Monday Poster Session
Category: Diet, Nutrition, and Obesity
P2689 - Prior Bariatric Surgery Increases the Risk of Adverse Outcomes in Alcohol-Associated Hepatitis Patients: A Nationwide Propensity Matched Cohort Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Shu-Yen Emily Chan, MD (she/her/hers)
Weiss Memorial Hospital
Nashville, TN
Presenting Author(s)
Emily Shu-Yen Chan, MD1, Natchaya Polpichai, MD2, Patrick Twohig, MD3
1Weiss Memorial Hospital, Chicago, IL; 2Division of gastroenterology/hepatology, Medical College of Georgia at Augusta University, Chicago, IL; 3University of Rochester Medical Center, Rochester, NY
Introduction: Alcohol‐associated liver disease (ALD) is increasing alongside the expanding use of bariatric surgery (BS) for obesity. Although prior studies links BS to higher risks of alcohol use disorder and ALD, its impact on outcomes among patients with alcohol‐associated hepatitis (AH) remains unclear.
Methods: We conducted a retrospective cohort study using de‑identified TriNetX records from 67 healthcare organizations including 113 million patients. Adults diagnosed with AH from 1/1/2014 to 12/31/ 2023 were included. Those with a prior history of BS were 1:1 propensity score matched to AH patients without BS (n = 2,786 per group). Matching variables included demographics, comorbidities, baseline labs values and medication use. The primary endpoint was five‐year all‐cause mortality. Secondary endpoints were rates of hospitalization, sepsis, hepatic encephalopathy (HE), variceal bleeding, ascites, spontaneous bacterial peritonitis (SBP), hepatorenal syndrome, acute kidney injury (AKI), acute respiratory distress syndrome (ARDS), and requirement for mechanical ventilation. Adjusted hazard ratios (aHRs) and 95% CIs were derived using Cox proportional hazards models. Overall and event‐free survival were estimated via Kaplan–Meier curves, with differences assessed by log‐rank testing.
Results: After PSM, AH patients with prior BS exhibited significantly higher risks across multiple outcomes compared with those without BS, including all-cause mortality (aHR:1.115, 95%CI: 1.005-1.238, log rank p=0.04), hospitalization rate (aHR:1.135, 95%CI: 1.006-1.209, log rank p< 0.001), sepsis (aHR:1.143, 95%CI: 1.027-1.273, log rank p=0.014), HE (aHR:1.231, 95%CI: 1.131-1.340, log rank p< 0.001), ascites (aHR:1.136, 95%CI: 1.048-1.231, log rank p=0.002), AKI (aHR:1.137, 95%CI: 1.043-1.239, log rank p=0.004), ARDS (aHR:1.128, 95%CI: 1.010-1.260, log rank p=0.032), and mechanical ventilation use (aHR:1.183, 95%CI: 1.011-1.383, log rank p=0.035). Yet, no significant differences were observed in the risk of variceal bleeding (aHR:1.063, 95%CI: 0.937-1.206), SBP (aHR:1.140, 95%CI: 0.941-1.381) or hepatorenal syndrome (aHR:1.163, 95%CI: 0.994-1.360).
Discussion: Prior BS in patients with AH is linked to higher risks of cirrhosis decompensation, sepsis, AKI, overall mortality, and hospitalization compared with those without BS. All post‐bariatric patients, even without prior alcohol use disorder, should receive counseling on their increased risk of alcohol misuse and ALD be monitored long term for related complications.
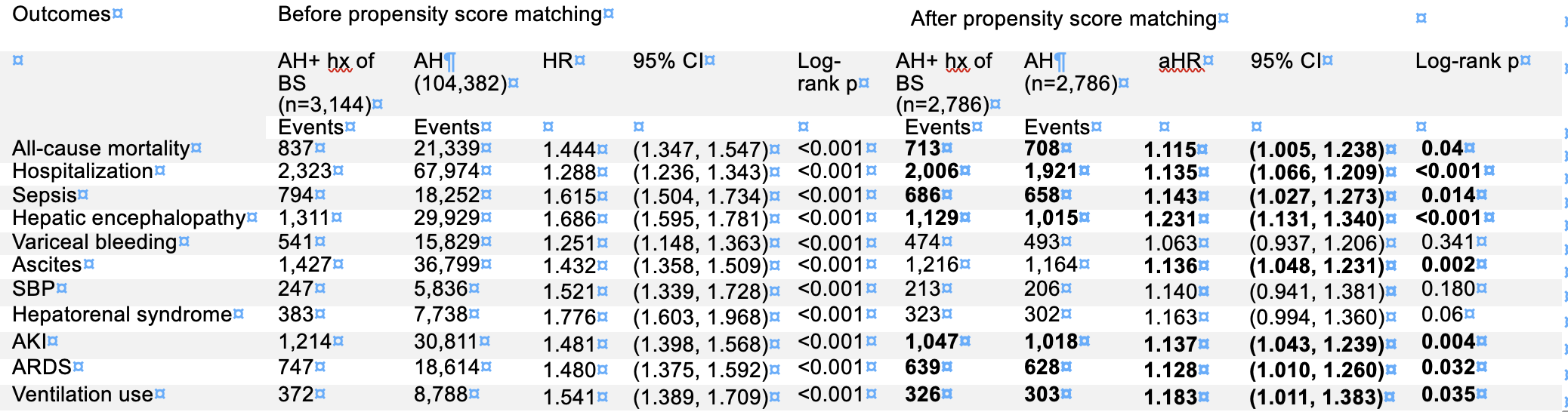
Figure: Table 1. Outcomes in AH patients with vs without prior bariatric surgery
Disclosures:
Emily Shu-Yen Chan indicated no relevant financial relationships.
Natchaya Polpichai indicated no relevant financial relationships.
Patrick Twohig indicated no relevant financial relationships.
Emily Shu-Yen Chan, MD1, Natchaya Polpichai, MD2, Patrick Twohig, MD3. P2689 - Prior Bariatric Surgery Increases the Risk of Adverse Outcomes in Alcohol-Associated Hepatitis Patients: A Nationwide Propensity Matched Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Weiss Memorial Hospital, Chicago, IL; 2Division of gastroenterology/hepatology, Medical College of Georgia at Augusta University, Chicago, IL; 3University of Rochester Medical Center, Rochester, NY
Introduction: Alcohol‐associated liver disease (ALD) is increasing alongside the expanding use of bariatric surgery (BS) for obesity. Although prior studies links BS to higher risks of alcohol use disorder and ALD, its impact on outcomes among patients with alcohol‐associated hepatitis (AH) remains unclear.
Methods: We conducted a retrospective cohort study using de‑identified TriNetX records from 67 healthcare organizations including 113 million patients. Adults diagnosed with AH from 1/1/2014 to 12/31/ 2023 were included. Those with a prior history of BS were 1:1 propensity score matched to AH patients without BS (n = 2,786 per group). Matching variables included demographics, comorbidities, baseline labs values and medication use. The primary endpoint was five‐year all‐cause mortality. Secondary endpoints were rates of hospitalization, sepsis, hepatic encephalopathy (HE), variceal bleeding, ascites, spontaneous bacterial peritonitis (SBP), hepatorenal syndrome, acute kidney injury (AKI), acute respiratory distress syndrome (ARDS), and requirement for mechanical ventilation. Adjusted hazard ratios (aHRs) and 95% CIs were derived using Cox proportional hazards models. Overall and event‐free survival were estimated via Kaplan–Meier curves, with differences assessed by log‐rank testing.
Results: After PSM, AH patients with prior BS exhibited significantly higher risks across multiple outcomes compared with those without BS, including all-cause mortality (aHR:1.115, 95%CI: 1.005-1.238, log rank p=0.04), hospitalization rate (aHR:1.135, 95%CI: 1.006-1.209, log rank p< 0.001), sepsis (aHR:1.143, 95%CI: 1.027-1.273, log rank p=0.014), HE (aHR:1.231, 95%CI: 1.131-1.340, log rank p< 0.001), ascites (aHR:1.136, 95%CI: 1.048-1.231, log rank p=0.002), AKI (aHR:1.137, 95%CI: 1.043-1.239, log rank p=0.004), ARDS (aHR:1.128, 95%CI: 1.010-1.260, log rank p=0.032), and mechanical ventilation use (aHR:1.183, 95%CI: 1.011-1.383, log rank p=0.035). Yet, no significant differences were observed in the risk of variceal bleeding (aHR:1.063, 95%CI: 0.937-1.206), SBP (aHR:1.140, 95%CI: 0.941-1.381) or hepatorenal syndrome (aHR:1.163, 95%CI: 0.994-1.360).
Discussion: Prior BS in patients with AH is linked to higher risks of cirrhosis decompensation, sepsis, AKI, overall mortality, and hospitalization compared with those without BS. All post‐bariatric patients, even without prior alcohol use disorder, should receive counseling on their increased risk of alcohol misuse and ALD be monitored long term for related complications.
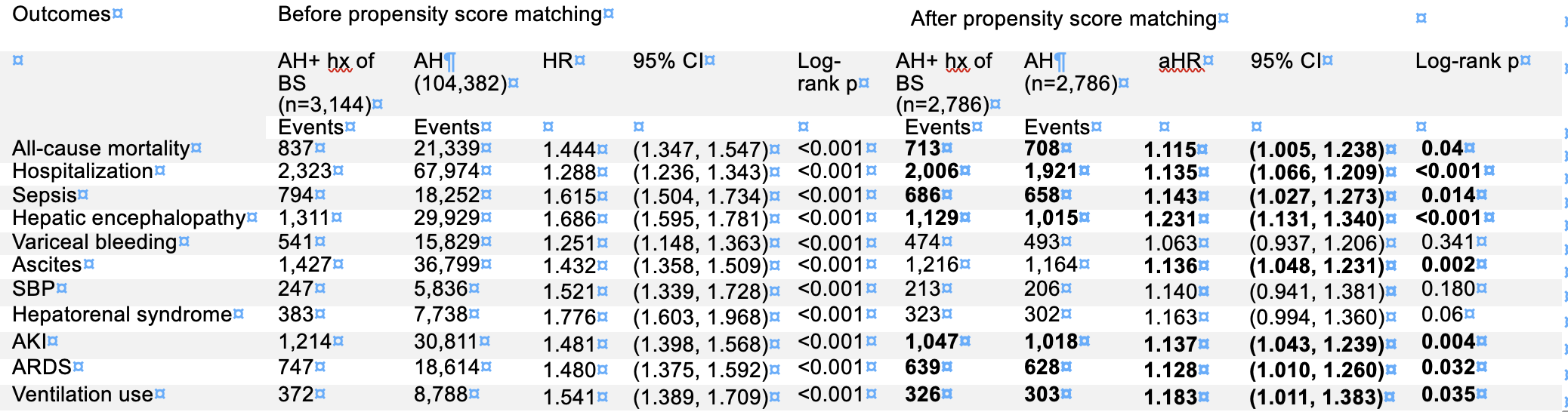
Figure: Table 1. Outcomes in AH patients with vs without prior bariatric surgery
Disclosures:
Emily Shu-Yen Chan indicated no relevant financial relationships.
Natchaya Polpichai indicated no relevant financial relationships.
Patrick Twohig indicated no relevant financial relationships.
Emily Shu-Yen Chan, MD1, Natchaya Polpichai, MD2, Patrick Twohig, MD3. P2689 - Prior Bariatric Surgery Increases the Risk of Adverse Outcomes in Alcohol-Associated Hepatitis Patients: A Nationwide Propensity Matched Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
