Monday Poster Session
Category: Diet, Nutrition, and Obesity
P2680 - Investigating the Prescription Patterns of GLP-1 Receptor Agonist Medications in Patients With Chronic Pancreatitis and Obesity
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- KP
Karthic Drishna Perumal, MD
Mount Carmel Health System
Powell, OH
Presenting Author(s)
Karthic Drishna Perumal, MD1, Thomas Mathews, MD2, Richard Maradiaga, MD3, Thomas R. McCarty, MD, MPH4, Raj Shah, MD3
1Mount Carmel Health System, Powell, OH; 2University of Kentucky, Lexington, KY; 3The Ohio State University Wexner Medical Center, Columbus, OH; 4Houston Methodist Hospital, Houston, TX
Introduction: Glucagon-like peptide-1 receptor agonists (GLP-1) have shown significant efficacy in managing obesity. However, some patients experience complications that limit their therapeutic benefits, including pancreatitis. While acute pancreatitis (AP) has been reported in association with GLP-1 use, a direct causal relationship remains unconfirmed. However, recurrent episodes of AP may progress to chronic pancreatitis (CP). Our study aims to evaluate the prevalence of obesity among patients with CP, the frequency of GLP-1 RA prescriptions in this cohort, and their healthcare utilization patterns.
Methods: We conducted a retrospective study utilizing the SlicerDicer database within the Epic electronic health record at a single, tertiary care referral center in the United States. The study period spanned November 2019 to November 2024. Inclusion criteria included patients with a prior CP diagnosis and those newly diagnosed with obesity within this timeframe. The dataset was refined to individuals prescribed a GLP-1—specifically semaglutide, tirzepatide, or liraglutide—within 12 months of their obesity diagnosis. Statistical analyses were performed using chi-square testing.
Results: Among 3,388 patients with CP, 19% (n=659) were diagnosed with obesity at a later clinical encounter. Of these, 15% (n=100) were prescribed a GLP-1, totaling 124 new prescriptions. Semaglutide was the most frequently prescribed (58%), followed by tirzepatide (31%) and liraglutide (11%). Patients using GLP-1 RAs demonstrated significantly higher healthcare utilization than non-GLP-1 users, with emergency department visits averaging 6 vs. 3.7 per patient (p< 0.001) and hospital admissions averaging 4.1 vs. 3.2 per patient (p< 0.001) over five years.
Discussion: Our study highlights the clinical complexity in managing obesity in individuals with CP. While 19% of CP patients were diagnosed with obesity, only 15% received a GLP-1 prescription, suggesting potential provider hesitancy due to concerns of AP. Increased healthcare utilization among GLP-1 users highlights the need for closer monitoring and the development of tailored approaches to identify predictive markers for individuals at increased risk of CP complications. Future longitudinal studies are required to elucidate the safety profile of GLP-1s in patients with CP and obesity in order to develop personalized obesity management strategies, while minimizing adverse effects and ensuring the maximum therapeutic benefit of GLP-1s in this population.
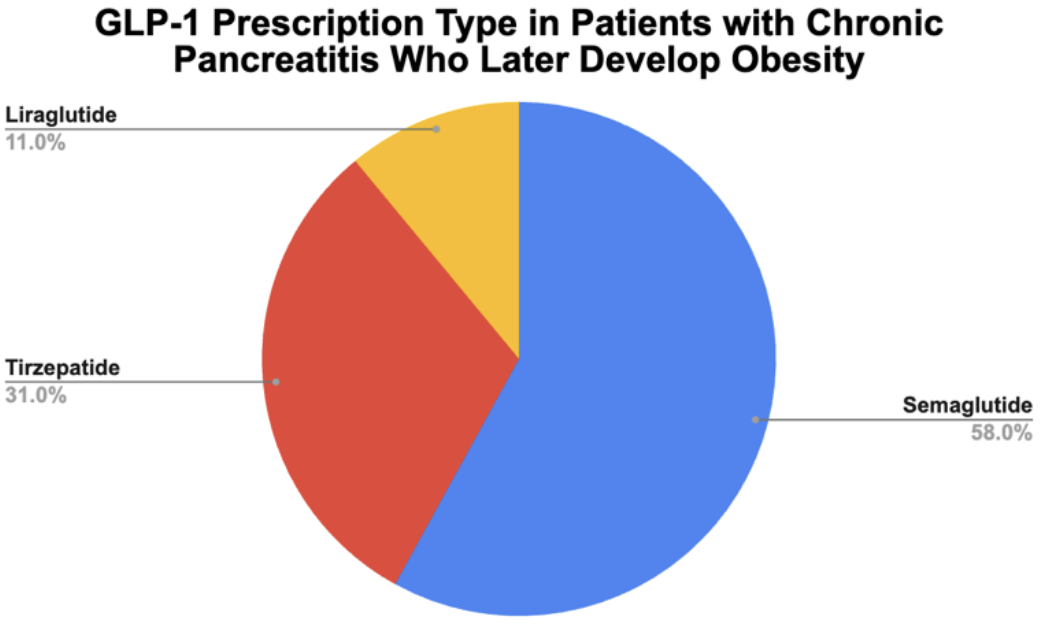
Figure: Figure 1: Rate of the type of GLP-1 medication prescriptions seen in patients with chronic pancreatitis who later developed and were subsequently diagnosed with obesity.
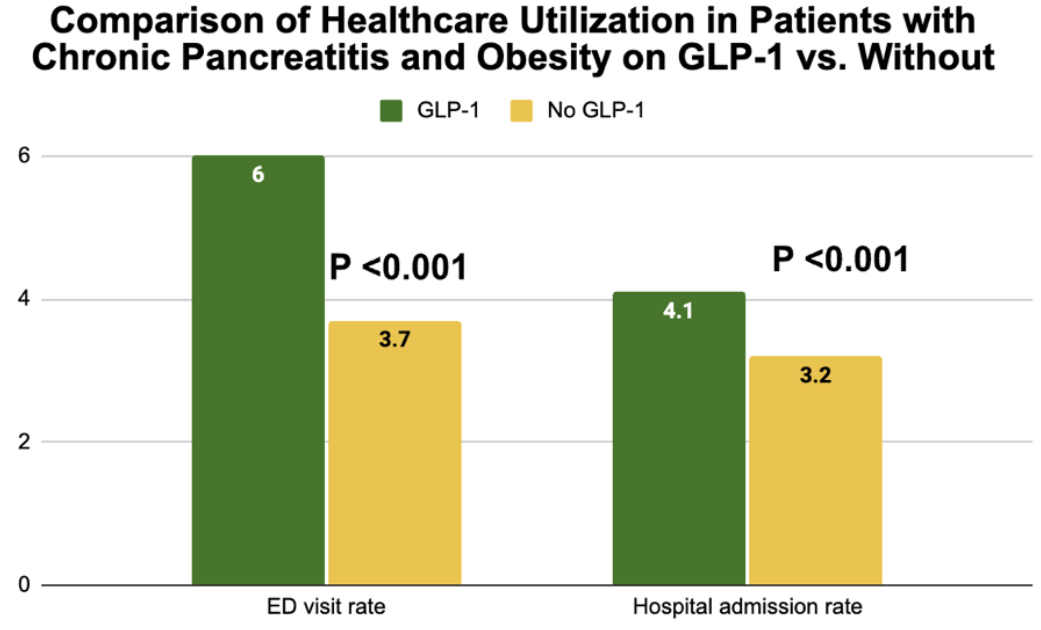
Figure: Figure 2: Comparison of healthcare utilization including both emergency department visits and hospitalization admissions amongst patients with chronic pancreatitis who were diagnosed with obesity and prescribed a GLP-1 medication vs those who were no prescribed a GLP-1 medication.
Disclosures:
Karthic Drishna Perumal indicated no relevant financial relationships.
Thomas Mathews indicated no relevant financial relationships.
Richard Maradiaga indicated no relevant financial relationships.
Thomas McCarty: Covidien/Medtronic – Consultant. Endoquest Robotics – Consultant.
Raj Shah indicated no relevant financial relationships.
Karthic Drishna Perumal, MD1, Thomas Mathews, MD2, Richard Maradiaga, MD3, Thomas R. McCarty, MD, MPH4, Raj Shah, MD3. P2680 - Investigating the Prescription Patterns of GLP-1 Receptor Agonist Medications in Patients With Chronic Pancreatitis and Obesity, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mount Carmel Health System, Powell, OH; 2University of Kentucky, Lexington, KY; 3The Ohio State University Wexner Medical Center, Columbus, OH; 4Houston Methodist Hospital, Houston, TX
Introduction: Glucagon-like peptide-1 receptor agonists (GLP-1) have shown significant efficacy in managing obesity. However, some patients experience complications that limit their therapeutic benefits, including pancreatitis. While acute pancreatitis (AP) has been reported in association with GLP-1 use, a direct causal relationship remains unconfirmed. However, recurrent episodes of AP may progress to chronic pancreatitis (CP). Our study aims to evaluate the prevalence of obesity among patients with CP, the frequency of GLP-1 RA prescriptions in this cohort, and their healthcare utilization patterns.
Methods: We conducted a retrospective study utilizing the SlicerDicer database within the Epic electronic health record at a single, tertiary care referral center in the United States. The study period spanned November 2019 to November 2024. Inclusion criteria included patients with a prior CP diagnosis and those newly diagnosed with obesity within this timeframe. The dataset was refined to individuals prescribed a GLP-1—specifically semaglutide, tirzepatide, or liraglutide—within 12 months of their obesity diagnosis. Statistical analyses were performed using chi-square testing.
Results: Among 3,388 patients with CP, 19% (n=659) were diagnosed with obesity at a later clinical encounter. Of these, 15% (n=100) were prescribed a GLP-1, totaling 124 new prescriptions. Semaglutide was the most frequently prescribed (58%), followed by tirzepatide (31%) and liraglutide (11%). Patients using GLP-1 RAs demonstrated significantly higher healthcare utilization than non-GLP-1 users, with emergency department visits averaging 6 vs. 3.7 per patient (p< 0.001) and hospital admissions averaging 4.1 vs. 3.2 per patient (p< 0.001) over five years.
Discussion: Our study highlights the clinical complexity in managing obesity in individuals with CP. While 19% of CP patients were diagnosed with obesity, only 15% received a GLP-1 prescription, suggesting potential provider hesitancy due to concerns of AP. Increased healthcare utilization among GLP-1 users highlights the need for closer monitoring and the development of tailored approaches to identify predictive markers for individuals at increased risk of CP complications. Future longitudinal studies are required to elucidate the safety profile of GLP-1s in patients with CP and obesity in order to develop personalized obesity management strategies, while minimizing adverse effects and ensuring the maximum therapeutic benefit of GLP-1s in this population.
Figure: Figure 1: Rate of the type of GLP-1 medication prescriptions seen in patients with chronic pancreatitis who later developed and were subsequently diagnosed with obesity.
Figure: Figure 2: Comparison of healthcare utilization including both emergency department visits and hospitalization admissions amongst patients with chronic pancreatitis who were diagnosed with obesity and prescribed a GLP-1 medication vs those who were no prescribed a GLP-1 medication.
Disclosures:
Karthic Drishna Perumal indicated no relevant financial relationships.
Thomas Mathews indicated no relevant financial relationships.
Richard Maradiaga indicated no relevant financial relationships.
Thomas McCarty: Covidien/Medtronic – Consultant. Endoquest Robotics – Consultant.
Raj Shah indicated no relevant financial relationships.
Karthic Drishna Perumal, MD1, Thomas Mathews, MD2, Richard Maradiaga, MD3, Thomas R. McCarty, MD, MPH4, Raj Shah, MD3. P2680 - Investigating the Prescription Patterns of GLP-1 Receptor Agonist Medications in Patients With Chronic Pancreatitis and Obesity, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
