Monday Poster Session
Category: Colorectal Cancer Prevention
P2628 - Food Insecurity at the Zip Code Level Is Independently Associated With Delayed Colorectal Cancer Diagnosis: A Geospatial Analysis of SEER Data
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ashish Sharma, MD (he/him/his)
University of Connecticut-Hartford
Rocky Hill, CT
Presenting Author(s)
Harendra Kumar, MBBS1, Ashish Sharma, MD2, Angad Tiwari, MBBS3, Shea-Lee Godin, MD4, Mohit Kale, MD5
1Dow University of Health Sciences, Karachi, Sindh, Pakistan; 2University of Connecticut-Hartford, Hartford, CT; 3Maharani Laxmi Bai Medical College, Ghaziabad, Uttar Pradesh, India; 4University of Connecticut Health, Farmington, CT; 5Landmark Medical Center, Woonsocket, RI
Introduction: Delayed diagnosis of colorectal cancer (CRC) has a negative influence on prognosis and increases the treatment burden. While socioeconomic disparities are well-established in cancer treatment, the precise significance of local food insecurity—a measure of nutritional and economic deprivation—has not been well examined. This research uses the geographical interconnectedness of and SEER cancer registry data to assess the impact of food insecurity on stage at CRC diagnosis.
Methods: We conducted a retrospective cohort study using SEER 18 registries (2010-2019) on adult patients (aged ≥18) diagnosed with incident colorectal cancer (ICD-O-3 codes: C18.0-C20.9). Using U.S. Census data, geographical relationships were found between patient zip codes and USDA-defined food insecurity rates. The primary outcome was a diagnosis of regional or distant stage (vs. localized), as defined by SEER Summary Stage. Multivariable logistic regression was used to examine the relationship between food insecurity quartile and late-stage diagnosis after controlling age, gender, race/ethnicity, insurance status, and urban/rural classification. Spatial autocorrelation and hotspot studies were carried out using ArcGIS Pro and SaTScan.
Results: Among 221,380 CRC patients with geocoded zip code data, those in the highest quartile of food poverty had a significantly higher risk of late-stage diagnosis (61.2%) than those in the lowest quartile (48.7%) (p < 0.001). After adjustment, residence in a high-food insecurity region was independently associated with higher chances of late-stage CRC diagnosis (aOR: 1.42; 95% CI: 1.36-1.48; p < 0.001). Spatial cluster analysis revealed significant hotspots in the southern states and the Midwest. The correlation was clear across racial and insurance demographics.
Discussion: Food poverty at the zip code level is a strong, independent predictor of delayed colorectal cancer detection in the United States. These results the need to include socioeconomic variables, including food availability, in cancer prevention and early detection efforts.
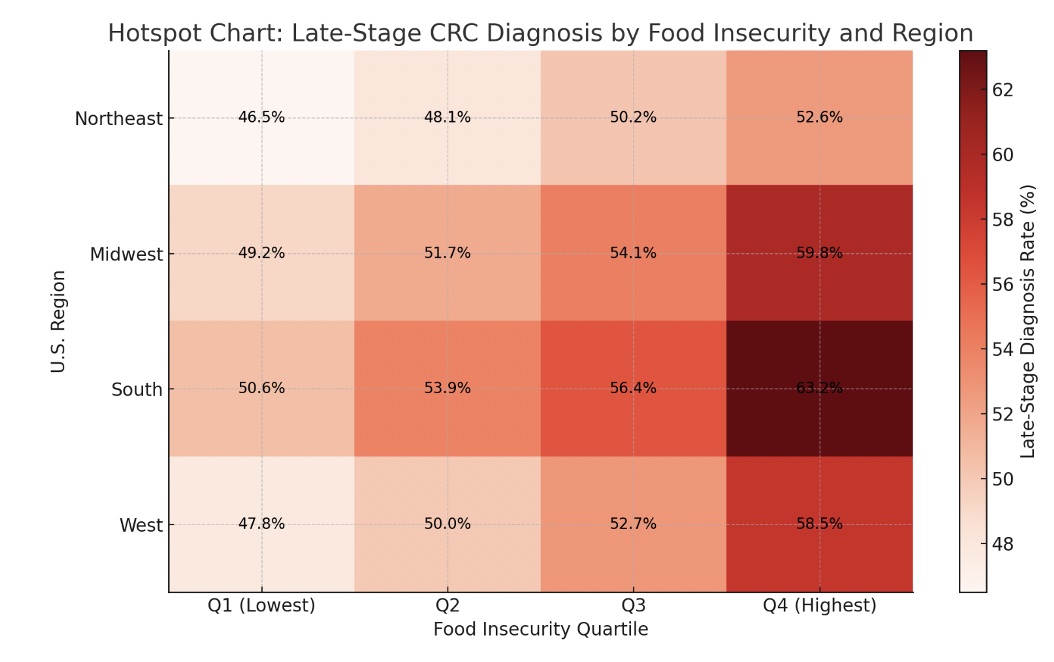
Figure: Figure 1: Hotspot Chart: Late-Stage CRC Diagnosis by Food Insecurity and Region
Disclosures:
Harendra Kumar indicated no relevant financial relationships.
Ashish Sharma indicated no relevant financial relationships.
Angad Tiwari indicated no relevant financial relationships.
Shea-Lee Godin indicated no relevant financial relationships.
Mohit Kale indicated no relevant financial relationships.
Harendra Kumar, MBBS1, Ashish Sharma, MD2, Angad Tiwari, MBBS3, Shea-Lee Godin, MD4, Mohit Kale, MD5. P2628 - Food Insecurity at the Zip Code Level Is Independently Associated With Delayed Colorectal Cancer Diagnosis: A Geospatial Analysis of SEER Data, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Dow University of Health Sciences, Karachi, Sindh, Pakistan; 2University of Connecticut-Hartford, Hartford, CT; 3Maharani Laxmi Bai Medical College, Ghaziabad, Uttar Pradesh, India; 4University of Connecticut Health, Farmington, CT; 5Landmark Medical Center, Woonsocket, RI
Introduction: Delayed diagnosis of colorectal cancer (CRC) has a negative influence on prognosis and increases the treatment burden. While socioeconomic disparities are well-established in cancer treatment, the precise significance of local food insecurity—a measure of nutritional and economic deprivation—has not been well examined. This research uses the geographical interconnectedness of and SEER cancer registry data to assess the impact of food insecurity on stage at CRC diagnosis.
Methods: We conducted a retrospective cohort study using SEER 18 registries (2010-2019) on adult patients (aged ≥18) diagnosed with incident colorectal cancer (ICD-O-3 codes: C18.0-C20.9). Using U.S. Census data, geographical relationships were found between patient zip codes and USDA-defined food insecurity rates. The primary outcome was a diagnosis of regional or distant stage (vs. localized), as defined by SEER Summary Stage. Multivariable logistic regression was used to examine the relationship between food insecurity quartile and late-stage diagnosis after controlling age, gender, race/ethnicity, insurance status, and urban/rural classification. Spatial autocorrelation and hotspot studies were carried out using ArcGIS Pro and SaTScan.
Results: Among 221,380 CRC patients with geocoded zip code data, those in the highest quartile of food poverty had a significantly higher risk of late-stage diagnosis (61.2%) than those in the lowest quartile (48.7%) (p < 0.001). After adjustment, residence in a high-food insecurity region was independently associated with higher chances of late-stage CRC diagnosis (aOR: 1.42; 95% CI: 1.36-1.48; p < 0.001). Spatial cluster analysis revealed significant hotspots in the southern states and the Midwest. The correlation was clear across racial and insurance demographics.
Discussion: Food poverty at the zip code level is a strong, independent predictor of delayed colorectal cancer detection in the United States. These results the need to include socioeconomic variables, including food availability, in cancer prevention and early detection efforts.
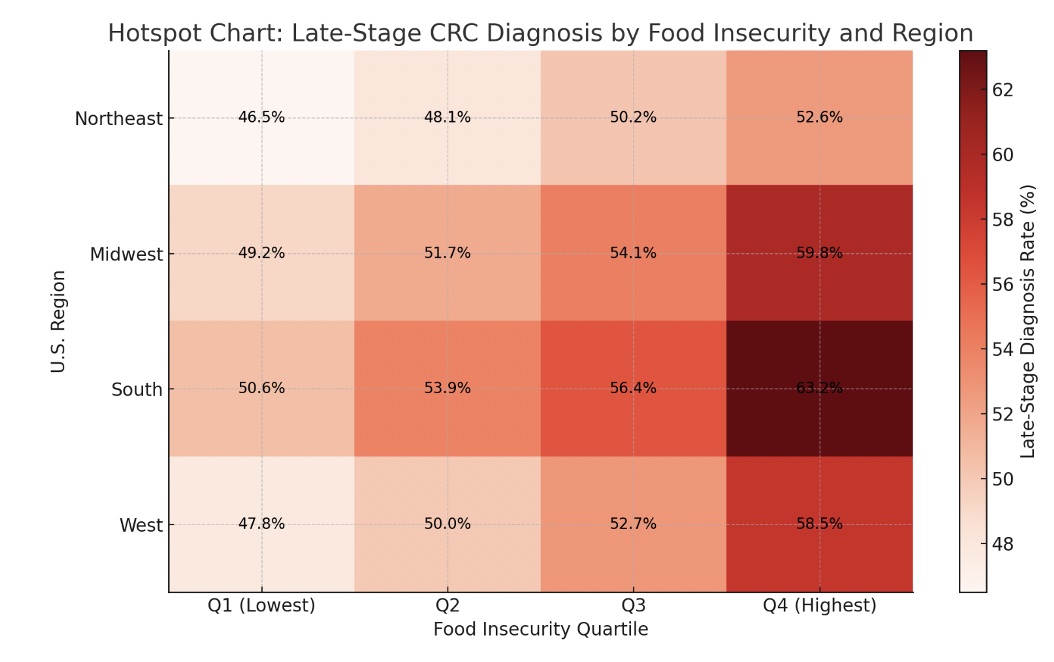
Figure: Figure 1: Hotspot Chart: Late-Stage CRC Diagnosis by Food Insecurity and Region
Disclosures:
Harendra Kumar indicated no relevant financial relationships.
Ashish Sharma indicated no relevant financial relationships.
Angad Tiwari indicated no relevant financial relationships.
Shea-Lee Godin indicated no relevant financial relationships.
Mohit Kale indicated no relevant financial relationships.
Harendra Kumar, MBBS1, Ashish Sharma, MD2, Angad Tiwari, MBBS3, Shea-Lee Godin, MD4, Mohit Kale, MD5. P2628 - Food Insecurity at the Zip Code Level Is Independently Associated With Delayed Colorectal Cancer Diagnosis: A Geospatial Analysis of SEER Data, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
