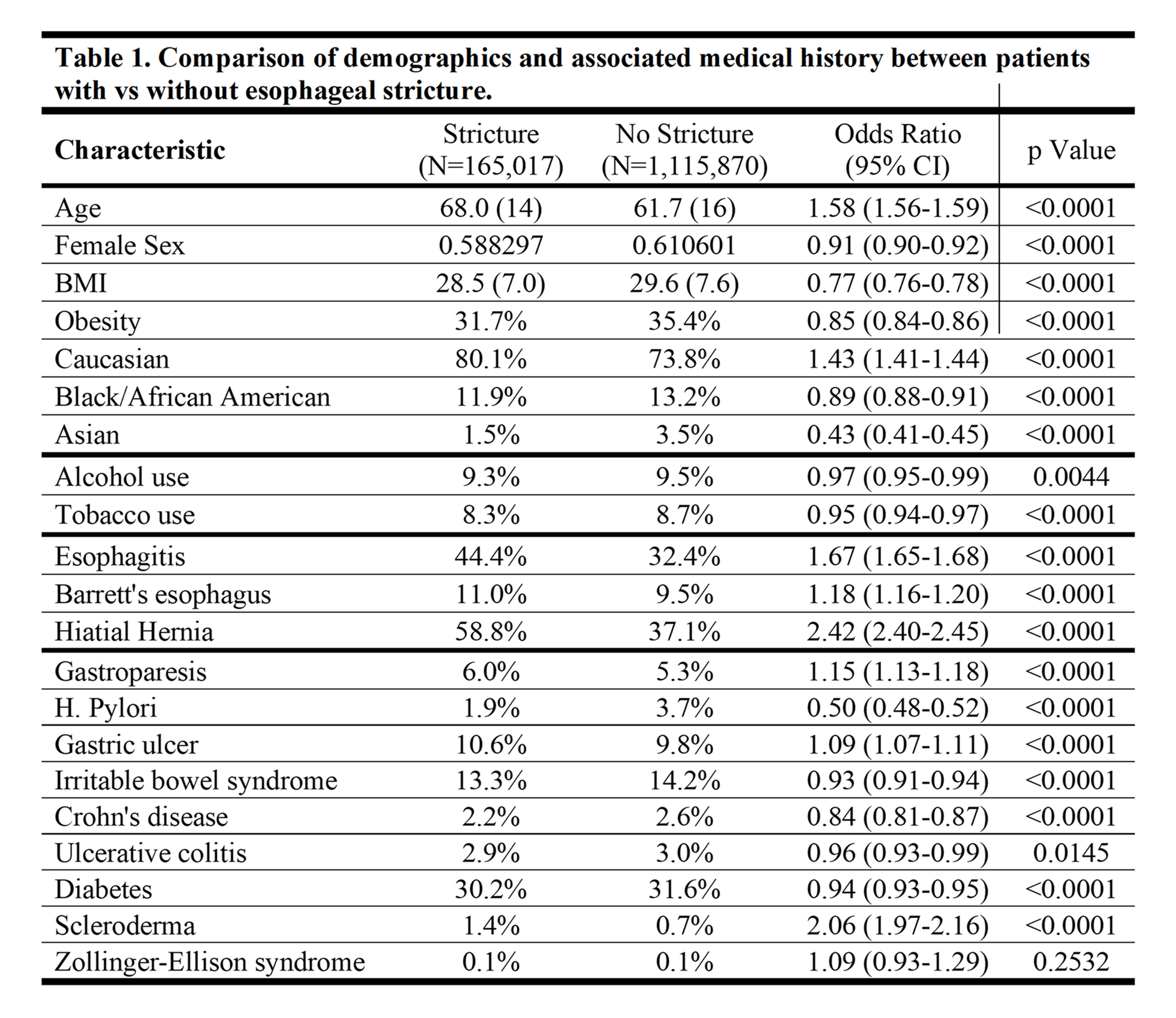
Figure: Table 1. Comparison of demographics and associated medical history between patients with vs without esophageal stricture.
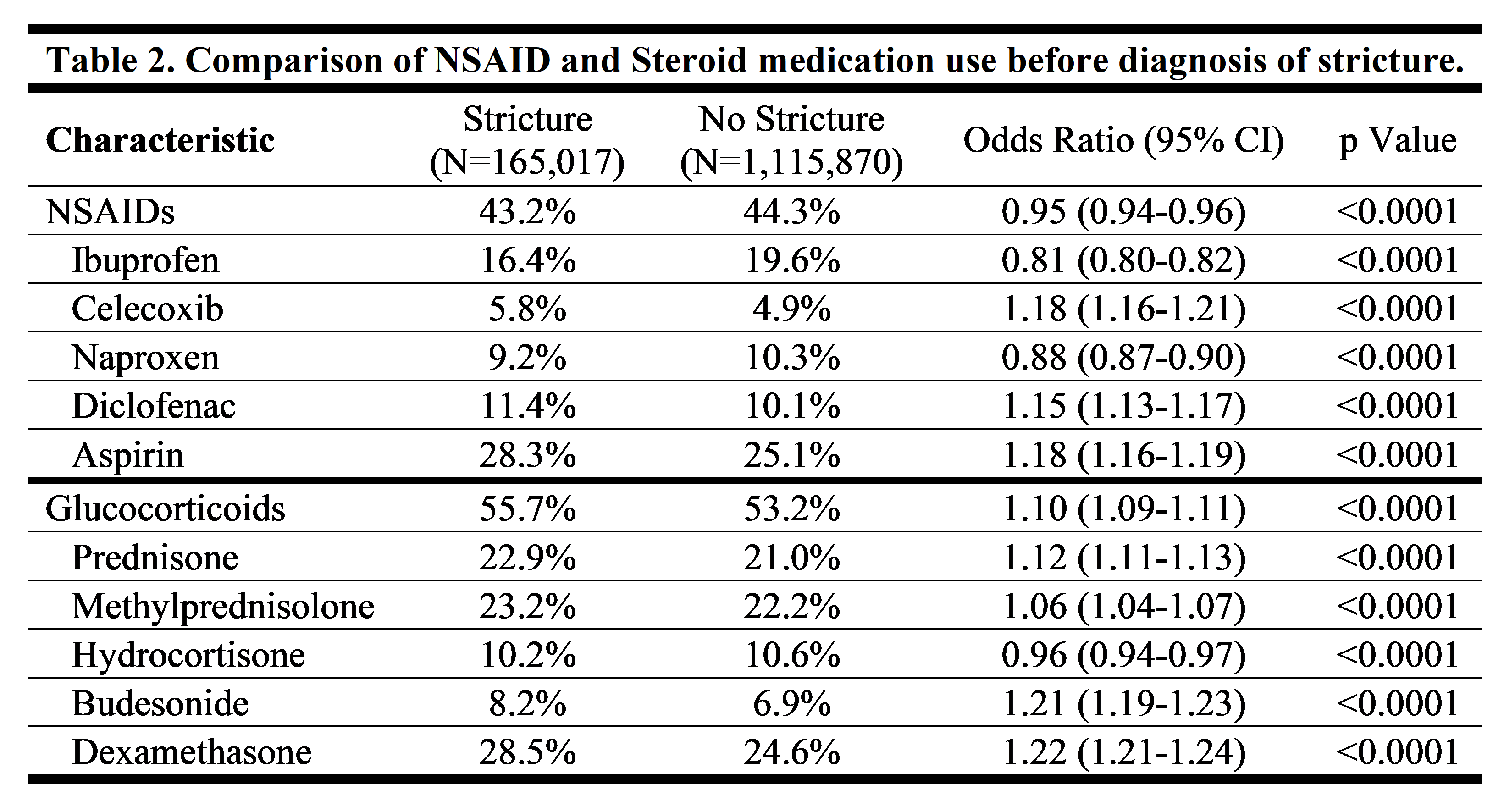
Figure: Table 2. Comparison of NSAID and Steroid medication use before diagnosis of stricture.
Disclosures:
Sven Eriksson indicated no relevant financial relationships.
Inanc Sarici indicated no relevant financial relationships.
Ping Zheng indicated no relevant financial relationships.
Shahin Ayazi indicated no relevant financial relationships.
Sven Eriksson, MD, MS1, Inanc Sarici, MD1, Ping Zheng, MD1, Shahin Ayazi, MD2. P2776 - Clinical and Demographic Predictors of Peptic Stricture: A Cohort Study of Over 5 Million GERD Patients Using a Large US National Health Record Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Allegheny Health Network, Pittsburgh, PA; 2Allegheny General Hospital, Pittsburgh, PA
Introduction: Peptic stricture is a common complication of GERD, yet population-level data on risk factors for its formation are limited. This study aimed to identify demographic, clinical, and medication exposure predictors of esophageal stricture in a large national cohort of GERD patients.
Methods: We conducted a retrospective cohort study using TriNetX, a federated electronic health record database. Adults diagnosed with GERD from 2015–2020 were selected. Patients were stratified by subsequent development of esophageal stricture, defined using diagnosis and procedure codes. Demographic characteristics, comorbidities, and medication use were compared between groups. Only patients who underwent endoscopy were included in comparative analysis.
Results: There were 5,035,574 patients with GERD. At a mean (SD) follow-up of 4.88 (3.6) years, 165,017 (3.4%) developed esophageal stricture, with a median time from GERD diagnosis to stricture of 888 days.
Of the GERD population, 1,280,887 patients (25.4%) underwent endoscopy. This group was divided based on the presence or absence of esophageal stricture, and their demographic and clinical characteristics are compared in Table 1. Stricture formation was more likely in older and Caucasian patients. Asian patients were less likely to form strictures (OR 0.43).
Hiatal hernia and esophagitis were strong clinical predictors of stricture. Barrett’s esophagus was also more prevalent. Stricture was associated with subsequent esophageal cancer [0.36% vs 0.13%, OR 2.85 (2.6–3.1), p< 0.0001]. Aspiration pneumonia was more common in patients with stricture [7.1% vs 4.1%, OR 1.79 (1.75–1.83), p< 0.0001]. Among systemic comorbidities, scleroderma had the strongest association. In contrast, H. pylori (OR 0.50) and Crohn’s (OR 0.84) were protective.
NSAID and steroid use are compared in Table 2. Strictures were slightly more common in selective and non-selective NSAIDs, as well as glucocorticoids, particularly dexamethasone and budesonide.
Discussion: Peptic stricture in GERD reflects a distinct clinical phenotype, characterized by older age, Caucasian race, hiatal hernia, and inflammatory injury. Strong associations with esophageal cancer and aspiration pneumonia underscore the serious implications of this complication. Inverse associations with Helicobacter pylori and Asian race suggest biological or environmental factors influence progression. These findings highlight the heterogeneity of GERD and support a personalized, risk-based approach to surveillance and management.
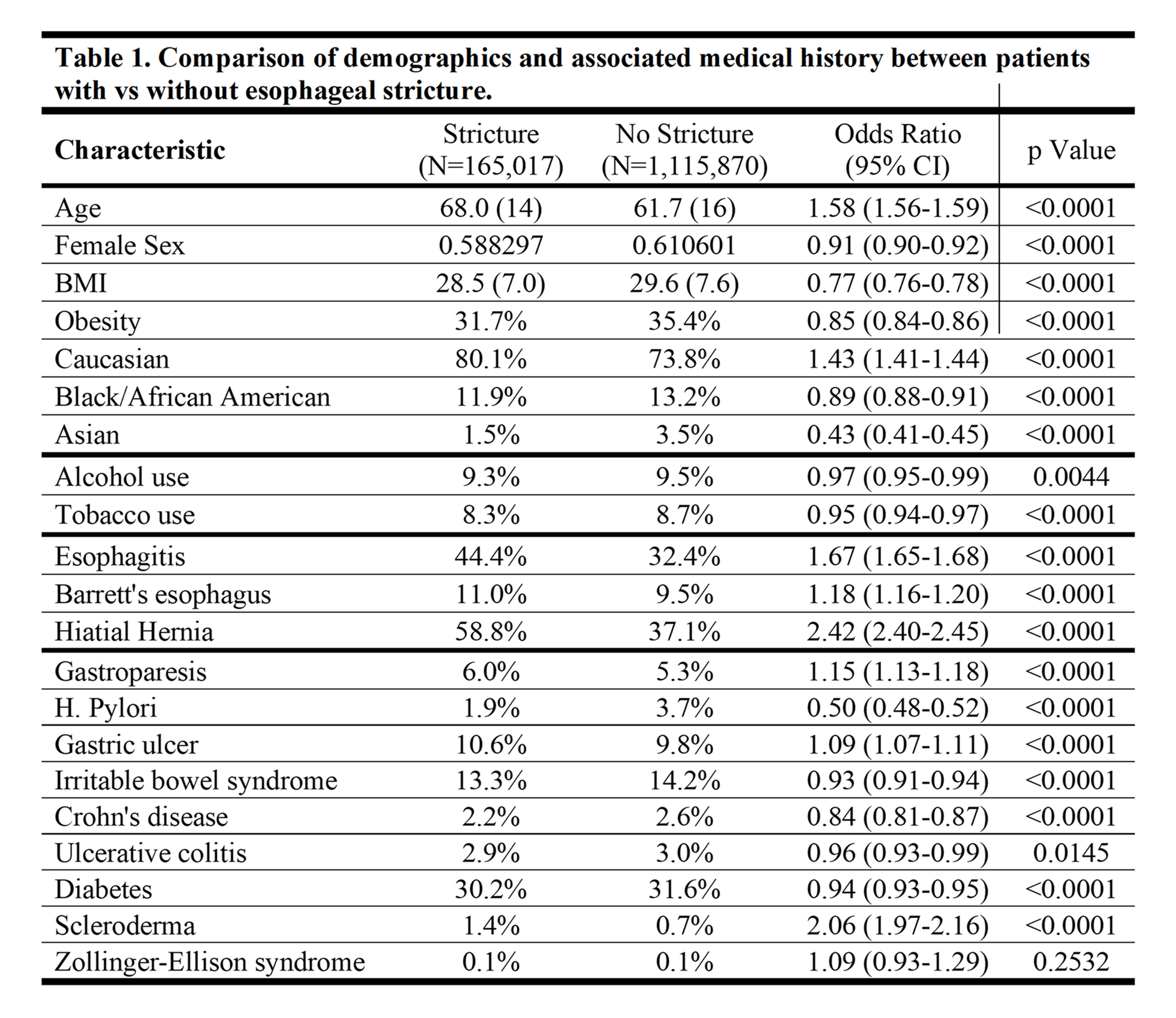
Figure: Table 1. Comparison of demographics and associated medical history between patients with vs without esophageal stricture.
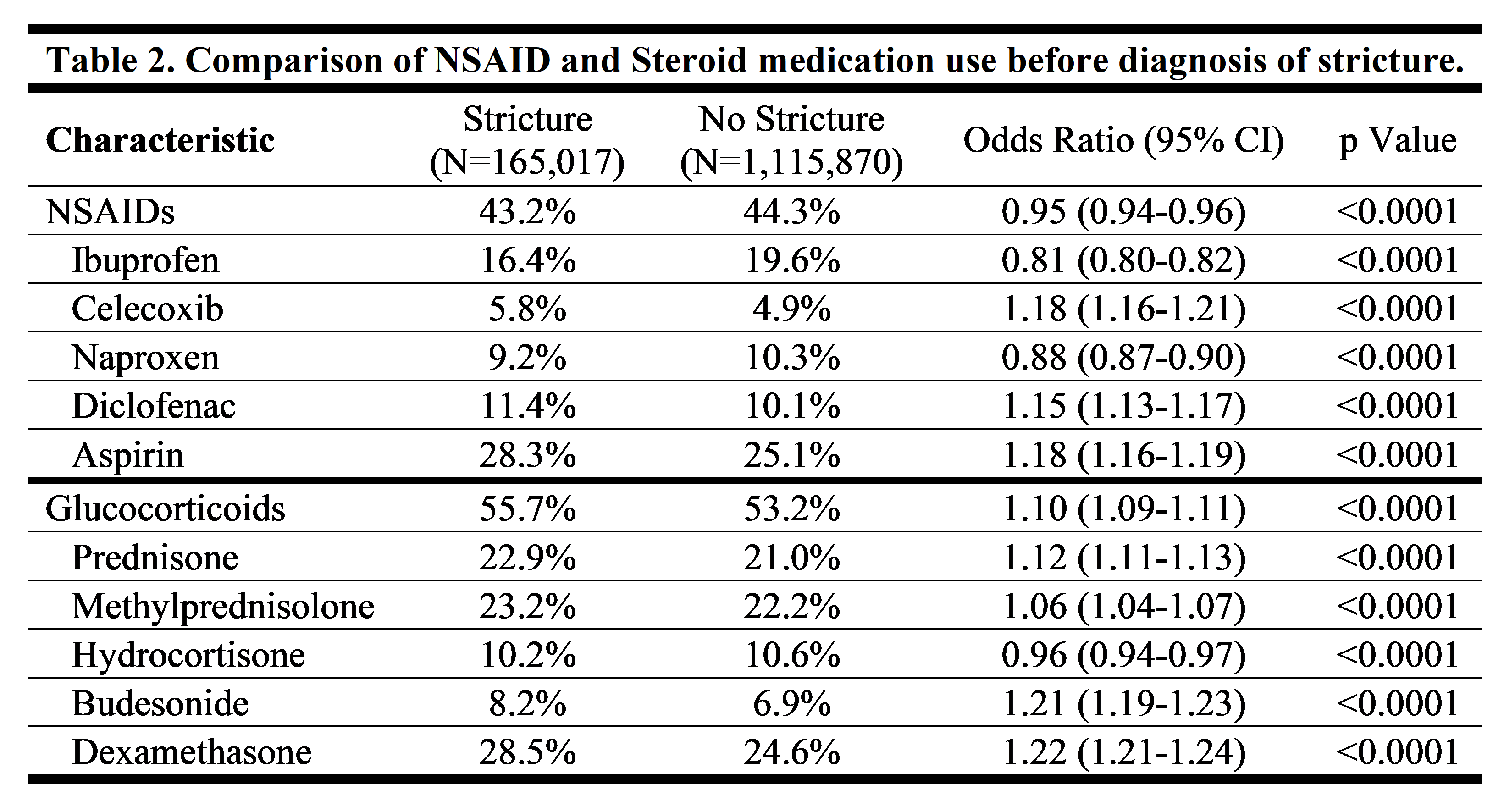
Figure: Table 2. Comparison of NSAID and Steroid medication use before diagnosis of stricture.
Disclosures:
Sven Eriksson indicated no relevant financial relationships.
Inanc Sarici indicated no relevant financial relationships.
Ping Zheng indicated no relevant financial relationships.
Shahin Ayazi indicated no relevant financial relationships.
Sven Eriksson, MD, MS1, Inanc Sarici, MD1, Ping Zheng, MD1, Shahin Ayazi, MD2. P2776 - Clinical and Demographic Predictors of Peptic Stricture: A Cohort Study of Over 5 Million GERD Patients Using a Large US National Health Record Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

