Monday Poster Session
Category: Colorectal Cancer Prevention
P2637 - Non-Genetic Risk Factors for Early-Onset Colorectal Cancer: A Systematic Review and Meta-Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Camryn Kenkel, MD (she/her/hers)
NYU Grossman School of Medicine
New York, NY
Presenting Author(s)
Camryn Kenkel, MD1, David Kim, MD1, Jerry Kong, BS1, Shari Forbes, MD2, Angela Xue, MD2, Katherine L.. Stone, MD2, Anika Zaman, BS, MPH2, Leah Kim, MD2, Caitlin Plovnick, MS, BA2, Peter S. Liang, MD, MPH2
1NYU Grossman School of Medicine, New York, NY; 2NYU Langone Health, New York, NY
Introduction: Early-onset colorectal cancer (EOCRC), defined as colorectal cancer (CRC) diagnosed before age 50, is increasingly prevalent and has become a leading cause of cancer-related death among younger adults worldwide. We aimed to comprehensively identify non-genetic risk factors associated with EOCRC.
Methods: We conducted a systematic review and meta-analysis of observational studies that evaluated non-genetic EOCRC risk factors in individuals aged < 55 years. PubMed, EMBASE, Scopus, and the Cochrane Library were searched through November 2024. Manuscripts and abstracts published in English were included. We performed random-effects meta-analyses and evaluated heterogeneity and publication bias. Study quality was assessed using the Newcastle-Ottawa Scale. We conducted sensitivity analyses excluding abstracts, low-quality studies, studies with participants outside the ages of 18-49, and studies that adjusted for less than two variables.
Results: We screened 4224 studies, of which 91 were included in the systematic review and 79 were eligible for meta-analysis. The analysis included data from over 300,000 EOCRC cases. Figure 1 shows significant risk factors ordered by magnitude of association. These included demographic (family history of polyps and cancer, white race, unemployment), comorbidity (chronic kidney disease, inflammatory bowel disease, obesity, diabetes, hypertension, hyperglycemia, metabolic syndrome, abdominal obesity, non-alcoholic fatty liver disease, weight gain since age 18-20), and lifestyle/exposure (sugary beverages, fried food, sweet food, processed meat, alcohol, smoking, red meat) risk factors. Protective factors were calcium, higher education, statins, vitamin D, and vitamin supplementation. Variables with non-significant associations are shown in Figure 2. In sensitivity analyses, Asian race, no aspirin use, no NSAID use, and sedentary lifestyle became significant; calcium, education, red meat, processed meat, and weight gain became nonsignificant. Heterogeneity was high among variables with at least five studies, except for metabolic syndrome (I2 = 0.0). Most variables did not have evidence of publication bias.
Discussion: This study confirms known EOCRC risk factors and identifies additional risk factors that warrant further investigation. These findings provide a foundation for improving EOCRC risk assessment and developing targeted screening strategies to facilitate early detection in high-risk populations.
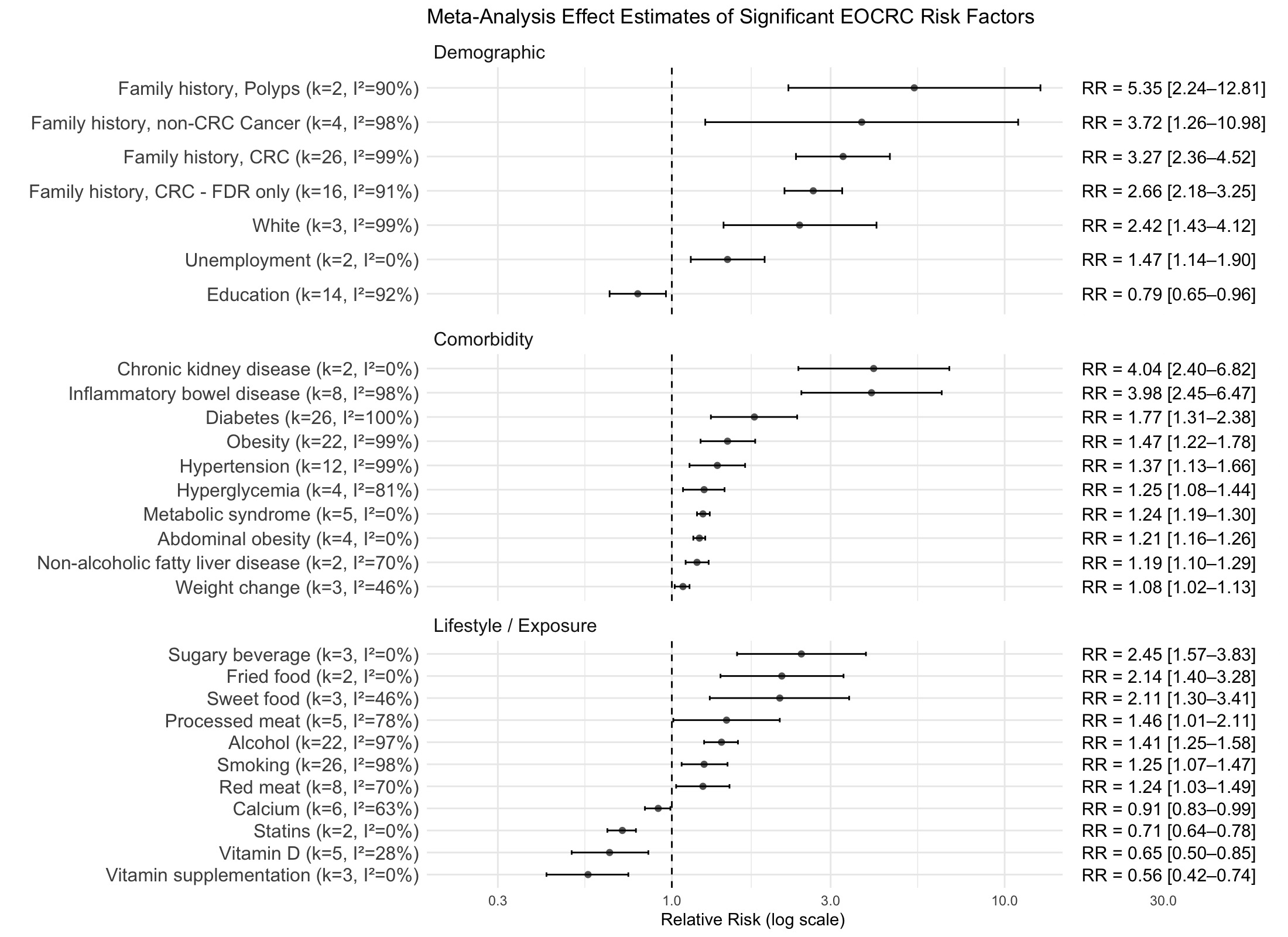
Figure: Figure 1. Effect estimates from meta-analysis of variables significantly associated with EOCRC. Abbreviations: CRC, colorectal cancer; FDR, first degree relative.
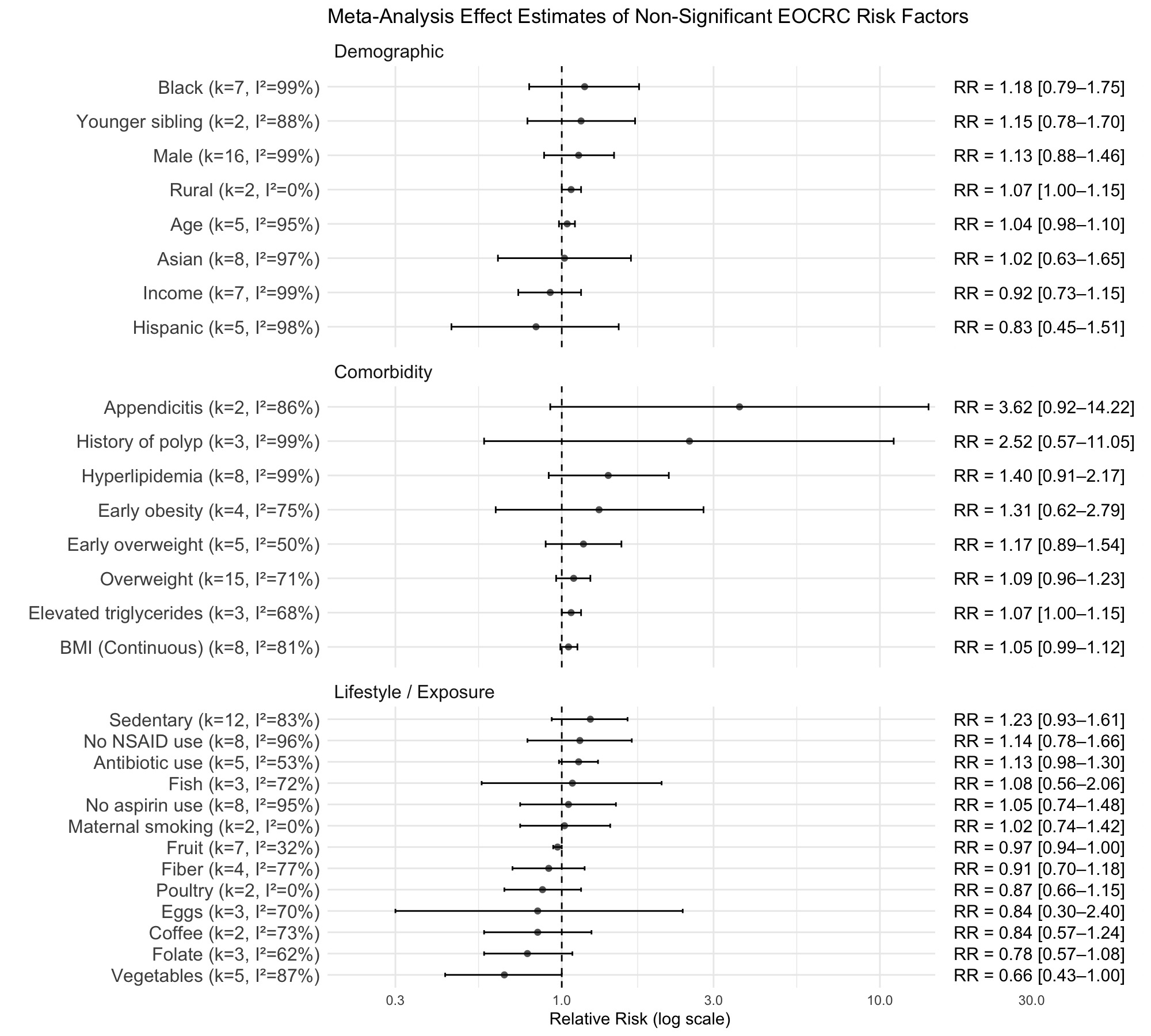
Figure: Figure 2. Effect estimates from meta-analysis of variables with non-significant associations with EOCRC. Abbreviations: BMI, body mass index; NSAID, non-steroidal anti-inflammatory drug.
Disclosures:
Camryn Kenkel indicated no relevant financial relationships.
David Kim indicated no relevant financial relationships.
Jerry Kong indicated no relevant financial relationships.
Shari Forbes indicated no relevant financial relationships.
Angela Xue indicated no relevant financial relationships.
Katherine Stone indicated no relevant financial relationships.
Anika Zaman indicated no relevant financial relationships.
Leah Kim indicated no relevant financial relationships.
Caitlin Plovnick indicated no relevant financial relationships.
Peter Liang: Freenome – Grant/Research Support. Guardant Health – Advisory Committee/Board Member. Natera – Advisory Committee/Board Member.
Camryn Kenkel, MD1, David Kim, MD1, Jerry Kong, BS1, Shari Forbes, MD2, Angela Xue, MD2, Katherine L.. Stone, MD2, Anika Zaman, BS, MPH2, Leah Kim, MD2, Caitlin Plovnick, MS, BA2, Peter S. Liang, MD, MPH2. P2637 - Non-Genetic Risk Factors for Early-Onset Colorectal Cancer: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1NYU Grossman School of Medicine, New York, NY; 2NYU Langone Health, New York, NY
Introduction: Early-onset colorectal cancer (EOCRC), defined as colorectal cancer (CRC) diagnosed before age 50, is increasingly prevalent and has become a leading cause of cancer-related death among younger adults worldwide. We aimed to comprehensively identify non-genetic risk factors associated with EOCRC.
Methods: We conducted a systematic review and meta-analysis of observational studies that evaluated non-genetic EOCRC risk factors in individuals aged < 55 years. PubMed, EMBASE, Scopus, and the Cochrane Library were searched through November 2024. Manuscripts and abstracts published in English were included. We performed random-effects meta-analyses and evaluated heterogeneity and publication bias. Study quality was assessed using the Newcastle-Ottawa Scale. We conducted sensitivity analyses excluding abstracts, low-quality studies, studies with participants outside the ages of 18-49, and studies that adjusted for less than two variables.
Results: We screened 4224 studies, of which 91 were included in the systematic review and 79 were eligible for meta-analysis. The analysis included data from over 300,000 EOCRC cases. Figure 1 shows significant risk factors ordered by magnitude of association. These included demographic (family history of polyps and cancer, white race, unemployment), comorbidity (chronic kidney disease, inflammatory bowel disease, obesity, diabetes, hypertension, hyperglycemia, metabolic syndrome, abdominal obesity, non-alcoholic fatty liver disease, weight gain since age 18-20), and lifestyle/exposure (sugary beverages, fried food, sweet food, processed meat, alcohol, smoking, red meat) risk factors. Protective factors were calcium, higher education, statins, vitamin D, and vitamin supplementation. Variables with non-significant associations are shown in Figure 2. In sensitivity analyses, Asian race, no aspirin use, no NSAID use, and sedentary lifestyle became significant; calcium, education, red meat, processed meat, and weight gain became nonsignificant. Heterogeneity was high among variables with at least five studies, except for metabolic syndrome (I2 = 0.0). Most variables did not have evidence of publication bias.
Discussion: This study confirms known EOCRC risk factors and identifies additional risk factors that warrant further investigation. These findings provide a foundation for improving EOCRC risk assessment and developing targeted screening strategies to facilitate early detection in high-risk populations.
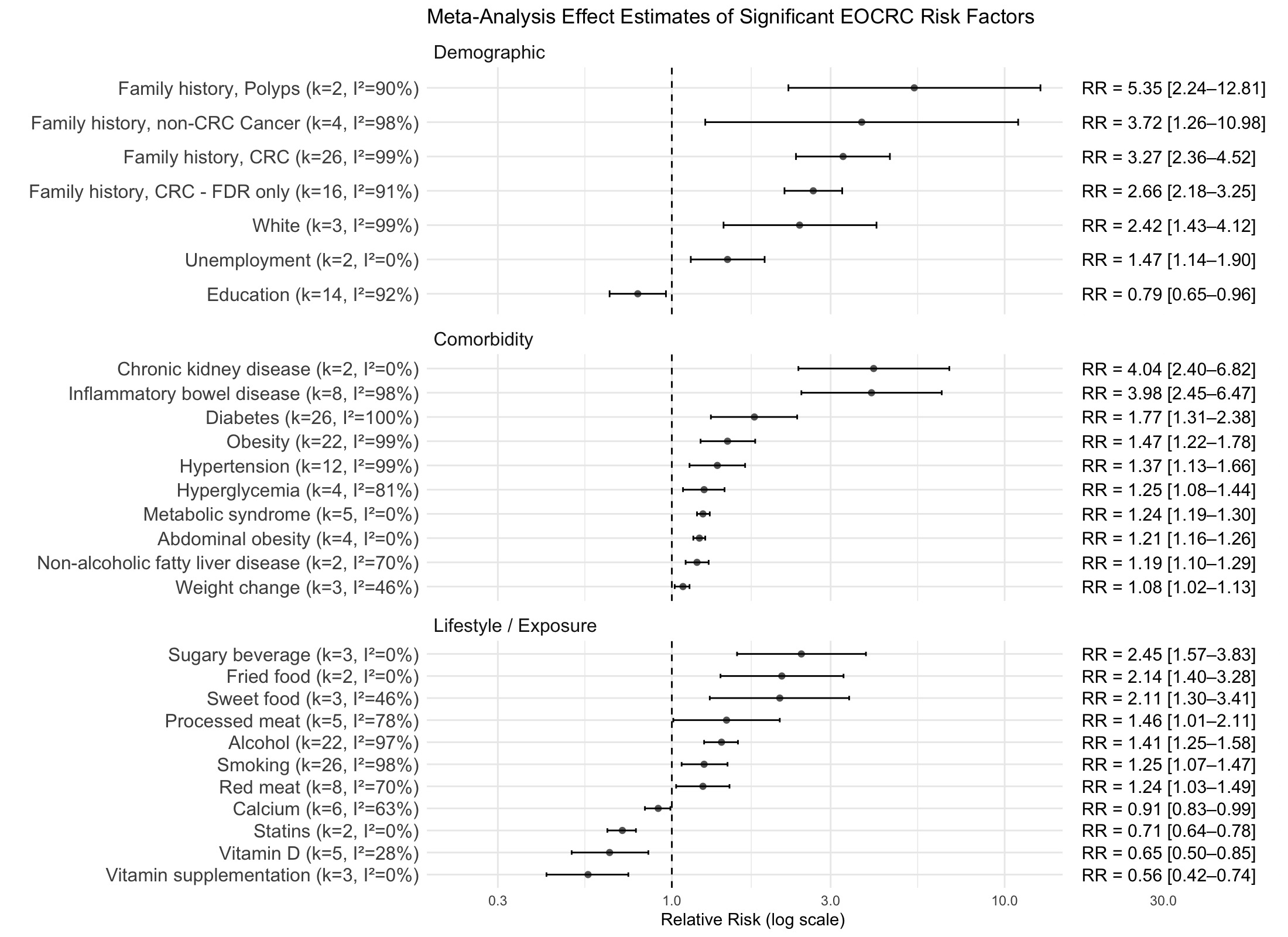
Figure: Figure 1. Effect estimates from meta-analysis of variables significantly associated with EOCRC. Abbreviations: CRC, colorectal cancer; FDR, first degree relative.
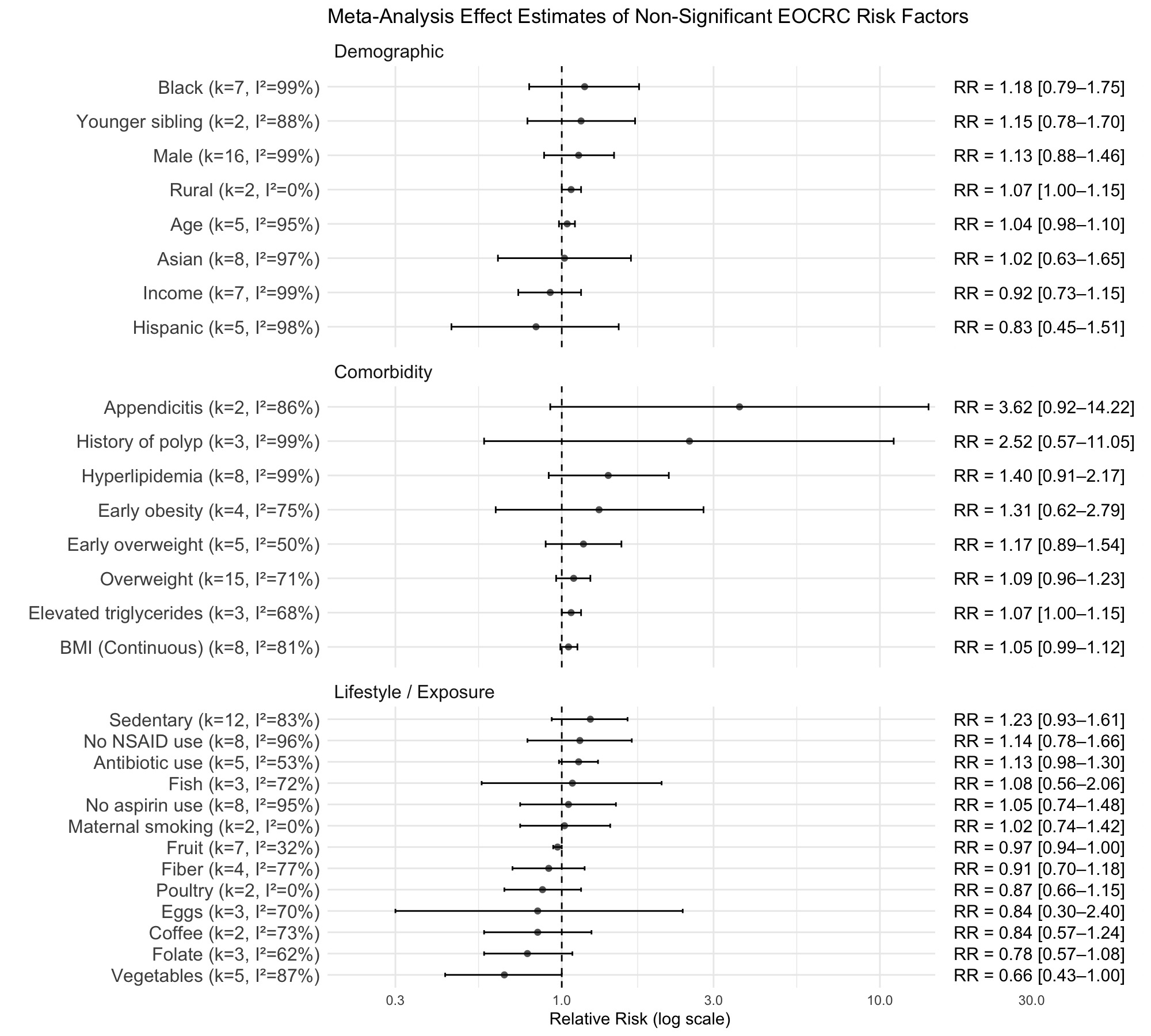
Figure: Figure 2. Effect estimates from meta-analysis of variables with non-significant associations with EOCRC. Abbreviations: BMI, body mass index; NSAID, non-steroidal anti-inflammatory drug.
Disclosures:
Camryn Kenkel indicated no relevant financial relationships.
David Kim indicated no relevant financial relationships.
Jerry Kong indicated no relevant financial relationships.
Shari Forbes indicated no relevant financial relationships.
Angela Xue indicated no relevant financial relationships.
Katherine Stone indicated no relevant financial relationships.
Anika Zaman indicated no relevant financial relationships.
Leah Kim indicated no relevant financial relationships.
Caitlin Plovnick indicated no relevant financial relationships.
Peter Liang: Freenome – Grant/Research Support. Guardant Health – Advisory Committee/Board Member. Natera – Advisory Committee/Board Member.
Camryn Kenkel, MD1, David Kim, MD1, Jerry Kong, BS1, Shari Forbes, MD2, Angela Xue, MD2, Katherine L.. Stone, MD2, Anika Zaman, BS, MPH2, Leah Kim, MD2, Caitlin Plovnick, MS, BA2, Peter S. Liang, MD, MPH2. P2637 - Non-Genetic Risk Factors for Early-Onset Colorectal Cancer: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
