Monday Poster Session
Category: Colon
P2590 - An Unusual Culprit: CMV Colitis-Induced Protein-Losing Enteropathy in an Immunocompetent Adult

Sanjna Shelukar, MD
Thomas Jefferson University Hospital
Philadelphia, PA
Presenting Author(s)
Thomas Jefferson University Hospital, Philadelphia, PA
Introduction:
Protein-losing enteropathy (PLE) is excessive protein loss via the gastrointestinal tract causing diarrhea, hypoalbuminemia, and fluid overload. Diagnosis is supported by elevated stool alpha-1 antitrypsin (A1AT). The extensive differential diagnosis includes infections such as Whipple’s disease and opportunistic pathogens (Figure 1). We present a rare case of cytomegalovirus (CMV) colitis causing severe PLE in an immunocompetent patient.
Case Description/
Methods:
An 80-year-old male presented to the hospital with 5 non-bloody diarrheal movements daily, anasarca, and labs notable for serum albumin of 1.6 g/dL and spot stool A1AT of 120 mg/dL (normal < 55 mg/dL). Stool studies (ova & parasites, Giardia antigen, bacterial & viral PCR) and celiac serologies were negative. Imaging showed distal ileum and ascending colon thickening. Colonoscopy (day 7) revealed patchy discontinuous ulcerations in the cecum, ascending colon, and terminal ileum. Biopsies confirmed CMV colitis. Upper endoscopy showed mild duodenal villous blunting. IV ganciclovir (2.5 mg/kg/day) was started and continued for 4 weeks, and he was discharged.
Two weeks post-discharge, he was re-hospitalized for large pleural effusions requiring weekly thoracenteses and chest tube placement. Repeat stool testing on day 2 was positive for Giardia antigen. Despite treatment with metronidazole, there was no clinical improvement over the next 6 weeks. Additional evaluation excluded alternate causes of PLE (Figure 1) while the patient remained hospitalized.
CT enterography (day 31) showed persistent ileocolonic inflammation. On day 44, IV methylprednisolone (20 mg twice daily) and a second course of ganciclovir were started. Within 1 week, bowel frequency decreased to 1-2/day, pleural output declined, and chest tube was removed.
Repeat colonoscopy (day 56) to evaluate for coexisting disease showed patchy ulcerations in the cecum and terminal ileum; biopsies reconfirmed CMV colitis. He was discharged on a steroid taper and valganciclovir for 6 weeks. Two months post-treatment, he had 1 daily formed stool, weight gain, and albumin rose to 3.2 g/dL.
Discussion:
This case highlights CMV colitis as a rare cause of severe PLE in an immunocompetent patient. Decline despite antivirals prompted evaluation for concomitant causes. Findings on repeat colonoscopy, and rapid and sustained clinical recovery with combined antiviral and steroid therapy, supports CMV as the etiology and underscores the need for reassessment when disease course is atypical.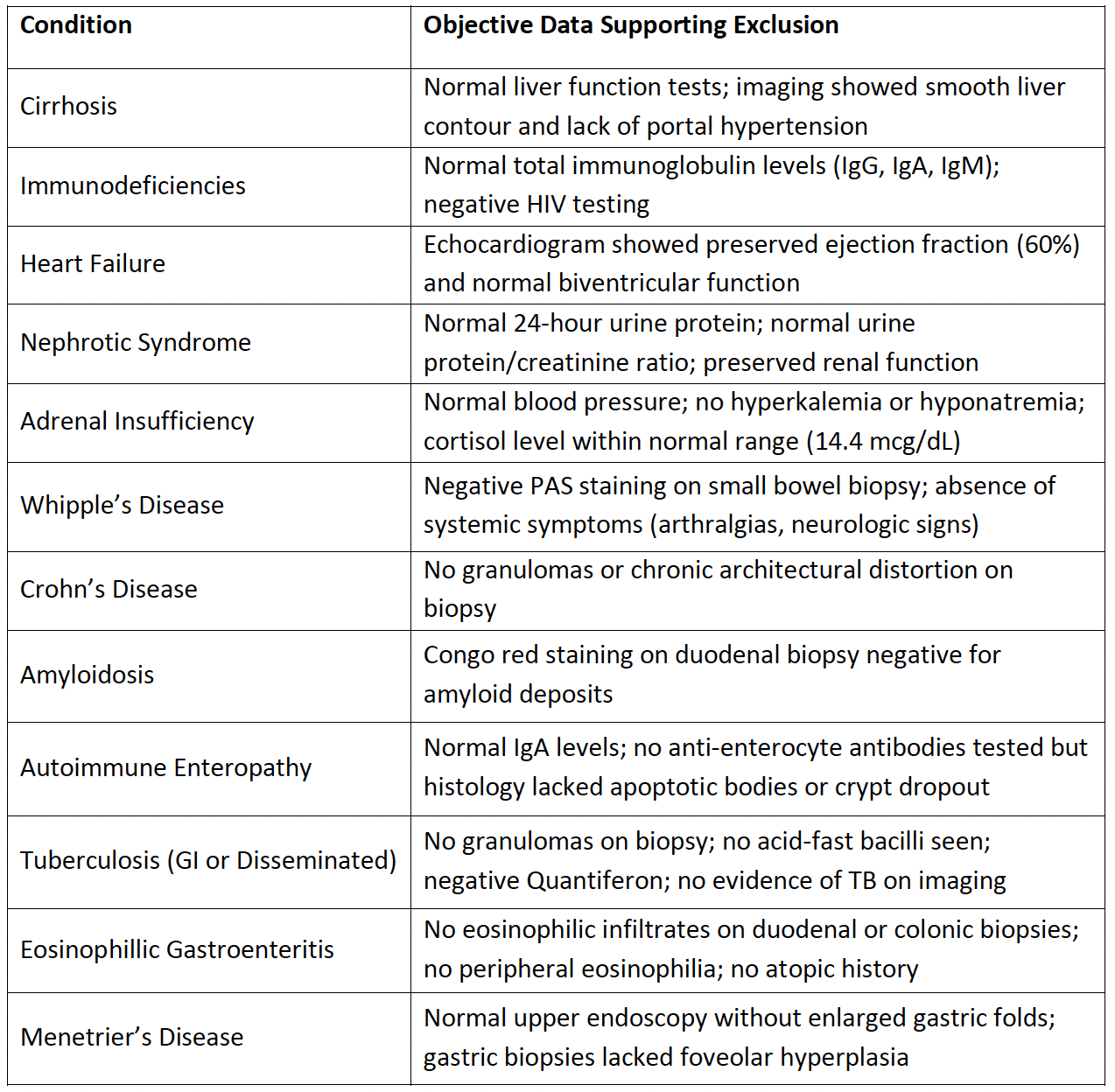
Figure: Figure 1: Alternate Etiologies Considered and Excluded
Disclosures:
Sanjna Shelukar indicated no relevant financial relationships.
Nehar Damle indicated no relevant financial relationships.
Leanna Rucker indicated no relevant financial relationships.
Maria Winte indicated no relevant financial relationships.
David Kastenberg indicated no relevant financial relationships.
Sanjna Shelukar, MD, Nehar Damle, MD, Leanna Rucker, MD, Maria Winte, MD, David Kastenberg, MD. P2590 - An Unusual Culprit: CMV Colitis-Induced Protein-Losing Enteropathy in an Immunocompetent Adult, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
