Monday Poster Session
Category: Esophagus
P2768 - Multimodal Assessment of Esophageal Peristalsis in Gastroesophageal Reflux Disease
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Fangfang Wang, MD
Mayo Clinic
Scottsdale, AZ
Presenting Author(s)
Fangfang Wang, MD1, Varan Perananthan, MD2, Andree Koop, MD3, Jennifer Horsley-Silva, MD4, Michael Crowell, PhD1, Ravi Karthik, MD2, Marcelo Vela, MD1
1Mayo Clinic, Scottsdale, AZ; 2Mayo Clinic, Rochester, MN; 3Mayo Clinic, Jacksonville, FL; 4Mayo Clinic Arizona, Scottsdale, AZ
Introduction: Peristalsis is a defense mechanism against GERD by clearing refluxate. Data are limited regarding the relative contributions of primary peristalsis, secondary peristalsis, and peristaltic augmentation in GERD.
Aim: evaluate the association between these peristaltic metrics and GERD via a multimodal approach.
Methods: Retrospectively analyzed patients with esophageal symptoms who underwent FLIP panometry (propofol-sedated, 16 cm balloon), high-resolution manometry (HRM) with multiple rapid swallows (MRS), and reflux monitoring (wireless pH or catheter-based pH-impedance off PPI). GERD was defined as % time pH < 4 (AET) > 6%. Exclusion criteria: achalasia, prior foregut surgery, Botox injection within 6 months, and indeterminate AET (4–6%). Secondary peristalsis was intact if repetitive antegrade contractions were seen on FLIP; EGJ distensibility index (DI) at 60 ml and max diameter at 60–70 ml recorded. Primary peristalsis was impaired if absent contractility or ineffective esophageal motility (IEM) were diagnosed by Chicago Classification v4.0. Post–MRS augmentation was intact if distal contractile integral (DCI) exceeded mean single-swallow DCI. Multimodal peristalsis assessment classified as normal if all 3 metrics (primary and secondary peristalsis, post-MRS augmentation) intact; mild dysfunction if 1 abnormal, severe dysfunction if ≥2 abnormal. Fisher’s exact test and Chi-square used for statistical analysis.
Results: 69 patients included (63% female; mean age 57; mean BMI 26); 22 (31%) had GERD. All had FLIP, 43 had HRM data. GERD was significantly more common (47% vs 19%, p=0.011), and mean AET was significantly higher (8.7% vs 2.7%, p=0.012) with impaired vs intact secondary peristalsis. No association between GERD or AET and DI or EGJ diameter. GERD prevalence was similar with impaired vs intact primary peristalsis (22% vs 32%, p=0.7), numerically higher with impaired vs intact MRS augmentation (39% vs 22%, p=0.3). In multimodal analysis, GERD occurred in 17% with normal peristalsis, 33% with mild, and 43% with severe dysfunction. Mean AET rose with worsening dysfunction (2.2%, 4.5%, 4.6%).
Discussion: Impaired secondary peristalsis was significantly associated with GERD. GERD prevalence and AET are higher with dysfunction on multimodal peristaltic assessment, but not statistically significant likely due to limited sample size. Multimodal peristalsis assessment by FLIP and HRM may enhance understanding of GERD pathophysiology and inform clinical practice, larger studies are needed
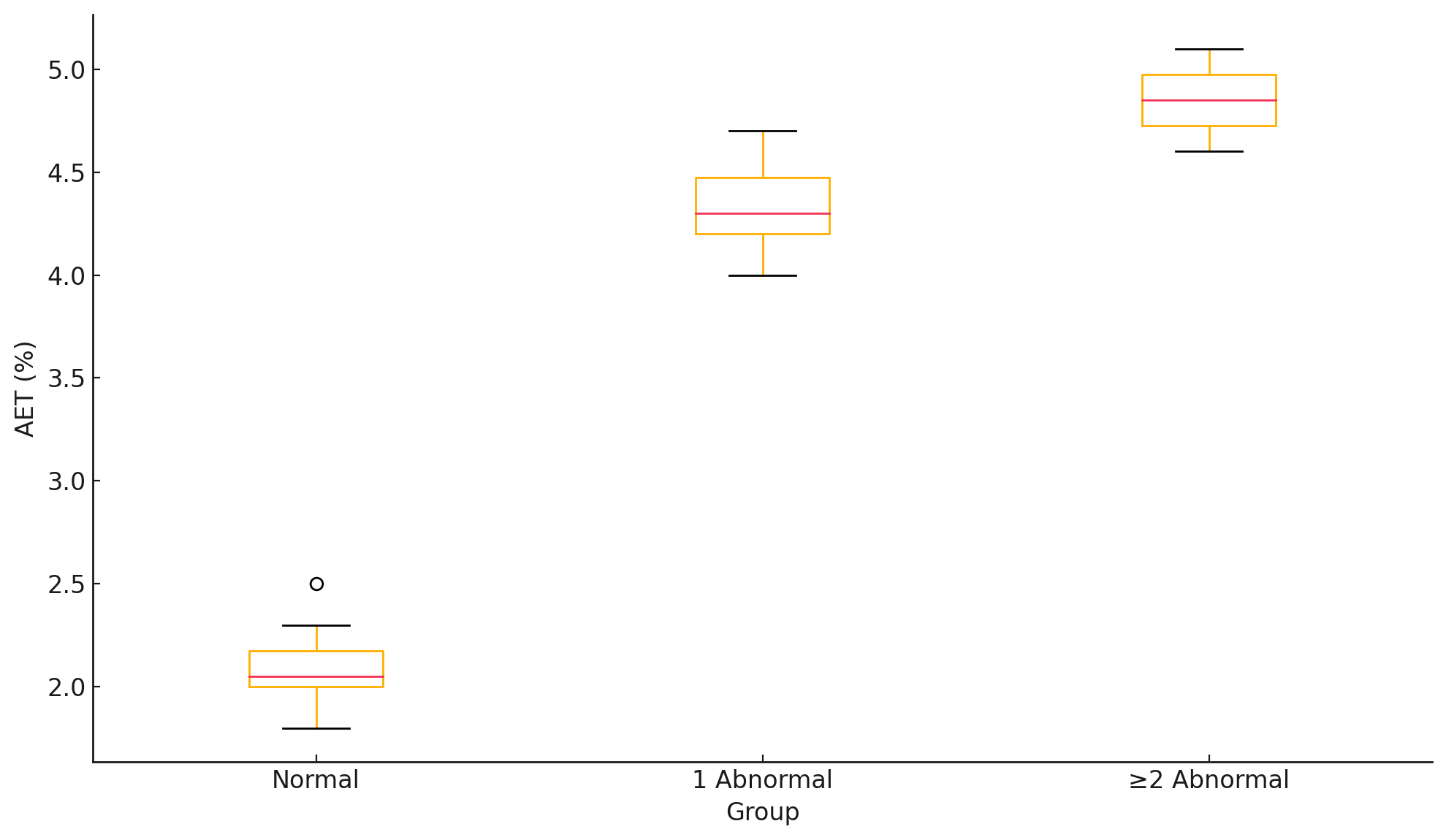
Figure: Mean AET by Multimodal Peristalses Assessment
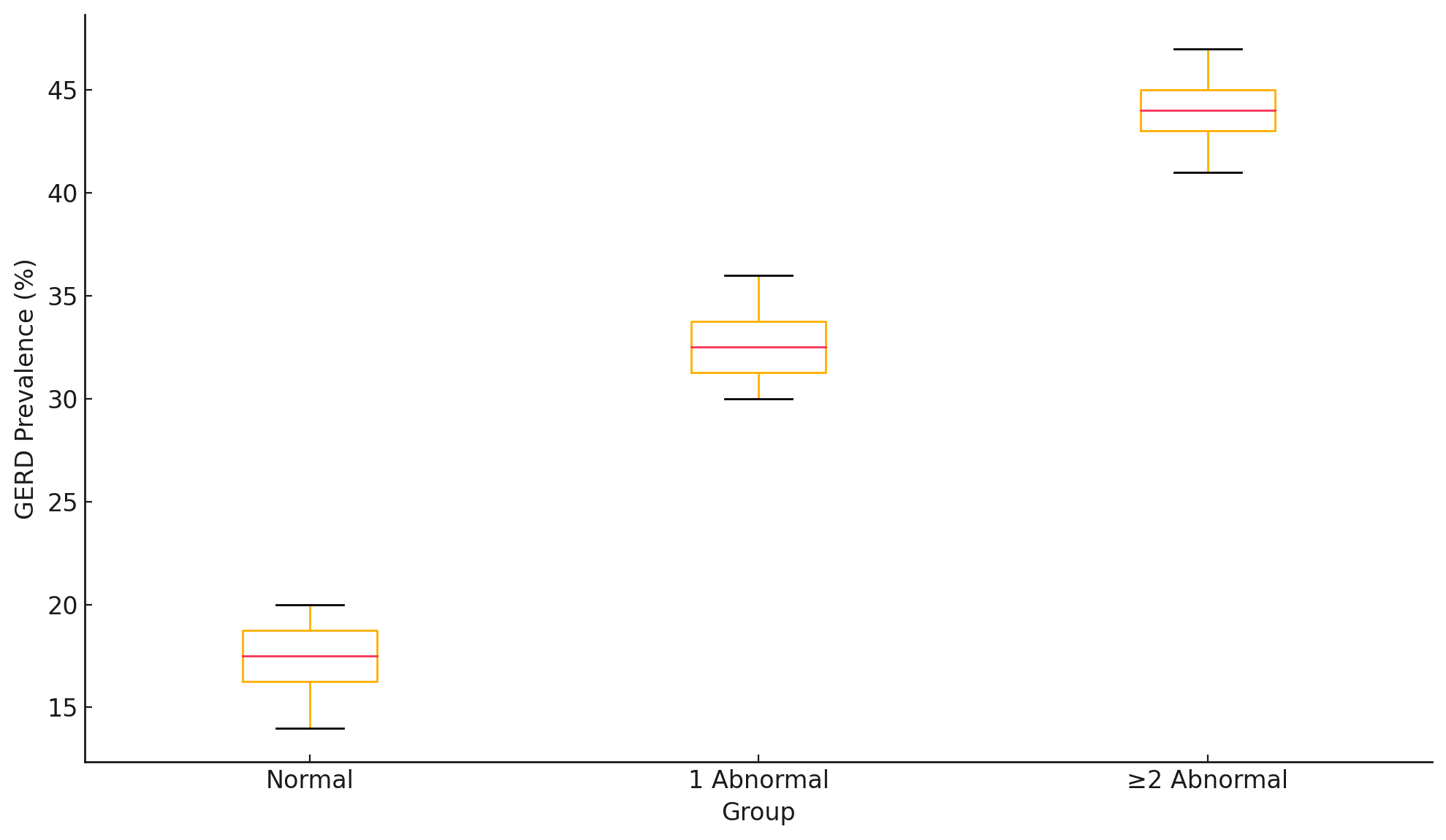
Figure: GERD Prevalence by Multimodal Peristalsis Assessment
Disclosures:
Fangfang Wang indicated no relevant financial relationships.
Varan Perananthan indicated no relevant financial relationships.
Andree Koop indicated no relevant financial relationships.
Jennifer Horsley-Silva indicated no relevant financial relationships.
Michael Crowell indicated no relevant financial relationships.
Ravi Karthik indicated no relevant financial relationships.
Marcelo Vela: Medtronic – Consultant.
Fangfang Wang, MD1, Varan Perananthan, MD2, Andree Koop, MD3, Jennifer Horsley-Silva, MD4, Michael Crowell, PhD1, Ravi Karthik, MD2, Marcelo Vela, MD1. P2768 - Multimodal Assessment of Esophageal Peristalsis in Gastroesophageal Reflux Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mayo Clinic, Scottsdale, AZ; 2Mayo Clinic, Rochester, MN; 3Mayo Clinic, Jacksonville, FL; 4Mayo Clinic Arizona, Scottsdale, AZ
Introduction: Peristalsis is a defense mechanism against GERD by clearing refluxate. Data are limited regarding the relative contributions of primary peristalsis, secondary peristalsis, and peristaltic augmentation in GERD.
Aim: evaluate the association between these peristaltic metrics and GERD via a multimodal approach.
Methods: Retrospectively analyzed patients with esophageal symptoms who underwent FLIP panometry (propofol-sedated, 16 cm balloon), high-resolution manometry (HRM) with multiple rapid swallows (MRS), and reflux monitoring (wireless pH or catheter-based pH-impedance off PPI). GERD was defined as % time pH < 4 (AET) > 6%. Exclusion criteria: achalasia, prior foregut surgery, Botox injection within 6 months, and indeterminate AET (4–6%). Secondary peristalsis was intact if repetitive antegrade contractions were seen on FLIP; EGJ distensibility index (DI) at 60 ml and max diameter at 60–70 ml recorded. Primary peristalsis was impaired if absent contractility or ineffective esophageal motility (IEM) were diagnosed by Chicago Classification v4.0. Post–MRS augmentation was intact if distal contractile integral (DCI) exceeded mean single-swallow DCI. Multimodal peristalsis assessment classified as normal if all 3 metrics (primary and secondary peristalsis, post-MRS augmentation) intact; mild dysfunction if 1 abnormal, severe dysfunction if ≥2 abnormal. Fisher’s exact test and Chi-square used for statistical analysis.
Results: 69 patients included (63% female; mean age 57; mean BMI 26); 22 (31%) had GERD. All had FLIP, 43 had HRM data. GERD was significantly more common (47% vs 19%, p=0.011), and mean AET was significantly higher (8.7% vs 2.7%, p=0.012) with impaired vs intact secondary peristalsis. No association between GERD or AET and DI or EGJ diameter. GERD prevalence was similar with impaired vs intact primary peristalsis (22% vs 32%, p=0.7), numerically higher with impaired vs intact MRS augmentation (39% vs 22%, p=0.3). In multimodal analysis, GERD occurred in 17% with normal peristalsis, 33% with mild, and 43% with severe dysfunction. Mean AET rose with worsening dysfunction (2.2%, 4.5%, 4.6%).
Discussion: Impaired secondary peristalsis was significantly associated with GERD. GERD prevalence and AET are higher with dysfunction on multimodal peristaltic assessment, but not statistically significant likely due to limited sample size. Multimodal peristalsis assessment by FLIP and HRM may enhance understanding of GERD pathophysiology and inform clinical practice, larger studies are needed
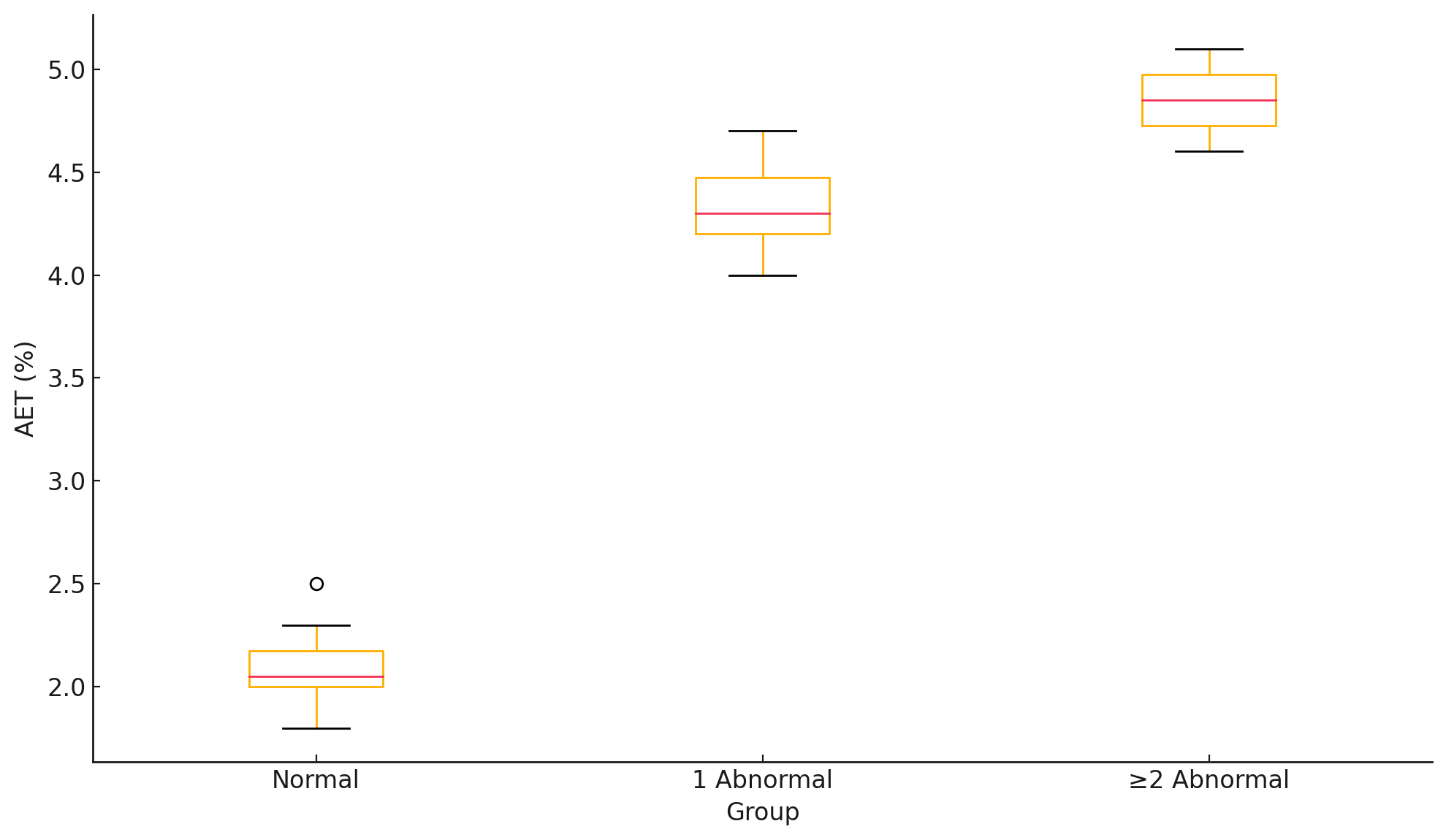
Figure: Mean AET by Multimodal Peristalses Assessment
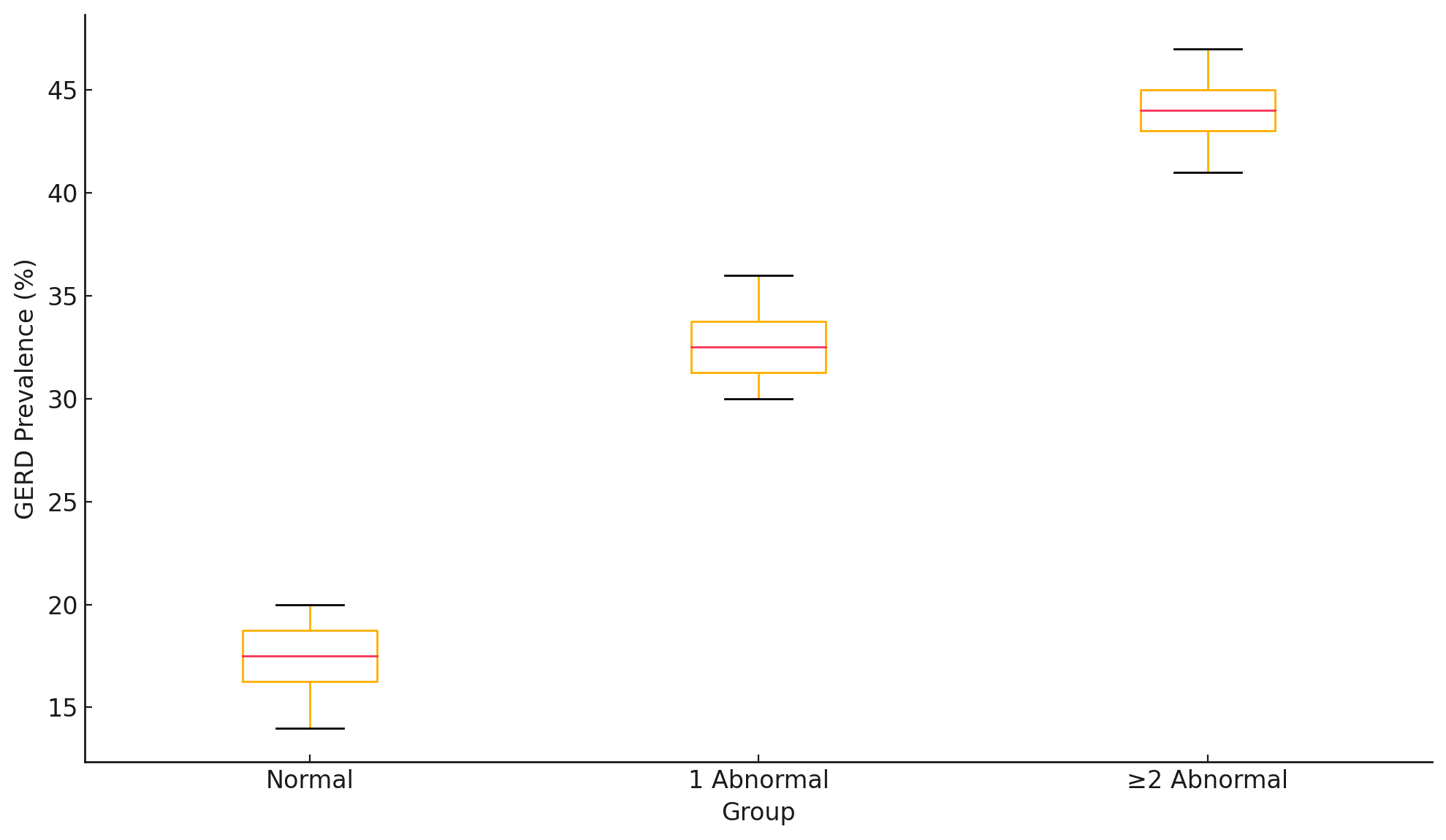
Figure: GERD Prevalence by Multimodal Peristalsis Assessment
Disclosures:
Fangfang Wang indicated no relevant financial relationships.
Varan Perananthan indicated no relevant financial relationships.
Andree Koop indicated no relevant financial relationships.
Jennifer Horsley-Silva indicated no relevant financial relationships.
Michael Crowell indicated no relevant financial relationships.
Ravi Karthik indicated no relevant financial relationships.
Marcelo Vela: Medtronic – Consultant.
Fangfang Wang, MD1, Varan Perananthan, MD2, Andree Koop, MD3, Jennifer Horsley-Silva, MD4, Michael Crowell, PhD1, Ravi Karthik, MD2, Marcelo Vela, MD1. P2768 - Multimodal Assessment of Esophageal Peristalsis in Gastroesophageal Reflux Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
