Monday Poster Session
Category: Colorectal Cancer Prevention
P2636 - Poor Adherence to Repeat Quality Colonoscopy After Inadequate Bowel Preparation: Analysis From GIQuIC Registry
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

David A. Johnson, MD, MACG
Eastern Virginia Medical School
Norfolk, VA
Presenting Author(s)
David A. Johnson, MD, MACG1, Jennifer Holub, MPH2, Aasma Shaukat, MD, MPH, FACG3
1Eastern Virginia Medical School, Norfolk, VA; 2GIQuIC, Bethesda, MD; 3NYU Grossman School of Medicine, Division of Gastroenterology and Hepatology, New York, NY
Introduction: Adequate bowel preparation (ABP) is essential to optimize quality colonoscopy (colo) related outcomes. The USMSTF 2025 guideline recommends rates >90% for ABP. Inadequate bowel preps (IBPs) important implications including: direct/indirect related costs, delayed or missed diagnosis, loss of patient willingness to repeat prep/exam and negative public messaging which may deter other patients from undergoing colo. The guideline recommends colo should be repeated within 1 yr after the initial IAP- albeit experts agree to do sooner if significant pathology identified.
Methods: We used colos from GIQUIC registry between 2011-2022, to study IAP rates and associated demographics with repeat colos after IAP and adherence to quality recommendations for repeat colo < 1 (primary analysis). Inclusion criteria were colos with any indication (screen/surveillance/diagnostic) and MD recommendation repeat < 1 yr. Multivariate logistic regression models were used to identify factors, covariates were kept if p ≤ 0.20 evaluating 2 outcomes: repeat colonoscopy after IBP < 1(quality) and ≤5yrs.
Results: From 16,747,770 colos, IAP was reported in 920,551. Rates of IBPs declined initially from 2011-14 (10.7-5.9%) but plateaued 2015-22 (5.2-5.5%). Primary analysis, limited to 298,148 IAPs, showed adherence to repeat colo was low across all indications (Table 1), without demographic differences, even if high risk pathology on index IAP (Table 1). Tine trend analysis showed significant worsening for compliance with guidelines for repeat colo across all indications (p< 0.001). Men were less likely to repeat colo after IAP in <1 year, (OR 0.93 95% CI 0.91-0.95) and less likely to have follow-up in ≤5 years (OR 0.91 95% CI: 0.90-0.93) compared with women. (Table 2) Rates of IAP on repeat colo were high (19-24.4 %) and significantly worse compared to diagnostics.
Repeat IAP 2nd exam Screening Surveillance Diagnostic
N repeat totals 48,222 38,761 37,075
N and 2nd IAP (%) 9,177 (19.0) 7,490 (19.3) 9,053 (24.4) p < .0001
Discussion: Adherence to national quality guideline recommendations for repeat colos following IAP across all categories was low, even if high risk pathology was identified. Rates of IAP on repeat colo were high. Interventions such as navigation strategies to optimize ABP and in particular to address appropriate follow up of IAP, are critically needed to optimize quality of colo.
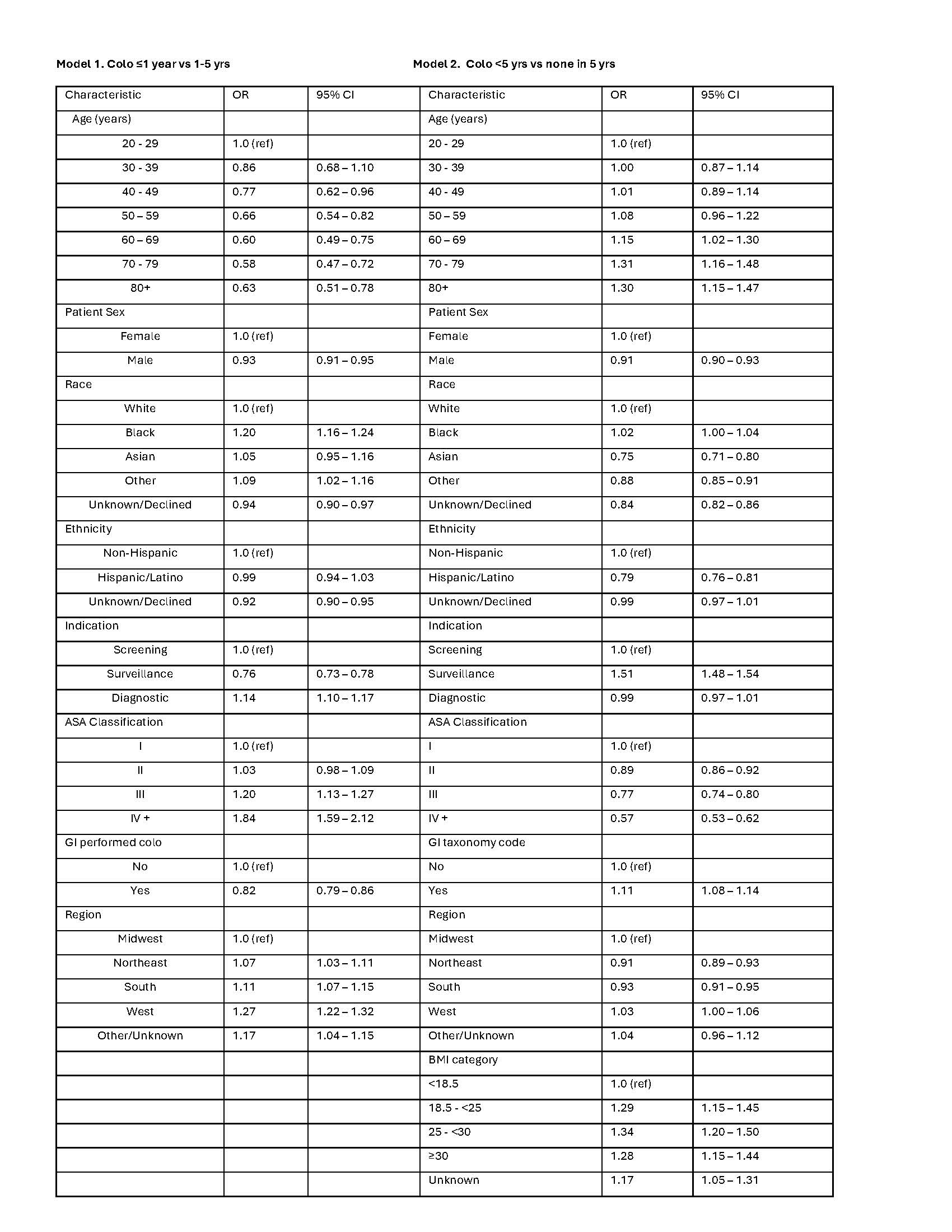
Figure: Table 1. Repeat colonoscopy timelines and demographic information
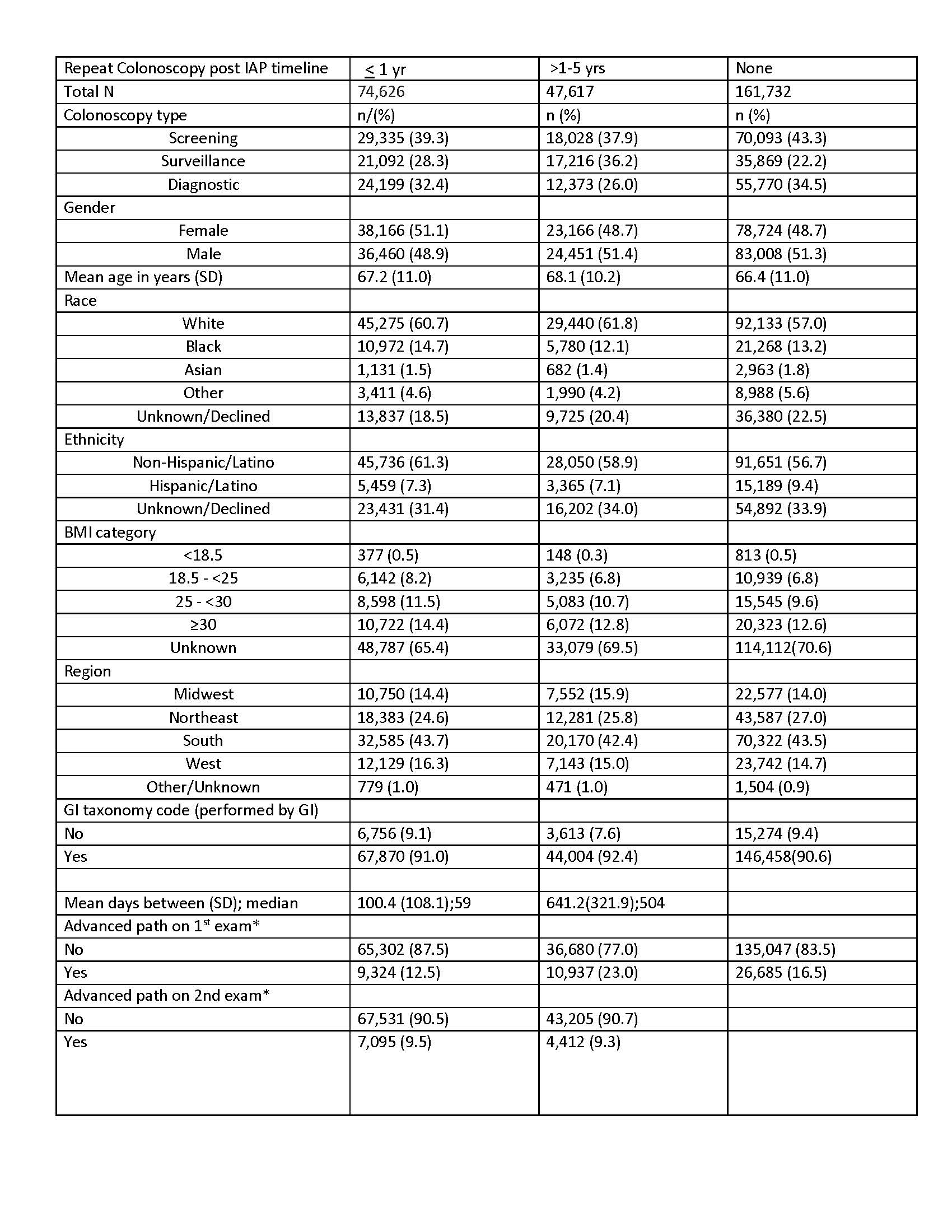
Figure: Table 2. Logistic regression models of outcomes of repeat colos post IAP
Disclosures:
David Johnson: Isothrive – Grant/Research Support. Sabala – Grant/Research Support.
Jennifer Holub indicated no relevant financial relationships.
Aasma Shaukat: Freenome inc – Consultant.
David A. Johnson, MD, MACG1, Jennifer Holub, MPH2, Aasma Shaukat, MD, MPH, FACG3. P2636 - Poor Adherence to Repeat Quality Colonoscopy After Inadequate Bowel Preparation: Analysis From GIQuIC Registry, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Eastern Virginia Medical School, Norfolk, VA; 2GIQuIC, Bethesda, MD; 3NYU Grossman School of Medicine, Division of Gastroenterology and Hepatology, New York, NY
Introduction: Adequate bowel preparation (ABP) is essential to optimize quality colonoscopy (colo) related outcomes. The USMSTF 2025 guideline recommends rates >90% for ABP. Inadequate bowel preps (IBPs) important implications including: direct/indirect related costs, delayed or missed diagnosis, loss of patient willingness to repeat prep/exam and negative public messaging which may deter other patients from undergoing colo. The guideline recommends colo should be repeated within 1 yr after the initial IAP- albeit experts agree to do sooner if significant pathology identified.
Methods: We used colos from GIQUIC registry between 2011-2022, to study IAP rates and associated demographics with repeat colos after IAP and adherence to quality recommendations for repeat colo < 1 (primary analysis). Inclusion criteria were colos with any indication (screen/surveillance/diagnostic) and MD recommendation repeat < 1 yr. Multivariate logistic regression models were used to identify factors, covariates were kept if p ≤ 0.20 evaluating 2 outcomes: repeat colonoscopy after IBP < 1(quality) and ≤5yrs.
Results: From 16,747,770 colos, IAP was reported in 920,551. Rates of IBPs declined initially from 2011-14 (10.7-5.9%) but plateaued 2015-22 (5.2-5.5%). Primary analysis, limited to 298,148 IAPs, showed adherence to repeat colo was low across all indications (Table 1), without demographic differences, even if high risk pathology on index IAP (Table 1). Tine trend analysis showed significant worsening for compliance with guidelines for repeat colo across all indications (p< 0.001). Men were less likely to repeat colo after IAP in <1 year, (OR 0.93 95% CI 0.91-0.95) and less likely to have follow-up in ≤5 years (OR 0.91 95% CI: 0.90-0.93) compared with women. (Table 2) Rates of IAP on repeat colo were high (19-24.4 %) and significantly worse compared to diagnostics.
Repeat IAP 2nd exam Screening Surveillance Diagnostic
N repeat totals 48,222 38,761 37,075
N and 2nd IAP (%) 9,177 (19.0) 7,490 (19.3) 9,053 (24.4) p < .0001
Discussion: Adherence to national quality guideline recommendations for repeat colos following IAP across all categories was low, even if high risk pathology was identified. Rates of IAP on repeat colo were high. Interventions such as navigation strategies to optimize ABP and in particular to address appropriate follow up of IAP, are critically needed to optimize quality of colo.
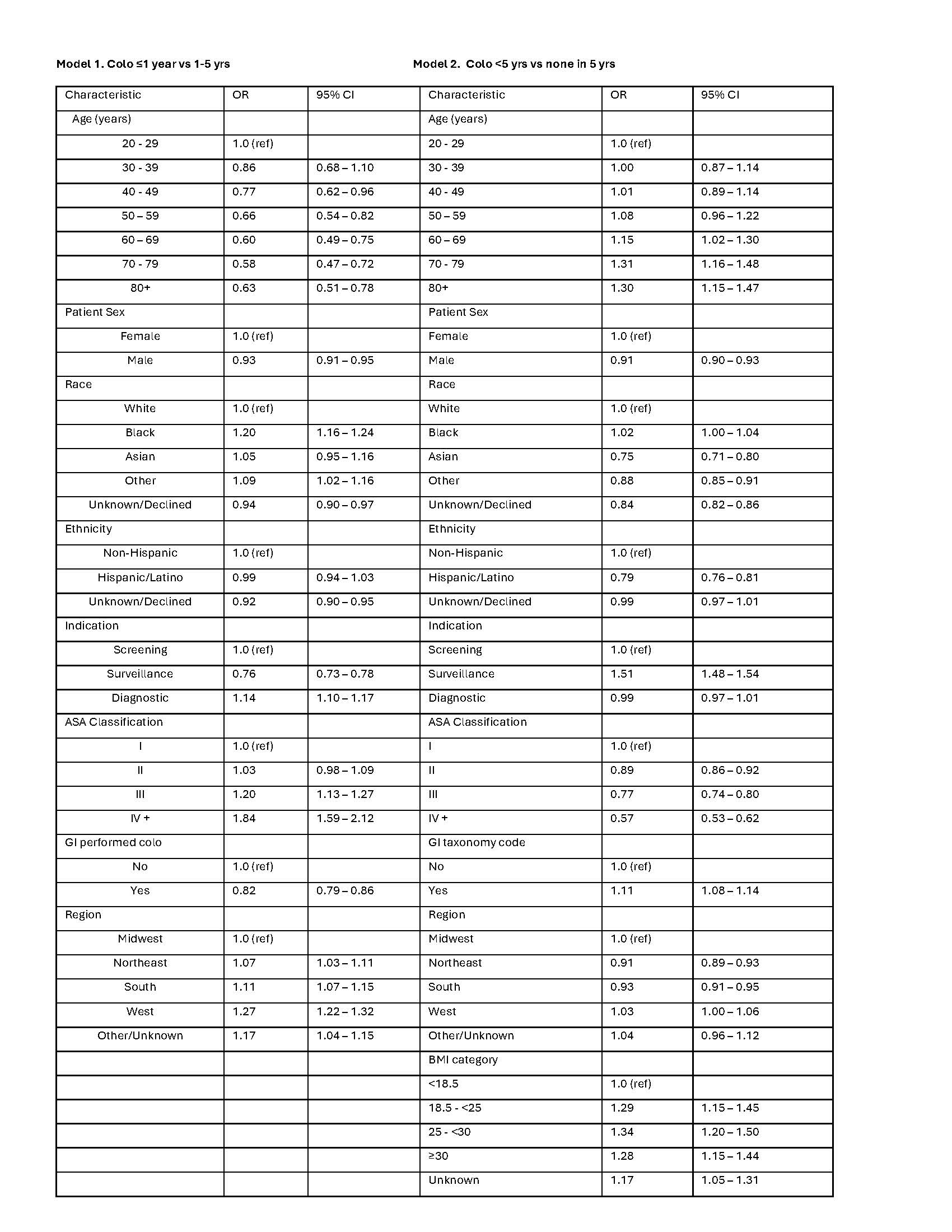
Figure: Table 1. Repeat colonoscopy timelines and demographic information
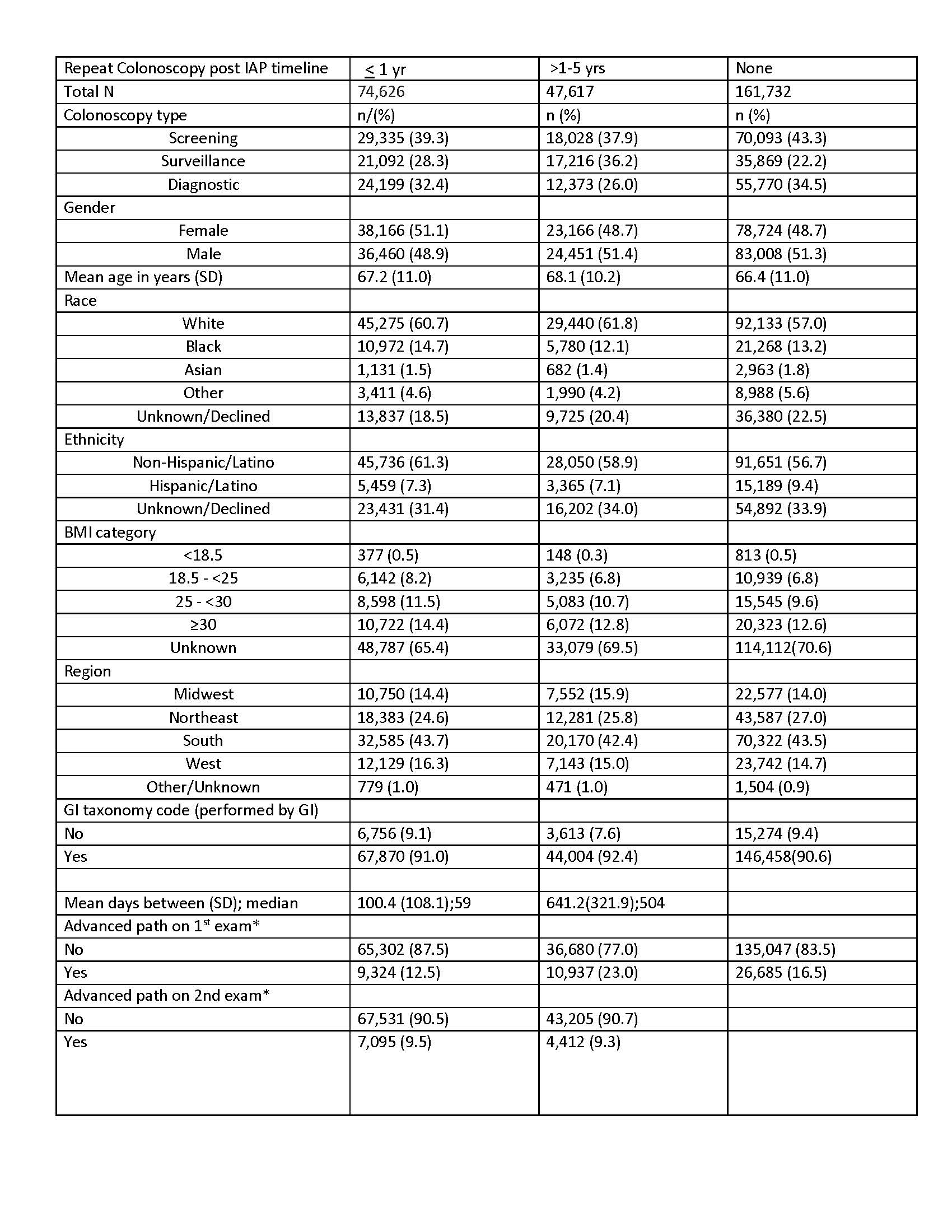
Figure: Table 2. Logistic regression models of outcomes of repeat colos post IAP
Disclosures:
David Johnson: Isothrive – Grant/Research Support. Sabala – Grant/Research Support.
Jennifer Holub indicated no relevant financial relationships.
Aasma Shaukat: Freenome inc – Consultant.
David A. Johnson, MD, MACG1, Jennifer Holub, MPH2, Aasma Shaukat, MD, MPH, FACG3. P2636 - Poor Adherence to Repeat Quality Colonoscopy After Inadequate Bowel Preparation: Analysis From GIQuIC Registry, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
