Monday Poster Session
Category: Diet, Nutrition, and Obesity
P2679 - Intermittent Fasting, Gut Microbiome Composition, and Metabolic Health: A 3-Week Intervention in Patients With Prediabetes and Type 2 Diabetes Mellitus
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- KP
Karthic Drishna Perumal, MD
Mount Carmel Health System
Powell, OH
Presenting Author(s)
Karthic Drishna Perumal, MD1, Frank Epitropoulos, MD2, Sumit Sharma, MD2, Tammy Aubel, BSN, RN2, Ann Salvator, MS2
1Mount Carmel Health System, Powell, OH; 2Mount Carmel Health System, Grove City, OH
Introduction: The gut microbiome plays a vital role in metabolic regulation, immune function, and inflammation control, particularly in individuals with prediabetes and Type 2 Diabetes Mellitus (T2DM). Intermittent Fasting (IF) and Time-Restricted Eating (TRE) are cost-effective strategies that align food intake with circadian biology, potentially improving metabolic health. However, limited clinical data exist regarding their effects on microbial diversity, systemic inflammation, and metabolic biomarkers.
Methods: This pilot study enrolled ten adults with prediabetes or T2DM from a community outpatient internal medicine clinic, excluding individuals on weight-affecting medications, restrictive diets, or recent antibiotic use. Participants followed a 3-week IF regimen with an 8-hour eating window (12 PM–8 PM) and a 16-hour fasting period, without macronutrient restrictions. Pre- and post-intervention assessments included fasting insulin and leptin levels, inflammatory cytokines (TNF-alpha, IL-6), omega fatty acid panels, and gut microbiome profiling via 16S rRNA sequencing with stool samples were also measured.
Results: Eight participants completed the protocol. IF resulted in a 63% reduction in fasting insulin (mean 24.9 to 9.3 μIU/mL) and a decrease in leptin (7.3 to 5.7 ng/mL), suggesting improved insulin sensitivity and satiety signaling. The omega-6/omega-3 ratio declined, indicating a shift away from a pro-inflammatory state. Microbiome analysis showed high diversity (Simpson Index ~0.99), primarily Firmicutes and Bacteroidetes, with functional genomic shifts in glycolysis and gluconeogenesis. Higher microbial diversity correlated with increased butyrate levels, supporting gut barrier integrity and reduced inflammation. Some patients exhibited elevated isobutyric and isovaleric acids, potentially indicating dysbiosis. The Firmicutes/Bacteroidetes (F/B) ratio remained key, with higher ratios linked to insulin resistance and inflammation, while lower ratios correlated with improved metabolic profiles.
Discussion: These findings highlight IF’s potential in modulating gut microbiota and metabolic markers. IF-induced shifts favored beneficial bacterial populations, supporting prior evidence on high-fiber, Mediterranean-style diets. Despite the small sample, results suggest IF enhances glucose regulation, lipid profiles, and microbial balance. Larger studies with extended follow-up and dietary monitoring are needed to validate these findings.
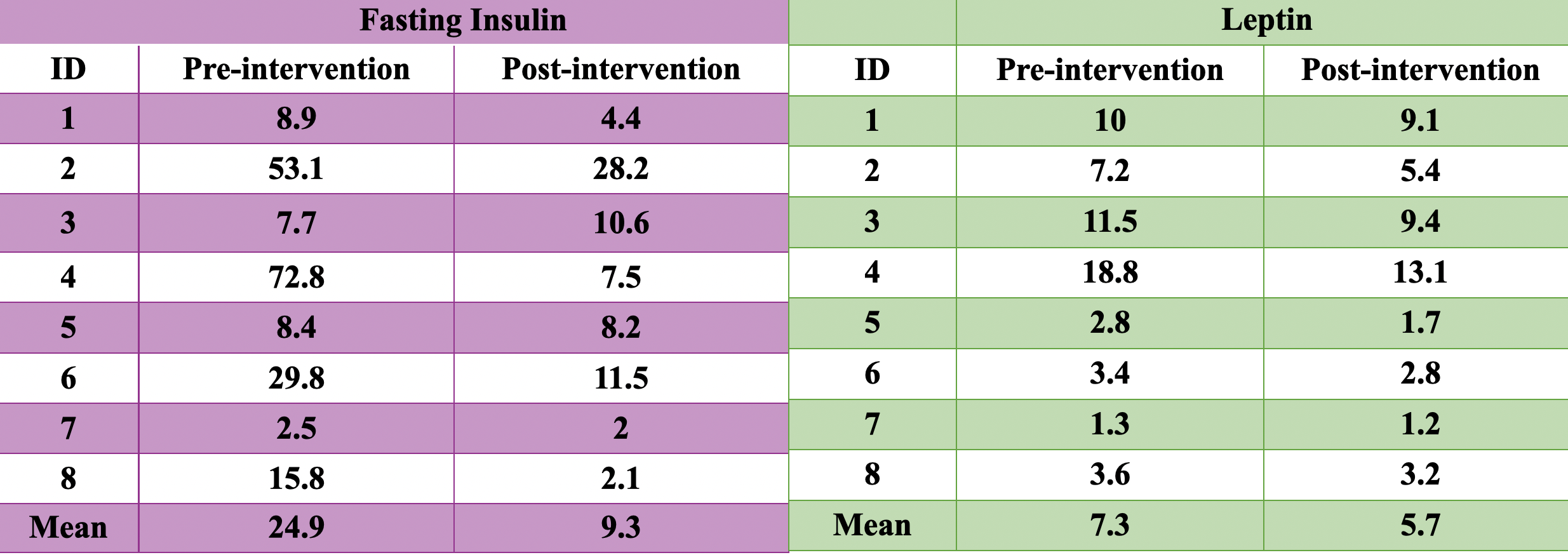
Figure: Table 1: The purple table shows the changes in fasting insulin levels pre and post-3-week intervention, while the green table displays the changes in leptin levels pre and post-3-week intervention. Both fasting insulin and leptin levels are shown to decrease after 3 weeks of intermittent fasting and timed restricted eating.
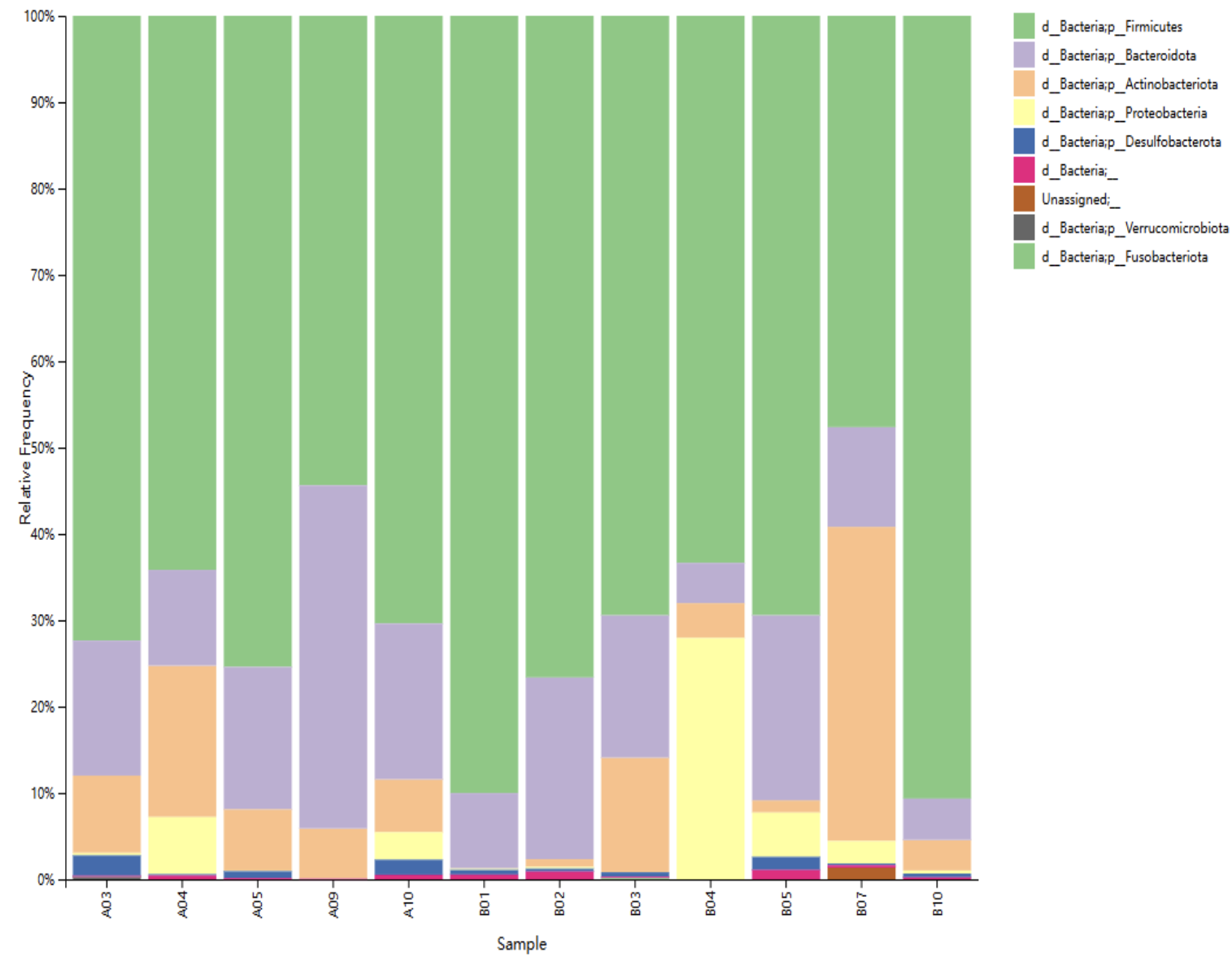
Figure: Figure 1: The taxonomy distribution of all samples at the Phylum classification level. Firmicutes and Bacteroidetes occupied most phyla in the gut microbiota, correlating with the green and purple colors as indicated by the legend on the top right.
Disclosures:
Karthic Drishna Perumal indicated no relevant financial relationships.
Frank Epitropoulos indicated no relevant financial relationships.
Sumit Sharma indicated no relevant financial relationships.
Tammy Aubel indicated no relevant financial relationships.
Ann Salvator indicated no relevant financial relationships.
Karthic Drishna Perumal, MD1, Frank Epitropoulos, MD2, Sumit Sharma, MD2, Tammy Aubel, BSN, RN2, Ann Salvator, MS2. P2679 - Intermittent Fasting, Gut Microbiome Composition, and Metabolic Health: A 3-Week Intervention in Patients With Prediabetes and Type 2 Diabetes Mellitus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mount Carmel Health System, Powell, OH; 2Mount Carmel Health System, Grove City, OH
Introduction: The gut microbiome plays a vital role in metabolic regulation, immune function, and inflammation control, particularly in individuals with prediabetes and Type 2 Diabetes Mellitus (T2DM). Intermittent Fasting (IF) and Time-Restricted Eating (TRE) are cost-effective strategies that align food intake with circadian biology, potentially improving metabolic health. However, limited clinical data exist regarding their effects on microbial diversity, systemic inflammation, and metabolic biomarkers.
Methods: This pilot study enrolled ten adults with prediabetes or T2DM from a community outpatient internal medicine clinic, excluding individuals on weight-affecting medications, restrictive diets, or recent antibiotic use. Participants followed a 3-week IF regimen with an 8-hour eating window (12 PM–8 PM) and a 16-hour fasting period, without macronutrient restrictions. Pre- and post-intervention assessments included fasting insulin and leptin levels, inflammatory cytokines (TNF-alpha, IL-6), omega fatty acid panels, and gut microbiome profiling via 16S rRNA sequencing with stool samples were also measured.
Results: Eight participants completed the protocol. IF resulted in a 63% reduction in fasting insulin (mean 24.9 to 9.3 μIU/mL) and a decrease in leptin (7.3 to 5.7 ng/mL), suggesting improved insulin sensitivity and satiety signaling. The omega-6/omega-3 ratio declined, indicating a shift away from a pro-inflammatory state. Microbiome analysis showed high diversity (Simpson Index ~0.99), primarily Firmicutes and Bacteroidetes, with functional genomic shifts in glycolysis and gluconeogenesis. Higher microbial diversity correlated with increased butyrate levels, supporting gut barrier integrity and reduced inflammation. Some patients exhibited elevated isobutyric and isovaleric acids, potentially indicating dysbiosis. The Firmicutes/Bacteroidetes (F/B) ratio remained key, with higher ratios linked to insulin resistance and inflammation, while lower ratios correlated with improved metabolic profiles.
Discussion: These findings highlight IF’s potential in modulating gut microbiota and metabolic markers. IF-induced shifts favored beneficial bacterial populations, supporting prior evidence on high-fiber, Mediterranean-style diets. Despite the small sample, results suggest IF enhances glucose regulation, lipid profiles, and microbial balance. Larger studies with extended follow-up and dietary monitoring are needed to validate these findings.
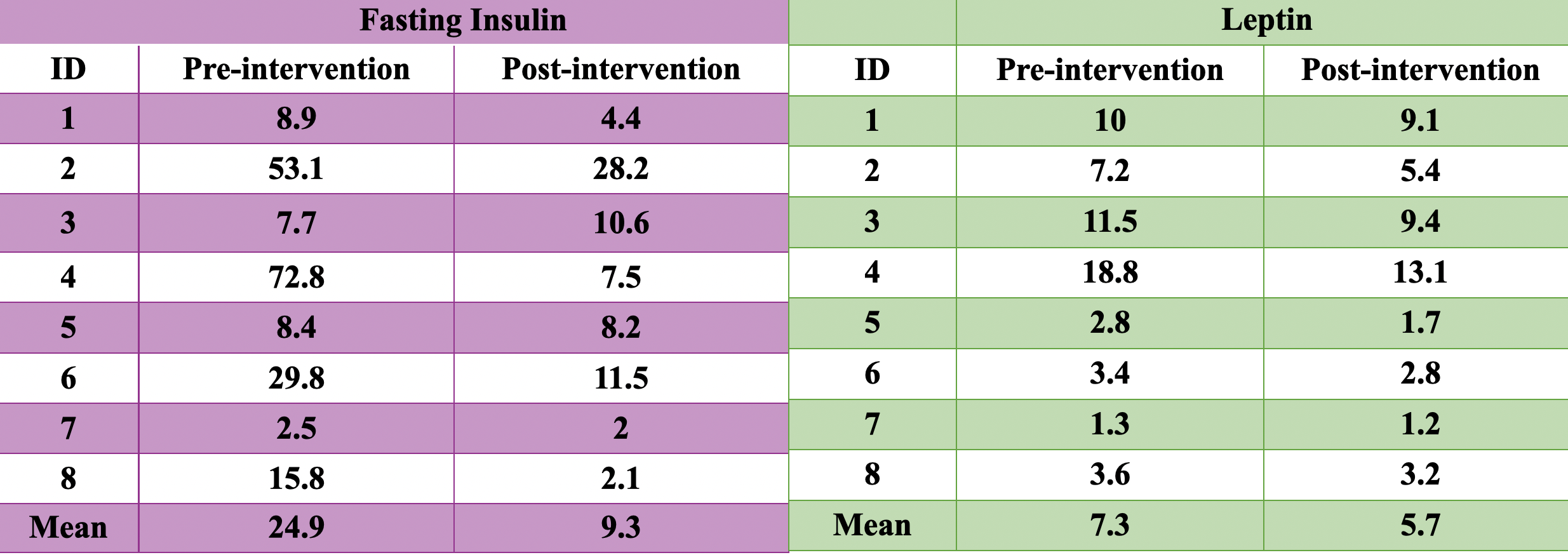
Figure: Table 1: The purple table shows the changes in fasting insulin levels pre and post-3-week intervention, while the green table displays the changes in leptin levels pre and post-3-week intervention. Both fasting insulin and leptin levels are shown to decrease after 3 weeks of intermittent fasting and timed restricted eating.
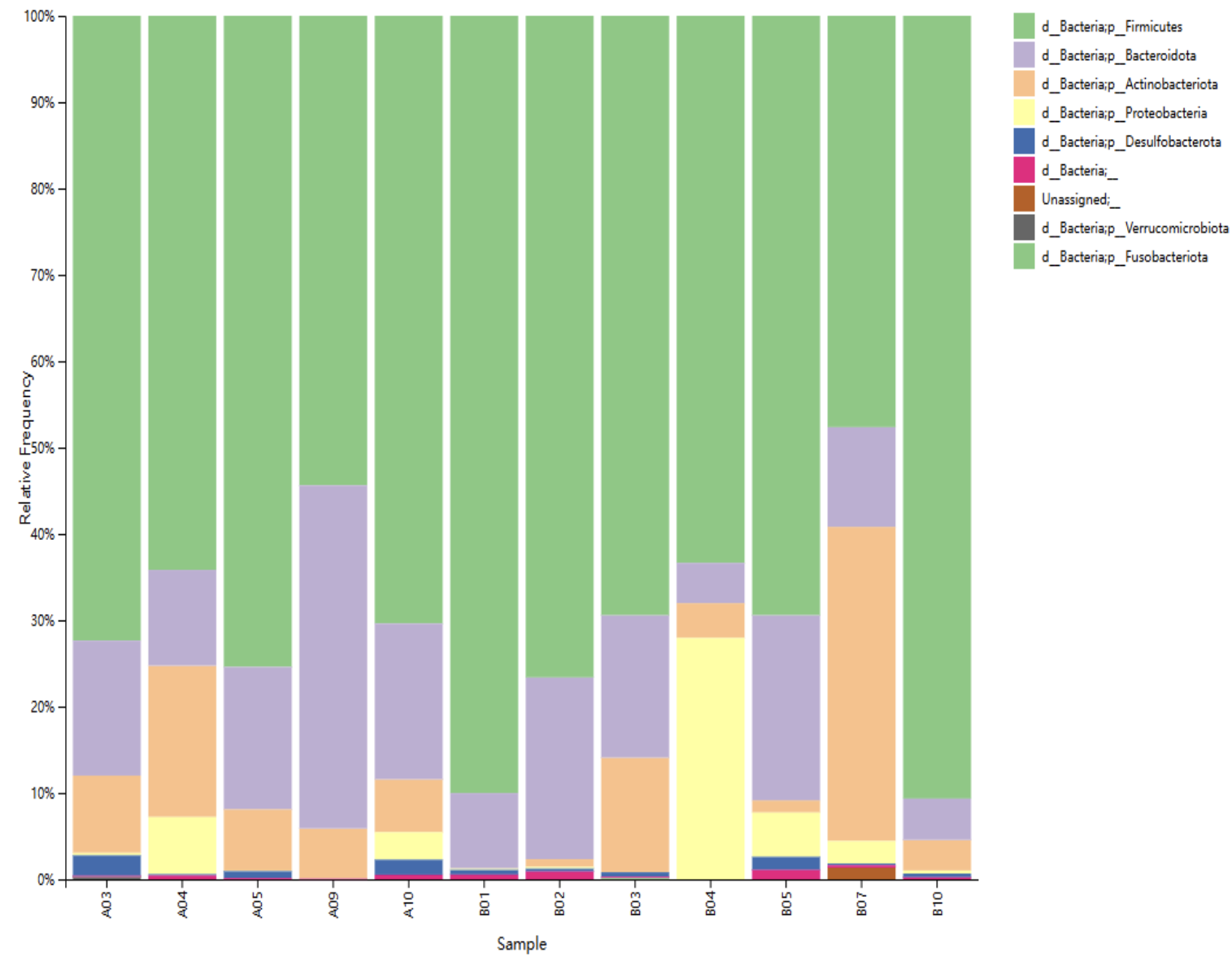
Figure: Figure 1: The taxonomy distribution of all samples at the Phylum classification level. Firmicutes and Bacteroidetes occupied most phyla in the gut microbiota, correlating with the green and purple colors as indicated by the legend on the top right.
Disclosures:
Karthic Drishna Perumal indicated no relevant financial relationships.
Frank Epitropoulos indicated no relevant financial relationships.
Sumit Sharma indicated no relevant financial relationships.
Tammy Aubel indicated no relevant financial relationships.
Ann Salvator indicated no relevant financial relationships.
Karthic Drishna Perumal, MD1, Frank Epitropoulos, MD2, Sumit Sharma, MD2, Tammy Aubel, BSN, RN2, Ann Salvator, MS2. P2679 - Intermittent Fasting, Gut Microbiome Composition, and Metabolic Health: A 3-Week Intervention in Patients With Prediabetes and Type 2 Diabetes Mellitus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

